Nationwide pulmonary function test rates in South Korean asthma patients
Introduction
Asthma is a chronic inflammatory airway disease characterised by variable respiratory symptoms, such as cough, wheeze, dyspnoea, and chest discomfort, in addition to variable expiratory airflow limitation (1). The socioeconomic burden of asthma has become so substantial that it is now considered a major public health issue (2). In the US, around 26 million asthma patients are treated annually, at a cost of $50 billion (3). Consequently, there has been worldwide effort to improve asthma management; however, asthma care quality has been unsatisfactory in several aspects of diagnosis, assessment, and treatment (4-6).
A pulmonary function test (PFT) is one of the best methods for diagnosis and assessment of asthma (1). Global Initiative for Asthma guidelines recommend that a PFT be performed at diagnosis or initiation of treatment, 3–6 months after starting asthma control treatment, and periodically as treatment continues. This process is important to assess asthma control status and evaluate the risk of asthma exacerbation. However, many researchers have reported that the PFT performance rate is considerably lower than would be expected if guidelines were followed, although specific rates vary among studies (4,7,8). Underutilization of PFTs may be caused by several factors, including a lack of equipment at health care facilities, indifference of doctors, and low compliance in some asthma patients. Further studies are required to understand the current status of PFT performance in a real-world context.
In the Republic of Korea, almost the entire population has health insurance through National Health Insurance (NHI), National Medical Aid (NMA), or Korea Veterans Health Service (KVHS) (9). When healthcare centres file claims for medical expenses, insurance reimbursement is approved by the Health Insurance Review and Assessment Service (HIRA), which assesses the quality of the medical practice. HIRA collects patient clinical data through insurance claims for several purposes, including healthcare big data analysis. Using this database, we can assess current PFT performance status in almost every asthma patient who visited a healthcare clinic in the Republic of Korea during the study period.
The aim of this study was to evaluate the current status of PFT performance in the Republic of Korea. We categorized performance rate by type of health care institution, medical specialty, and general characteristics of patients. We also studied differences in possession rates of PFT equipment by type of health care institution.
Methods
Data source and selection
We analysed a nationwide HIRA quality assessment database to investigate the current status of PFT performance in the Republic of Korea. Quality assessment was performed for medical institutions that treated more than nine asthma patients within a year. We extracted medical information of asthma patients from July 2013 to June 2014. This information included age, gender, medical institution, International Statistical Classification of Diseases and Related Health Problems, 10th revision (ICD-10) codes, PFT performance, and possession of PFT equipment. Patient inclusion criteria were (I) age >15 years; (II) primary or first secondary diagnosis of asthma by ICD-10 code; and (III) either prescription of asthma medication (corticosteroids, leukotriene receptor antagonists, long acting β2-agonists, short acting β2-agonists, anticholinergics, or xanthine derivatives) from an outpatient clinic more than once per year, or evidence in patient’s admission history of asthma medication having been prescribed previously. Patients with an ICD-10 code that forbids PFT performance per guidelines, such as dementia or various forms of paralysis, were excluded.
Medical institutions
Medical institutions were categorized as tertiary hospitals, general hospitals, convalescent hospitals, primary health clinics, public health centres, branch offices of a public health centre, or county hospitals. Clinics that did not fit in these categories, such as facilities practicing traditional medicine, dental clinics, and maternity clinics, were excluded. Medical institutions were also categorized by specialty: internal medicine, general practice, otorhinolaryngology, paediatrics, family medicine, and other.
Assessment of PFT performance
The PFT performance rate was defined as the ratio of the number of asthma patients who received a PFT to the number of asthma patients enrolled in this study during a one-year period (from July 2013 to June 2014). PFT types included spirometry with/without flow-volume curve, cardiopulmonary exercise test, peak expiratory flow rate test, and the bronchial provocation test.
The PFT performance rate was calculated for every medical institution included in this study. The rates were then compared among institution types and medical specialties. We also analysed the number of medical institutions at each PFT performance rate level. The PFT performance rate was also analysed by patient gender, age, and insurance type (NHI, NMA, or KVHS).
Possession rates of PFT equipment were assessed by type of medical institution. Performance rates of each type of PFT were also evaluated.
Ethics
This study was approved by the ethics committee of Seoul St. Mary’s Hospital (KIRB-0E482-001). The requirement for informed consent from the patients was waived due to the retrospective nature of this study and anonymity of the data.
Statistical analysis
Chi-square or Fisher’s exact tests were used to compare PFT performance rates according to sex, age, and insurance type. The Mantel-Haenszel chi-squared test was used to analyse correlations between PFT rate and type of insurance or age group. A P value <0.05 was considered statistically significant for all analyses. Statistical analyses were conducted using SAS 9.2 software (SAS Institute, Cary, NC, USA).
Results
Subjects for evaluation
Of a total of 33,341 medical institutions in South Korea, 16,804 (50.40%) underwent quality assessment by HIRA. Of these, 14,745 (87.75%) were primary health clinics, 43 (0.26%) were tertiary hospitals, and 280 (1.67%) were general hospitals. Primary health clinics treated an average of fewer than 10 asthma patients at each of 5,778 (38.19% of all clinics) locations; however, tertiary hospitals treated an average of more than 500 asthma patients at each of 33 (76.74% of all tertiary hospitals) locations.
This database included 831,613 patients. Of these, 686,063 (82.50%) were treated only at primary health clinics, whereas 43,471 (5.23%) were treated at tertiary hospitals, and 83,194 (10.00%) were treated at general hospitals.
Assessment of PFT performance
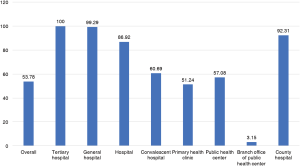
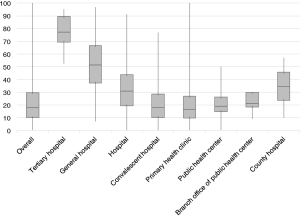
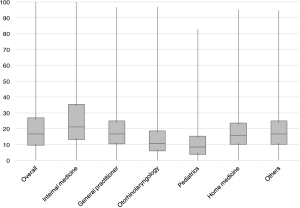
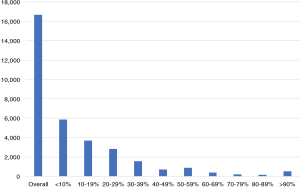
We analysed the PFT performance rate by medical institution type (Figure 1). The average PFT performance rate at tertiary hospitals was 78.00%, with a relatively low standard deviation (SD =11.96). In contrast, primary health clinics had an average PFT performance rate of 20.87% with a SD of 16.68. The mean PFT performance rate for all medical institutions was 22.67%. Analysis of PFT performance by specialty found that departments of internal medicine performed PFTs most frequently, at an average of 26.92% (Figure 2). The specialty with the lowest performance rate was paediatrics (10.77%), which was lower even than general practitioners (19.21%). In all, more than half of medical institutions performed PFTs for fewer than 20% of asthma patients, and fewer than 5% of institutions performed PFTs for more than 80% of asthma patients (Figure 3).
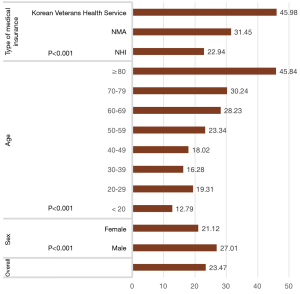
We also analysed PFT performance rate by general patient characteristics. As shown in Figure 4, the comparison of PFT performance rate by type of medical insurance revealed that patients who were covered by KVHS received PFT most frequently, followed by NMA and NHI (Figure 4; P<0.001 by chi-squared test, P<0.001 by Mantel-Haenszel chi-squared test). Also, male patients received PFTs more frequently than did female patients (27.01% vs. 21.12%, P<0.001 by chi-squared test). Overall, there were significant differences in PFT performance ratios among age groups (P<0.001 by chi-squared test). The PFT performance rate was higher for elderly patients than for younger patients (P<0.001 by Mantel-Haenszel chi-squared test).
Possession rates of PFT equipment at medical institutions are shown in Figure 5. All tertiary hospitals possessed PFT equipment, but only about half of primary health clinics did. A mere 3.15% of branch offices of public health centres possessed PFT equipment.
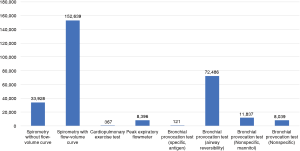
The analysis of performance rate by PFT type showed that the spirometry with flow-volume curve test was performed in the highest number of patients (n=152,639), followed by the bronchial provocation test (airway reversibility) (n=72,486) (Figure 6). Only 8,396 patients received a peak expiratory flowmeter test, and just 367 received a cardiopulmonary exercise test.
Discussion
In this study, we analysed a nationwide HIRA database to evaluate the current status of PFT performance in South Korea. Medical institutions that treated asthma patients were mainly primary health clinics, and asthma patients were treated mostly through primary health care. However, PFT performance rates were somewhat disappointing at primary health clinics (20.87%), whereas tertiary hospitals maintained a much higher performance rate (78.00%). As the PFT is the most important means of diagnosis and assessment in asthma patients, these results indicate that patients are not diagnosed and treated in a manner consistent with guidelines, especially at primary health clinics (1).
Previous studies have continuously reported underutilization of PFTs. In an analysis of Sweden’s Skaraborg Primary Care Database (SPCD) covering 2000–2005, only 20% of asthma patients in primary care were reported to have received spirometry at diagnosis, and 38% received it at follow-up (10). A Canadian study utilizing the Ontario Asthma Surveillance Information System (OASIS) database covering 1997–2007 found that only 42.7% of 465,866 asthma patients (95% CI, 42.6–42.9%) received a PFT during the peri-diagnostic period (11). Another population-based study from Germany reported that 54.1% (95% CI, 50.2–58.0%) of patients with asthma received a PFT in 2010 (4). Although previous studies have reported lower than expected rates of PFT performance, our results were even lower, which may be due to ignorance of the guidelines at primary health clinics. Also, some doctors, especially non-specialists, may not have been well-trained to utilize PFT equipment. Therefore, further training system is needed.
The importance of primary health care has been emphasized in past decades. It is well known that improvement of primary health care quality leads to a decrease in hospitalizations for ambulatory care sensitive conditions (ACSC), including asthma (12,13). In the German study, asthma patients in primary health care were voluntarily enrolled in a German national asthma disease management program (DMP), which regulates asthma care quality (4). Patients enrolled in the DMP saw significant improvements in asthma care, including attention to smoking cessation, inhalation techniques, asthma management plans, and PFT performance. In Sweden, primary health care centres have been using Asthma and COPD Nurse Practitioners (ACNPs) to improve management of asthma and COPD patients (14). In this practice, specially trained nurses examine lung function and maintain patient follow-up. Patients who were visited by ACNPs had overwhelmingly higher PFT performance rates (98% vs. 5%) and smoking habits documentation (78% vs. 28%) compared to patients visited by general practitioners.
In our study, male and elderly patients tended to receive PFTs more frequently. The discrepancy of PFT performance rate between different sex and age groups may have been affected by several factors. As patient factors, willingness to spend time for additional diagnostic procedures, or self-awareness of disease characteristics may have encouraged older patients to receive PFT after recommendation of doctors (15). Also, clinicians may have been more cautious in elderly patients with symptoms of dyspnea, compared to younger patients. Doctors may have used PFT more in elderly patients to differentiate other conditions such as chronic obstructive pulmonary disease (COPD). Finally, our study design may have affected these differences. We included asthma patients in our study by doctor-reported diagnostic codes. As a result, there are some possibilities that patients with ACO (asthma COPD overlap) may have been included in our patient group. As PFT is indispensable in diagnosis of COPD, this may explain the reason of high PFT performance rate in elderly and male patients (16).
In the German study, elderly patients had a significantly higher PFT performance rate compared to younger patients, which is consistent with our study (4). However, in contrast to our results, the German study found that female patients received PFTs slightly more frequently than male patients (56.6% vs. 50.3%), though this difference was not statistically significant. In the German study, a factor that significantly affected PFT performance rate was non-obese BMI status. In the Canadian study, patients aged between 50 and 59 years had highest PFT performance rate, and rates decreased in younger and older patients (11). Unlike our study, female patients had a significantly higher PFT performance rate than male patients. Additionally, low socioeconomic status, rural residence, high comorbidity, absence of medical specialist involved in care, and being initially diagnosed between October and December were associated with poor PFT performance rates.
The greatest strength of this study is the large number of patients and institutions involved; it covered nearly every asthma patient in South Korea. This study showed the underutilization of PFTs in real-world terms, especially in primary health care. However, there are some limitations to this study. First, the study was designed as an observational, retrospective study, which may create several biases. Second, this study only includes 1 year of data. Analysis of long-term databases should be done in further studies.
Conclusions
In this study, we used the 2013 HIRA database to evaluate PFT performance rates in South Korea. This study showed that PFT performance rates were significantly lower than would be expected according to performance guidelines. The poor performance rates were most notable in primary health clinics, in specialties other than internal medicine, and for female and younger patients.
Acknowledgements
This study was supported by HIRA (Join Project on Quality Assessment Research).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This study was approved by the ethics committee of Seoul St. Mary’s Hospital (KIRB-0E482-001). The requirement for informed consent from the patients was waived due to the retrospective nature of this study and anonymity of the data.
References
- Fanta CH. Asthma. N Engl J Med 2009;360:1002-14. [Crossref] [PubMed]
- Masoli M, Fabian D, Holt S, et al. The global burden of asthma: executive summary of the GINA Dissemination Committee report. Allergy 2004;59:469-78. [Crossref] [PubMed]
- Trends in asthma morbidity and mortality [database on the Internet]. American Lung Association. 2016. Available online: http://www.lung.org/assets/documents/research/asthma-trend-report.pdf, accessed: March 1, 2016
- Steppuhn H, Langen U, Mueters S, et al. Asthma management practices in adults--findings from the German Health Update (GEDA) 2010 and the German National Health Interview and Examination Survey (DEGS1) 2008-2011. J Asthma 2016;53:50-61. [Crossref] [PubMed]
- Hasegawa K, Tsugawa Y, Clark S, et al. Improving Quality of Acute Asthma Care in US Hospitals: Changes Between 1999-2000 and 2012-2013. Chest 2016;150:112-22. [Crossref] [PubMed]
- Braido F, Brusselle G, Guastalla D, et al. Determinants and impact of suboptimal asthma control in Europe: The international cross-sectional and longitudinal assessment on asthma control (LIAISON) study. Respir Res 2016;17:51. [Crossref] [PubMed]
- Vermeire PA, Rabe KF, Soriano JB, et al. Asthma control and differences in management practices across seven European countries. Respir Med 2002;96:142-9. [Crossref] [PubMed]
- To T, Guan J, Zhu J, et al. Quality of asthma care under different primary care models in Canada: a population-based study. BMC Fam Pract 2015;16:19. [Crossref] [PubMed]
- Grace MS, Baxter M, Dubuis E, et al. Transient receptor potential (TRP) channels in the airway: role in airway disease. Br J Pharmacol 2014;171:2593-607. [Crossref] [PubMed]
- Weidinger P, Nilsson JL, Lindblad U. Adherence to diagnostic guidelines and quality indicators in asthma and COPD in Swedish primary care. Pharmacoepidemiol Drug Saf 2009;18:393-400. [Crossref] [PubMed]
- Gershon AS, Victor JC, Guan J, et al. Pulmonary function testing in the diagnosis of asthma: a population study. Chest 2012;141:1190-6. [Crossref] [PubMed]
- Rosano A, Loha CA, Falvo R, et al. The relationship between avoidable hospitalization and accessibility to primary care: a systematic review. Eur J Public Health 2013;23:356-60. [Crossref] [PubMed]
- Gibson OR, Segal L, McDermott RA. A systematic review of evidence on the association between hospitalisation for chronic disease related ambulatory care sensitive conditions and primary health care resourcing. BMC Health Serv Res 2013;13:336. [Crossref] [PubMed]
- Carlfjord S, Lindberg M. Asthma and COPD in primary health care, quality according to national guidelines: a cross-sectional and a retrospective study. BMC Fam Pract 2008;9:36. [Crossref] [PubMed]
- Dennis SM, Zwar NA, Marks GB. Diagnosing asthma in adults in primary care: a qualitative study of Australian GPs' experiences. Prim Care Respir J 2010;19:52-6. [Crossref] [PubMed]
- GOLD Guideline, 2018. Available online: http://goldcopd.org/