Knowledge and practice of Chinese physicians toward carbapenem-resistant enterobacteriaceae: a nationwide cross-sectional survey in top 100 hospitals
Introduction
Antimicrobial resistance has markedly increased worldwide concern over the past decades, while the current emergence of carbapenem-resistant enterobacteriaceae (CRE) constitutes a great public health threat (1,2). In United States, CRE infections have been confirmed in nearly all states and are associated with 25% attributable mortality (3,4). A single CRE infection can cost ranging from $22,484 to $66,031 for hospitals, $10,440 to $31,621 for third-party payers, and $37,778 to $83,512 for society (4). Because of limited antibiotic options to treat such infections, CRE is listed as a critical priority pathogen by the World Health Organization (WHO) to guide research, discovery, and development of new antibiotics (5).
In China, carbapenem-resistance of Klebsiella pneumoniae clinical strains has increased from 2.4% to 13.4% over the past decade (6), while different carbapenem resistance rate and relative prevalence of various carbapenemase genes among clinical Escherichia coli strains have been reported from different provinces of China (7,8). However, Chinese tertiary hospitals, located in different cities, not only provide high-level medical and health services, but are also responsible for medical higher education and scientific research, where the physicians’ knowledge and practice are different per definitions with respect to case mix, intensity of care provided, and other personal experience. Since the emergence of hypervirulent carbapenem-resistant K. pneumoniae isolates has been frequently documented in recent years (9-11), the concern is growing regarding urgent public health threat due to these gram-negative organisms.
As physicians are the major player in clinical treatment and hospital infection control, less attention has been focused on their general knowledge and practice toward this rapidly evolving gram-negative resistance issue. Therefore, a national cross-sectional survey was conducted in Chinese top 100 hospitals, representing the healthcare facility elite, to understand the current knowledge and practice of Chinese physicians toward CRE.
Methods
Survey population
The study was a cross-sectional survey of CRE-related knowledge and practice of Chinese physicians in top 100 large-size tertiary comprehensive hospitals (ranked by Ailibi Hospital Management Forum, available at: http://www.ailibi.com/index.php/portal/article/index/tid/125). At least eight physicians in each tertiary hospital were randomly invited by the chiefs of the Department of Infection Control: two from the Department of Intensive Care Unit (ICU), two from the Department of Respiratory Medicine, two from the Department of Hematology and two from the Department of Infectious Diseases (only diagnosis and treatment of infectious diseases). Only the attending physicians, associate chief physicians, and chief physicians were included in this study, while the junior physicians were excluded. Ethical approval for this study was obtained from the Institution of Review Board of Fudan University.
Survey questionnaire
The questionnaire was self-designed after consulting a large number of published studies and was revised after experts’ evaluation. The questionnaire comprised three sections: (I) socio demographic information; (II) CRE knowledge, and (III) practice options toward CRE. The nine knowledge questions focused on the indications for CRE treatment and awareness of infection control. The four practice questions focused on the CRE treatment, high-risk factors and infection control strategy (Supplementary file).
Survey procedure
The Nosocomial Infection Control Sector of Chinese Preventive Medicine Association sent emails in 2 weeks to the chiefs of the Department of Infection Control of the top 100 tertiary hospitals between June–July 2017. One week later, questionnaires were sent to the chiefs of the Departments of Infection Control who accepted to participate and invited the designated physicians to complete the questionnaires. The completed questionnaires were both mailed and submitted online to The Nosocomial Infection Control Sector of Chinese Preventive Medicine Association. All participants took part in the study on a voluntary and a real-name registration system.
Data collection
The collected questionnaires were reviewed manually, and the missing responses were corrected or verified by re-contacting the respondents. All data were double checked and input into a database. For knowledge questions, each correct answer was given 1 score, whereas 0 score was given to wrong answers. The total scores were classified into three levels as follows: (I) high level: 7–9 scores; (II) moderate level: 4–6 scores; (III) low level: 0–4 scores.
Statistical analyses
Statistical analyses were performed using SPSS statistical software (version 19; SPSS Inc., Chicago, IL). Continuous data were described as median and range or as mean ± standard deviation (SD) according to their distribution. Categorical data were evaluated using chi-square tests. Odds ratios (ORs) and 95% confidence intervals (CIs) were determined by logistic regression analysis. Variables associated with knowledge level with P values ≤0.10 in univariate analyses were included in an ordinal logistic regression model. All P values were two-tailed, and P values ≤0.05 were considered statistically significant.
Results
Socio demographic characteristics
A total of 529 physicians from 53/100 (53%) hospitals accepted and completed the questionnaires, and all responses were available for the study. The characteristics of the physicians are displayed in Table 1. The cities in which the designed hospitals were located were categorized by New Tier City Institute as first-tier cities, new first-tier cities, or second-tier cities (The detailed rank available at: https://www.cbnweek.com/articles/normal/20927). Males and females were equally represented, and the mean age of the physicians was 38.3 (SD 6.6). The proportion of physicians in Department of ICU, Department of Respiratory Medicine, Department of Hematology, and Department of Infectious Diseases was 41.0%, 26.8%, 21.2% and 11.0%, respectively. Of the 529 physicians, 195 (36.9%) had a PhD/MD degree, whereas 264 (49.9%) had a master’s degree.
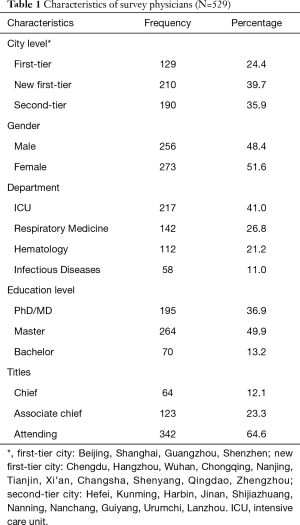
Full table
CRE knowledge assessment
The respondents answered a total of nine questions regarding CRE knowledge, and distribution of responses to each knowledge question is shown in Table 2. The percentage of correct answers to each question ranged from 25.7% to 89%, and the scores ranged from 1 to 9, with a median of 6 (interquartile range, 5–7). The physicians demonstrated insufficient knowledge about the right use of antibiotics to CRE (question Nos. 4, 5, and 7). The level of knowledge of respondents was as follows: high, 28.92%; moderate, 62.94; and low, 8.12%.
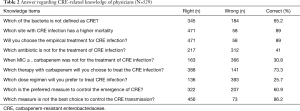
Full table
Factors associated with the knowledge level
Factors associated with the modified CRE knowledge score from ordinal logistic regression are shown in Table 3. All demographic characteristics including clinical experience were included in the model. A significant relationship was found between CRE knowledge level and demographic characteristics of city level, work department, and CRE infection treated in the last 6 months after adjusting for the other variables in the model. Specifically, the physicians who worked in first-tier cities and new first-tier cities had a higher knowledge level compared with those who worked in second-tier cities. The physicians in the Department of Infectious Diseases had a higher knowledge level compared with those in the Department of ICU, Department of Respiratory Medicine, and Department of Hematology. However, differences were not found among physicians in the Department of ICU, Department of Respiratory Medicine, and Department of Hematology. Furthermore, the physicians who treated CRE infection in the last 6 months had a higher knowledge level compared with those who did not.
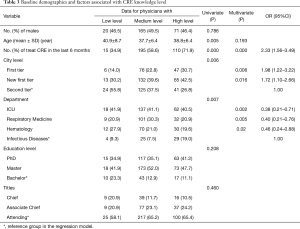
Full table
Clinical and infection control practices
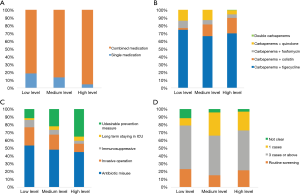
Figure 1A,B,C,D shows the distribution of physicians’ practices toward CRE clinical and infection control. The proportion of physicians who sought to treat CRE infection with combined medication was respectively 81.4%, 86.5% and 95.4%, according to their CRE knowledge level (Figure 1A). However, the primary treatment given by physicians with different knowledge levels was tigecycline combined with carbapenem (74.4%, 66.4%, and 69.9%, respectively; Figure 1B). In infection control practices, the proportion of physicians considering invasive operations with the indwelling catheter as the main risk factor was 23.3%, 19.2%, and 10.5%, respectively. While the proportion of physicians considering undesirable infection control practice as the main risk factor was 11.6%, 21.9%, and 35.3%, respectively (Figure 1C). However, no significant difference was observed between their knowledge levels and best choice in CRE screening (Figure 1D).
Discussion
A large proportion of hospital-acquired infections caused by multidrug-resistant organisms (MDROs) have been frequently documented in recent years, increasing mortality, readmissions, and economic burden (4,12,13). Although MDROs have received national media and legislative concerns, this was the first nationwide survey about the knowledge and practice toward CRE among Chinese physicians. Unlike studies addressing knowledge on antibiotic use (14-16), the present study focused mainly on the current physician’ knowledge and practice when facing CRE infection.
In fact, the number of cities in China has exceeded 600 and they are categorized by New Tier City Institute, an unofficial academic research institute, as first- to fifth-tier cities. First-tier cities have higher commercial resources aggregation, transportation convenience, and future development than other tier cities, resulting in more top hospitals located and elite physicians gathered. The results showed that the total scores for knowledge ranged from 1 to 9 (median =6; interquartile range, 5–7), indicating that the current knowledge of Chinese physicians toward CRE is common. Similar, the study by Thibodeau (17) on 434 medicine clinicians in 3 teaching hospitals found that 51.1% of clinicians correctly scored 50% or greater on the knowledge questions. Our multivariate analysis showed that some investigated demographic characteristics, such as city level, work department, and personal experience, had an impact on CRE-related knowledge. Especially, the physicians who worked in first-tier cities, served in the Department of Infectious Diseases, or have treated CRE infection in the last 6 months, had a higher knowledge level for they have more opportunities for academic exchange and personnel training. Therefore, the need for increased awareness of CRE-related knowledge by Chinese physicians is obvious.
As this survey was conducted in 2017 summer, CRE was endemic in Chinese hospitals, and nearly 60.5% of physicians dealt with CRE infection in the last 6 months. Still several misunderstandings exist on the major of physicians. For instance, the organisms of CRE are resistant to nearly all antibiotics, including third-generation cephalosporin. However, 59% of surveyed physicians still considered that cefoperazone was suitable for the treatment of CRE infection, which might lead to the abuse of antibiotics for clinical treatment. Besides, higher dose of meropenem rather than imipenem can be selected to treat CRE infection by Chinese expert consensus, but 74.3% of surveyed physicians have no sense of carbapenems treatment to CRE and made wrong answer. This misunderstanding regarding the use of carbapenem in treatment was worse than previously thought. Therefore, more systematic and targeted education for physicians is highly needed to address such misunderstandings.
In addition, this study also compared the clinical and infection control practices of physicians with different levels of CRE knowledge. Although infection control practices effectively decrease the spread of resistance during outbreaks (18), awareness among clinicians is imperative in preventing further spread of this epidemic. However, variation in practice regarding CRE among physicians may illustrate how knowledge regarding CRE threats and controls differ within the hospitals. Take Figure 1D as an instance, WHO has recommend that surveillance screening for CRE should be performed as soon as possible after hospital admission or risk exposure while China has not issued guidelines or consensus on the timing of screening for CRE. Therefore, major of the surveyed physicians considered that screening for CRE should be performed in healthcare associated outbreak according to Chinese guideline. As reported by Fedorowsky (19), lower CRE incidence rates were associated with higher organizational culture scores, so it’s necessary to conducted more organizational culture or training for Chinese physicians to improve their compliance with practice or knowledge level.
The present study had some limitations. First, only 53 of top 100 large-size tertiary comprehensive hospitals were involved, and not all physicians in designated departments participated in this survey, which might affect these results. Second, the questionnaire was not designed for a 5-point Likert scale, but adaptations were made for specific components unique to CRE. However, many gaps in knowledge and a great deal of variability in opinions in Chinese physicians with regard to CRE infection were found, highlighting the urgent need for more targeted education and interventions.
Supplementary
Knowledge and practice of physicians toward CRE questionnaire
1. Socio demographic information
Name: _______________ Gender:______________ Age:_________
Province: _____________ Hospital: ___________________________________________________
Department: __________________(1.ICU 2.Respiatory Medicine 3. Hematology 4. Infectious Diseases)
Educational level: ______________(1.Ph.D 2.Master 3.Bachelor)
Titles: ___________(1. Chief physician 2. Associate chief physician 3. Attending physician)
Treat CRE infection in the last 6 months: ___________(1. Yes 2. No)
2. CRE knowledge
2.1 Which of the bacteria is not defined as CRE?
A. Carbapenem-resistant Escherichia coli
B. Carbapenem-resistant Klebsiella pneumoniae
C. Carbapenem-resistant Proteus
D. Carbapenem-resistant Pseudomonas aeruginosa*
2.2 Which site with CRE infection has higher mortality?
A. Bloodstream infection*
B. Pulmonary infection
C. Urinary tract infection
D. Other site infection
2.3 Is that right to choose the empirical treatment for CRE infection?
A. Yes*
B. No
2.4 Which antibiotic is not for the treatment of CRE infection?
A. Cefoperazone*
B. Meropenem
C. Amikacin
D. Tigecycline
E. Colistin
2.5 When the MIC breakpoint ≥, carbapenem was not for the treatment of CRE infection?
A. 1
B. 2
C. 4
D. 8*
E. 16
2.6 Which therapy with carbapenem will you choose to treat the CRE infection?
A. Increase the dose
B. Prolonged infusion time
C. Combined medication
D. All above*
2.7 Which dose regimen will you prefer to treat CRE infection?
A. Imipenem 1g q8h
B. Imipenem 1g q6h
C. Imipenem 2g q8h
D. Meropenem 1g q8h
E. Meropenem 2g q8h*
2.8 Which is the preferred measure to control the emergence of CRE?
A. Avoiding overuse of prophylactic antibiotics
B. Rational selection of antibiotic types and dosages*
C. Limit the use of carbapenem antibiotics
D. Innovation new antibiotic
E. Antimicrobial stewardship in agriculture
2.9 Which measure is not the best choice to control the CRE transmission?
A. Active surveillance
B. Contact precautions
C. Hand washing
D. Environmental cleaning
E. Selective digestive decontamination*
*Correct response to each question
3. Practice options toward CRE
3.1 Which treatment will you prefer for CRE infection?
A. Single medication
B. Combined medication
3.2 Which antibiotic will you prefer to treat CRE infection?
A. Carbapenem + tigecycline
B. Carbapenem + colistin
C. Carbapenem + fosfomycin
D. Carbapenem + quinolone
E. Double carbapenem
3.3 Which is the major risk factor for CRE infection/colonization?
A. Antibiotic misuse
B. Invasive operation
C. Immunosuppressive
D. Long-term stay in the ICU
E. Undesirable preventive measure
3.4 When do you recommend impatient for CRE screening?
A. Not clear
B. 1 case
C. 3 cases or above
D. Routine screening
Acknowledgements
The authors would like to thank all participants and chiefs of the Departments of Infection Control who accepted to participate in this study.
Funding: This work was supported by Sumitomo Pharma (Suzhou) Co. Ltd.; The 4th Three-year Action Plan for Public Health of Shanghai (The Project No.: 15GWZK0101); Research project plan of Shanghai Municipal Commission of Health and Family Planning Funding (201640313).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: Ethical approval for this study was obtained from the Institution of Review Board of Fudan University.
References
- Magill SS, Edwards JR, Bamberg W, et al. Multistate point-prevalence survey of health care-associated infections. N Engl J Med 2014;370:1198-208. [Crossref] [PubMed]
- Moellering RC Jr. NDM-1--a cause for worldwide concern. N Engl J Med 2010;363:2377-9. [Crossref] [PubMed]
- Guh AY, Bulens SN, Mu Y, et al. Epidemiology of Carbapenem-Resistant Enterobacteriaceae in 7 US Communities, 2012-2013. JAMA 2015;314:1479-87. [Crossref] [PubMed]
- Bartsch SM, McKinnell JA, Mueller LE, et al. Potential economic burden of carbapenem-resistant Enterobacteriaceae (CRE) in the United States. Clin Microbiol Infect 2017;23:48.e9-e16. [Crossref] [PubMed]
- Tacconelli E, Carrara E, Savoldi A, et al. Discovery, research, and development of new antibiotics: the WHO priority list of antibiotic-resistant bacteria and tuberculosis. Lancet Infect Dis 2018;18:318-27. [Crossref] [PubMed]
- Hu FP, Guo Y, Zhu DM, et al. Resistance trends among clinical isolates in China reported from CHINET surveillance of bacterial resistance, 2005-2014. Clin Microbiol Infect 2016;22 Suppl 1:S9-14. [Crossref] [PubMed]
- Zhang R, Liu L, Zhou H, et al. Nationwide Surveillance of Clinical Carbapenem-resistant Enterobacteriaceae (CRE) Strains in China. EBioMedicine 2017;19:98-106. [Crossref] [PubMed]
- Zhang R, Chan EW, Zhou H, et al. Prevalence and genetic characteristics of carbapenem-resistant Enterobacteriaceae strains in China. Lancet Infect Dis 2017;17:256-7. [Crossref] [PubMed]
- Zhang Y, Zeng J, Liu W, et al. Emergence of a hypervirulent carbapenem-resistant Klebsiella pneumoniae isolate from clinical infections in China. J Infect 2015;71:553-60. [Crossref] [PubMed]
- Zhang R, Lin D, Chan EW, et al. Emergence of Carbapenem-Resistant Serotype K1 Hypervirulent Klebsiella pneumoniae Strains in China. Antimicrob Agents Chemother 2015;60:709-11. [Crossref] [PubMed]
- Gu D, Dong N, Zheng Z, et al. A fatal outbreak of ST11 carbapenem-resistant hypervirulent Klebsiella pneumoniae in a Chinese hospital: a molecular epidemiological study. Lancet Infect Dis 2018;18:37-46. [Crossref] [PubMed]
- Barrasa-Villar JI, Aibar-Remon C, Prieto-Andres P, et al. Impact on Morbidity, Mortality, and Length of Stay of Hospital-Acquired Infections by Resistant Microorganisms. Clin Infect Dis 2017;65:644-52. [Crossref] [PubMed]
- Maechler F, Pena Diaz LA, Schroder C, et al. Prevalence of carbapenem-resistant organisms and other Gram-negative MDRO in German ICUs: first results from the national nosocomial infection surveillance system (KISS). Infection 2015;43:163-8. [Crossref] [PubMed]
- Bai Y, Wang S, Yin X, et al. Factors associated with doctors' knowledge on antibiotic use in China. Sci Rep 2016;6:23429. [Crossref] [PubMed]
- Yu M, Zhao G, Stalsby Lundborg C, et al. Knowledge, attitudes, and practices of parents in rural China on the use of antibiotics in children: a cross-sectional study. BMC Infect Dis 2014;14:112. [Crossref] [PubMed]
- Wang X, Peng D, Wang W, et al. Massive misuse of antibiotics by university students in all regions of China: implications for national policy. Int J Antimicrob Agents 2017;50:441-6. [Crossref] [PubMed]
- Thibodeau E, Doron S, Iacoviello V, et al. Carbapenem-resistant enterobacteriaceae: analyzing knowledge and practice in healthcare providers. PeerJ 2014;2. [Crossref] [PubMed]
- Munoz-Price LS, Hayden MK, Lolans K, et al. Successful control of an outbreak of Klebsiella pneumoniae carbapenemase-producing K. pneumoniae at a long-term acute care hospital. Infect Control Hosp Epidemiol 2010;31:341-7. [Crossref] [PubMed]
- Fedorowsky R, Peles-Bortz A, Masarwa S, et al. Carbapenem-resistant Enterobacteriaceae carriers in acute care hospitals and postacute-care facilities: The effect of organizational culture on staff attitudes, knowledge, practices, and infection acquisition rates. Am J Infect Control 2015;43:935-9. [Crossref] [PubMed]


