Microinvasive segmentectomy: a case of video-assisted thoracic surgery left S9+10 segmentectomy
Introduction
Different from lingual or superior segmentectomy, procedures like anterior (S3) segmentectomy can be regarded as complicated type of segmentectomy, because of the complicated type including resection of more than one intersegmental plane. Accurate division of the planes is vital to the procedure and it relies on the accurate division of every branch of target segmental vessels and bronchi. We reported the process of a video-assisted thoracoscopic surgery (VATS) anatomical left S9+10 segmentectomy for a GGO lesion in a 66-year-old male.
Surgical technique
A GGO lesion at S9+10 of left lower lobe in a 66-year-old male patient was identified 12 months ago. The lesion was found increased by a follow-up CT scan. A three-dimensional (3D) reconstruction of lung by the chest CT scan was performed to identify the location of the lesion and the possible variations of the pulmonary vessels and bronchi. We made a surgical plan of a VATS Left S9+10 segmentectomy on this patient (Figure 1).

After intubated, the patient was placed in the right lateral decubitus position. A 10-mm port was placed in the 8th intercostal space on the mid axillary line. Another incision of about 2 cm and an incision of about 1.5 cm were made in the 5th intercostal space on the left anterior axillary line and in the 5th intercostal space on the left posterior axillary line, respectively.
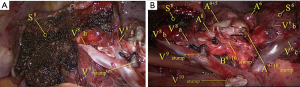
A6, A8 and A10 were identified and skeletonized. A9a and A9b+A10 were then identified and skeletonized. The #12 and #13 lymph nodes were dissected. All the segmental bronchi of left lower lobe were exposed. Branches of B6, B8 and B9+10 were identified before B9+10 was divided. The left lower lobe was then retracted ventrally. The 8–13th levels of lymph nodes were dissected. The tunnel between S6 and S8 were also explored. S6 and S8–10 were divided by an endostapler. A9+10 was cut and B9+10 was then revealed and cut. All branches of the pulmonary vein of the left lower lobe were exposed and skeletonized from surrounding pulmonary parenchyma for as long as possible. Branches V9 and V10 were then identified and divided.
The whole left lung was inflated with pure oxygen and then deflated for 15 minutes. The inflation-deflation line was clear between S8 and S9+10. The intersegmental plane of S9+10 and S8 was divided along the V8b and also along the inflation-deflation border line firstly using electrocautery and then an endostapler. Intraoperative frozen sections revealed a pathological diagnosis of invasive adenocarcinoma with no segmental lymph nodes involvement. A systematic lymph node dissection was then performed.
After S9+10 resection, S8 and S6 were separated. V6 and V8 were identified and preserved on the intersegmental plane of S6 and S8 separately (Figure 2).
Discussion
Several literatures have showed that segmentectomy can achieve equivalent therapeutic effect to lobectomy for stage IA lung cancer (2-4). But the major defects, such as the wrong division of segmental vessels or insufficient resection margin distance, can cause unnecessary harm to the patients and even endanger the treatment value of the procedure for the lung neoplasm. These defects should be avoided as far as possible. The S9+10 segmentectomy of the lower lobe is a complicated type of segmentectomy which includes division of two intersegmental planes (5). The variations of the pulmonary vessels in the lower lobe are very common. The identification of the target segment with enough resection margin distance and the complete understanding of the variation pattern before surgery are recommended for a smooth and accurate S9+10 segmentectomy. We referred to the preoperative 3D reconstruction of the lung by CT scan (6) to achieve these targets. In this case, we found segmentectomy of the S9+10 to be the proper surgery for its satisfaction of complete removal of the lesion with enough resection margin distance. We also detected the proper branching pattern of the vessels and bronchi preoperatively with this tool. We use a sculpting manner (7) to perform the biopsy of the whole lower lobe. Every important structure was compared with the 3D reconstruction image and identified before being divided. This manner helps to preclude any major default in dividing the target segmental vessels or bronchi.
In this case, we divided the intersegmental plane of S6 and S9+10 using a tunnel manner by staplers. After the division, it became easy for exposure of the segmental vessels and bronchi of S9 and S10. We chose electrocautery combined with staplers for the division of the S8 and S9 intersegmental plane. Electrocautery has been shown to be useful for dissecting the intersegmental plane (8,9). In our opinion, combination of both manners for the division may be ideal in the complex type of segmentectomy. It may decrease the number of the staplers in the operation, preserving the intersegmental veins and ameliorating the expansion of S8. Since the resection margin was enough according to the 3D reconstruction preoperatively we divided along the deflation-inflation plane and adjacent to the target segment by electrocautery. We inflated the remnant lung and examined the air leak after the removal of target segments. Only slight air leak was detected. In our opinion, to keep the electrocautery dividing in the target segments, adjacent to the correct intersegmental plane is vital in the plane-dividing process. And a clear intersegmental plane relies on the correctness of division of the branches of vessels and bronchi of the target segments.
Conclusions
For complicated type of segmentectomy procedures, we suggest proper surgical planning according to 3D reconstruction based on CT images. Precise identification and accurate division of the anatomical structures is fundamental to carry out this type of segmentectomy smoothly.
Acknowledgements
Dr. Yunfeng Yuan was granted the Award of Excellence in the 2017 VATS Lobectomy & Segmentectomy Video Contest.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Xue L, Yuan Y. Left S segmentectomy. Asvide 2018;5:642. Available online: http://www.asvide.com/article/view/26151
- Koike T, Yamato Y, Yoshiya K, et al. Intentional limited pulmonary resection for peripheral T1 N0 M0 small-sized lung cancer. J Thorac Cardiovasc Surg 2003;125:924-8. [Crossref] [PubMed]
- Keenan RJ, Landreneau RJ, Maley RH Jr, et al. Segmental resection spares pulmonary function in patients with stage I lung cancer. Ann Thorac Surg 2004;78:228-33; discussion-233.
- Okada M, Koike T, Higashiyama M, et al. Radical sublobar resection for small-sized non-small cell lung cancer: a multicenter study. J Thorac Cardiovasc Surg 2006;132:769-75. [Crossref] [PubMed]
- Iwata H, Shirahashi K, Mizuno Y, et al. Surgical technique of lung segmental resection with two intersegmental planes. Interact Cardiovasc Thorac Surg 2013;16:423-5. [Crossref] [PubMed]
- Shimizu K, Nakano T, Kamiyoshihara M, et al. Segmentectomy guided by three-dimensional computed tomography angiography and bronchography. Interact Cardiovasc Thorac Surg 2012;15:194-6. [Crossref] [PubMed]
- Xue L, Yuan Y. Microinvasive segmentectomy in a sculpting manner: a case of VATS left S(1+2) segmentectomy. J Thorac Dis 2017;9:3265-8. [Crossref] [PubMed]
- Saito H, Konno H, Atari M, et al. Management of Intersegmental Plane on Pulmonary Segmentectomy Concerning Postoperative Complications. Ann Thorac Surg 2017;103:1773-80. [Crossref] [PubMed]
- Ohtsuka T, Goto T, Anraku M, et al. Dissection of lung parenchyma using electrocautery is a safe and acceptable method for anatomical sublobar resection. J Cardiothorac Surg 2012;7:42. [Crossref] [PubMed]


