Neoadjuvant PD-1 blockade in non-small cell lung cancer: what else do we need to do?
For decades, systemic therapy for non-small cell lung cancer (NSCLC) was subjected to cytotoxic agents. For patients with locally advanced NSCLC (stages IIIA–B) not suitable to surgical resection, the current standard of regimen is concurrent chemoradiotherapy, which induces median survival time in excess of 2- and 5-year survival of 15–20% (1). For advanced NSCLC patients, the application of third-generation of chemotherapy drugs such as docetaxel, paclitaxel and gemcitabine, had improved the overall survival to 8 months (2). For resectable NSCLC patients, neoadjuvant chemotherapy would significantly improve the overall survival (HR =0.84; 95% CI, 0.77–0.92; P=0.0001). With regard to stage III NSCLC, the result was similar (HR =0.84; 95% CI, 0.75–0.95; P=0.005) (3). However, in 2002, Carney concluded that we had reached a plateau of efficacy in NSCLC, which cannot be improved further with conventional chemotherapeutic drugs (4).
In 2009, the approval of gefitinib for advanced NSCLC in all lines of treatment for patients harboring EGFR mutations opening the age of molecularly targeted drugs in NSCLC. Targeted therapy is a very important component of precision medicine, a medical model that proposes the customization of diagnostic tests, treatments and medical practices based on patients’ genetic mutation or other molecular or cellular subtypes. For this, targeted therapy is limited by the gene mutation status. Dr. Tsao predicted up to 69% patients with NSCLC could have a potentially actionable target (5), but so far, only EGFR and ALK mutation subgroups could have FDA approved targeted therapy, which accounting 24% of NSCLC patients (6).
Fortunately, the emergence of immune checkpoint inhibitors has tremendously improved the treatment for patients with solid tumors, such as NSCLC and melanoma. Programmed death 1 (PD-1) is a key immune checkpoint receptor expressed by activated T cells and mediates immunosuppression (7). In physiological conditions, programmed death-ligand 1 (PD-L1) could bind to its receptor PD-1, resulting in cytotoxic T cell apoptosis and prevent autoimmune diseases of heart, lung, thymus, spleen, kidney, etc. However, the overexpression of PD-L1 on tumor cells, dampening immunosurveillance (8). Blockade of PD-1, including PD-1 antibodies and PD-L1 antibodies, such as nivolumab (PD-1 Ab, Bristol-Myers Squibb), pembrolizumab (PD-1 Ab, Merck Sharp & Dohme) and atezolizumab (PD-L1 Ab, Hoffmann-La Roche) helps overcome immune resistance, representing a major breakthrough therapy across multiple malignancies including NSCLC. Since the conduction of first PD-1 blockade randomized controlled trial (RCT) at 2006, more and more RCTs have demonstrated durable responses, improved survival and reduced treatment-related adverse events (TRAEs) in patients with previously treated and untreated advanced NSCLC (9-15). Among the numerous advantages of immunotherapy, the most distinct one is long OS after response. According to Dr. Gettinger, the estimated 5-year OS rate was 16% for all pretreated advanced NSCLC patients (N=129) received nivolumab, compared with 5% 5-year OS rate in this population without immunotherapy (16).
Just as the emergence of neoadjuvant chemotherapy, neoadjuvant immunotherapy was also raised after successfully applied to advanced stage NSCLC. Neoadjuvant immunotherapy for NSCLC patients was first reported by Dr. Patrick Forde at EMSO 2016 congress (17). And this study group published their initial experience with lung resection after treatment with immune checkpoint inhibitors for 5 advanced stage NSCLC at 2017 (18). Of these 5 patients, 4 received lobectomy and mediastinal lymph node dissection, one received wedge resection and mediastinal lymph node dissection. All patients had R0 resection and uncomplicated hospital course except one minor chest tube air leak. This initial experience suggests that pulmonary resection after checkpoint inhibitor therapy is feasible, even in patients who experience pneumonitis or other immune-related toxicities during their treatment. The main limitation of this study is small sample size and lack of survival data.
And at 2018, Dr. Matthew published their study about safety and feasibility of lung resection after administration of immune checkpoint inhibitors for metastatic or unresectable tumors (19). This retrospective study reviewed 19 patients who received lung resection within 6 months of treatment with PD-1 or CTLA-4 (T-lymphocyte-associated protein 4) blockade for metastatic or unresectable cancer. The primary tumors include lung cancer, melanoma, breast cancer and sarcoma. Results showed high R0 resection rate (95%), acceptable operation time, acceptable complication rate (32%) and satisfactory 2-year OS and DFS (77%, 42%). This study also revealed common posttreatment adhesions at hilum or the chest wall as similar as neoadjuvant chemotherapy, which was technically challenging to the surgeons. Confounding factors such as various drugs, unequal doses, inconsistent duration from administration drug to surgery, affected the quality of this study. Other limitations of this study were its retrospective nature and small sample size.
Just one month after Dr. Matthew’s publication, Dr. Patrick Forde published their study about neoadjuvant PD-1 blockade in resectable lung cancer on the New England Journal of Medicine (20). Quite different from previous two studies (18,19), this study only enrolled stage I, II, or IIIA NSCLC. Confounding factors were well controlled. Nivolumab (at a dose of 3 mg per kilogram of body weight) was administered intravenously every 2 weeks, with surgery conducted approximately 4 weeks after the first dose. As a result, neoadjuvant nivolumab showed few TRAEs, did not delay surgery and induced a major pathological response in 45% of resected tumors. A significant correlation between tumor mutation burden (TMB) and percentage of residual tumor was detected (Spearman’s rho, −0.75, P=0.008). This study gave us an insight about neoadjuvant immunotherapy. But as a pilot study, it was also limited by small number of patients and lack of long-term follow-up.
Furthermore studies with big sample size and long-term follow-up are warranted to define the role of neoadjuvant immunotherapy in reducing recurrences and improving survival of NSCLC. For the moment, there are 5 active RCTs focusing on neoadjuvant immunotherapy of NSCLC are recruiting patients (Table 1). Before neoadjuvant anti PD-1 immunotherapy could be added to guideline, some questions are necessary to be solved. First, which population should receive neoadjuvant immunotherapy? Second, what is the best marker to predict the patients’ response to immunotherapy. TMB, microsatellite instability (MSI), PD-L1 expression level, tumor infiltrating lymphocyte (TIL) or other factors? It seems that TMB and PD-L1 expression level is feasible to nivolumab and pembrolizumab, respectively. But what about atezolizumab, avelumab, and durvalumab? Third, in consideration of pseudoprogression, what is best way to evaluate the effect of immunotherapy before surgery? Furthermore, right now it is unclear when to stop the immunotherapy. Fourth, about TRAEs of immunotherapy. Will treatment related pneumonitis delay the surgery? How to prevent and treat immunotherapy associated myocarditis? These questions are very important to the widely application of neoadjuvant anti PD-1 immunotherapy.
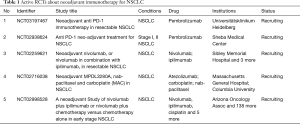
Full table
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Bradley JD, Paulus R, Komaki R, et al. Standard-dose versus high-dose conformal radiotherapy with concurrent and consolidation carboplatin plus paclitaxel with or without cetuximab for patients with stage IIIA or IIIB non-small-cell lung cancer (RTOG 0617): a randomised, two-by-two factorial phase 3 study. Lancet Oncol 2015;16:187-99. [Crossref] [PubMed]
- Schiller JH, Harrington D, Belani CP, et al. Comparison of four chemotherapy regimens for advanced non-small-cell lung cancer. N Engl J Med 2002;346:92-8. [Crossref] [PubMed]
- Song WA, Zhou NK, Wang W, et al. Survival benefit of neoadjuvant chemotherapy in non-small cell lung cancer: an updated meta-analysis of 13 randomized control trials. J Thorac Oncol 2010;5:510-6. [Crossref] [PubMed]
- Carney DN. Lung cancer--time to move on from chemotherapy. N Engl J Med 2002;346:126-8. [Crossref] [PubMed]
- Tsao AS, Scagliotti GV, Bunn PA Jr, et al. Scientific Advances in Lung Cancer 2015. J Thorac Oncol 2016;11:613-38. [Crossref] [PubMed]
- Hirsch FR, Scagliotti GV, Mulshine JL, et al. Lung cancer: current therapies and new targeted treatments. Lancet 2017;389:299-311. [Crossref] [PubMed]
- Dong H, Zhu G, Tamada K, et al. B7-H1, a third member of the B7 family, co-stimulates T-cell proliferation and interleukin-10 secretion. Nat Med 1999;5:1365-9. [Crossref] [PubMed]
- Chemnitz JM, Parry RV, Nichols KE, et al. SHP-1 and SHP-2 associate with immunoreceptor tyrosine-based switch motif of programmed death 1 upon primary human T cell stimulation, but only receptor ligation prevents T cell activation. J Immunol 2004;173:945-54. [Crossref] [PubMed]
- Fehrenbacher L, Spira A, Ballinger M, et al. Atezolizumab versus docetaxel for patients with previously treated non-small-cell lung cancer (POPLAR): a multicentre, open-label, phase 2 randomised controlled trial. Lancet 2016;387:1837-46. [Crossref] [PubMed]
- Borghaei H, Paz-Ares L, Horn L, et al. Nivolumab versus Docetaxel in Advanced Nonsquamous Non-Small-Cell Lung Cancer. N Engl J Med 2015;373:1627-39. [Crossref] [PubMed]
- Brahmer J, Reckamp KL, Baas P, et al. Nivolumab versus Docetaxel in Advanced Squamous-Cell Non-Small-Cell Lung Cancer. N Engl J Med 2015;373:123-35. [Crossref] [PubMed]
- Herbst RS, Baas P, Kim DW, et al. Pembrolizumab versus docetaxel for previously treated, PD-L1-positive, advanced non-small-cell lung cancer (KEYNOTE-010): a randomised controlled trial. Lancet 2016;387:1540-50. [Crossref] [PubMed]
- Reck M, Rodríguez-Abreu D, Robinson AG, et al. Pembrolizumab versus Chemotherapy for PD-L1-Positive Non-Small-Cell Lung Cancer. N Engl J Med 2016;375:1823-33. [Crossref] [PubMed]
- Langer CJ, Gadgeel SM, Borghaei H, et al. Carboplatin and pemetrexed with or without pembrolizumab for advanced, non-squamous non-small-cell lung cancer: a randomised, phase 2 cohort of the open-label KEYNOTE-021 study. Lancet Oncol 2016;17:1497-508. [Crossref] [PubMed]
- Rittmeyer A, Barlesi F, Waterkamp D, et al. Atezolizumab versus docetaxel in patients with previously treated non-small-cell lung cancer (OAK): a phase 3, open-label, multicentre randomised controlled trial. Lancet 2017;389:255-65. [Crossref] [PubMed]
- Gettinger S, Horn L, Jackman D, et al. Five-Year Follow-Up of Nivolumab in Previously Treated Advanced Non-Small-Cell Lung Cancer: Results From the CA209-003 Study. J Clin Oncol 2018;36:1675-84. [Crossref] [PubMed]
- Forde PM, Smith KN, Chaft JE, et al. NSCLC, early stage Neoadjuvant anti-PD1, nivolumab, in early stage resectable non-small-cell lung cancer. Ann Oncol 2016.27.
- Chaft JE, Hellmann MD, Velez MJ, et al. Initial Experience With Lung Cancer Resection After Treatment With T-Cell Checkpoint Inhibitors. Ann Thorac Surg 2017;104:e217-8. [Crossref] [PubMed]
- Bott MJ, Cools-Lartigue J, Tan KS, et al. Safety and Feasibility of Lung Resection After Immunotherapy for Metastatic or Unresectable Tumors. Ann Thorac Surg 2018;106:178-83. [Crossref] [PubMed]
- Forde PM, Chaft JE, Smith KN, et al. Neoadjuvant PD-1 Blockade in Resectable Lung Cancer. N Engl J Med 2018;378:1976-86. [Crossref] [PubMed]


