Hemoglobin in normal range, the lower the better?—Evidence from a study from Chinese community-dwelling participants
Introduction
Cardiovascular disease is the leading cause of mortality in the world, which accounts for about 30% of all causes of deaths. Of these deaths, high blood pressure is regarded as the most important risk factor and underlying cause of cardiovascular disease (1-3). Furthermore, such risk factors as high level of serum total cholesterol (TC), triglycerides (TG), low-density lipoprotein cholesterol (LDL-C), uric acid (UA) and diabetic mellitus contributed greatly to the development of the cardiovascular disease. Therefore, to maintain the blood pressure values at an appropriate level and decrease the risk factors to the minimal level are especially important. And it is imperative for us to obtain enough knowledge about factors that are associated with blood pressure or those cardiovascular risk factors.
Previous reports indicate that systolic blood pressure (SBP) and diastolic blood pressure (DBP) may increase with increasing hemoglobin (Hb) levels not only in hypertensive patients, but also in healthy patients (4,5). In addition, increased Hb values often accompany insulin resistance and compensatory hyperinsulinemia in humans (6-8). Conversely, anemia has also been suggested to be responsible for insulin resistance (9), thus suggesting a reasonable postulation that J- or U-shaped relationship might exist between the level of Hb and other cardiovascular risk factors. However, to our knowledge, studies that demonstrate a relationship between hematological parameters such as Hb and blood pressure and other cardiovascular risk factors are very few. And drawbacks of these earlier studies were too small individuals included or the lack of adjustment for potential confounding factors, such as age, gender and heart rate (4,10). In that, this study aimed to investigate the relationship between Hb and the traditional cardiovascular risk factors such as hypertension, hyperglycemia, and dyslipidemia by using cross-sectional data in large community-dwelling subjects.
Materials and methods
Subjects
Participants were recruited at the time of their health examination in a single community. All of the visits in the period from Jun. 1, 2012, to Nov. 30, 2012, were eligible for inclusion in the study. Information on medical history, present conditions, and drugs was obtained by interview. All of enrolled participants have no knowledge of their blood pressure previously and none of them had received any anti-hypertension medication before enrollment. During the physical examination, TC, TG, LDL-C, high-density lipoprotein cholesterol (HDL-C), fasting plasma glucose (FPG) and UA were measured. Eligibility criteria include a body weight ≥40 kg, regular pulse, an SBP of ≥90 and ≤200 mmHg and a DBP of ≥50 and ≤110 mmHg, and an Hb level of ≥84 mmol/L for men and ≥78 g/L for women.
Blood pressure measurements
Blood pressure measurements were obtained by manual auscultation with a mercury-gravity manometer via a standardized protocol by trained physicians. Three blood pressure readings were obtained after the participant had been seated, with feet on the ground and back supported, and resting quietly for ≥5 minutes. Each reading was obtained 30 seconds apart, and a fourth reading was obtained if ≥1 of the previous readings had been interrupted (11,12). Mean SBP and DBP for each participant were calculated from the recorded readings. Because we only obtained blood pressure measurements at a single study visit, and thus, a formal diagnosis of hypertension is not possible, participants were characterized as having “elevated blood pressure” if the mean SBP ≥140 mmHg and/or DBP ≥90 mmHg, and “normal blood pressure” if the mean SBP/DBP were <140/90 mmHg. Furthermore, we recorded such information as date of birth, sex, height and weight. We calculated the body mass index (BMI) by dividing weight (in kilograms) by height squared (in meters squared). All of the participants gave written informed consent before they were included in the study.
Biochemical analysis
Hyperuricemia was defined as serum UA ≥420 μmol/L in men or ≥360 μmol/L in women (13). Diabetes was defined as FPG ≥7.0 mmol/L, and/or diabetes history with an antidiabetic drug treatment. Impaired fasting glucose (IFG) was defined as subjects without previously confirmed or treated diabetes but with FPG from 5.6 to below 7.0 mmol/L. General obesity was defined as BMI ≥25 kg/m2. Dyslipidemia was defined as subjects with TG level ≥1.7 mmol/L and/or high TC ≥5.2 mmol/L (14).
Statistical analysis
All data analyses were conducted using SPSS 13.0. Pearson χ2 test was used for the comparison of categorical variables, and continuous data was assessed using analysis of variance (ANOVA). All values are expressed as mean ± standard deviation (SD), unless otherwise specified. Differences based on quartiles of Hb status within gender were analyzed by one-way ANOVA or Kruskal-Wallis H test. Correlation analysis was used for continuous variables between Hb level and various confounding cardiovascular risk factors including blood pressure with adjustment of age. Binary logistic regression analysis was used to determine the factors associated with blood pressure in the entire population, and the results are presented with p for trend. Statistical significance was set at a two-tailed P<0.05.
Results
Baseline characteristics
The subjects comprised 4,851 men and 4,186 women, and all the patients were divided into six groups based on their Hb levels and categorized by gender. The individuals were divided into the following groups according to the quartiles of Hb status and gender. Men: Group 1, ≤119 g/L; Group 2, 120-129 g/L; Group 3, 130-139 g/L; Group 4, 140-149 g/L; Group 5, 150-159 g/L; and Group 6, ≥160 g/L. Women: Group 1, ≤109 g/L; Group 2, 110-119 g/dL; Group 3, 120-129 g/L; Group 4, 130-139g/L; Group 5, 140-149 g/L; and Group 6, ≥150 g/L. Both in men and woman, the Hb level in 6th group were above the upper limit of normal range and the level of Hb in 1th group was under the normal range. The whole patients were evaluated at baseline and found to be eligible for the present analysis. The demographic characteristics of these people are summarized in Table 1.

Full table
Associations of blood pressure and other cardiovascular risk factors with the titre of Hb
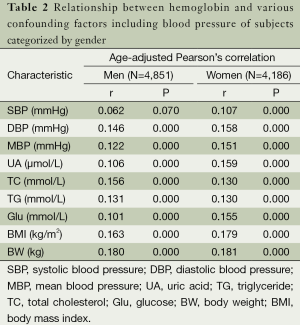
Table 2 shows that whether in men or women, elevated Hb levels were positively associated with DBP, MBP, UA, TC, TG, fasting GLU, BMI and age (P=0.00 from 1st tertile to the highest Hb level). Meanwhile, no significant difference in SBP level was observed among the groups of Hb in men (P=0.14). Furthermore, the incidence of hyperuricemia and obesity gradually increased with the increase level of Hb, and Chi-square test demonstrated that significant difference can be seen in different Hb groups (both P=0.00 in women and men for hyperuricemia and obesity). Those benefits, however, seem to be disappeared in patients with anemia.
Full table
The relationship of blood pressure and other risk factors including Hb
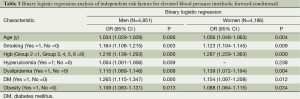
To evaluate the association between Hb and the blood pressure, the enrolled individuals were divided into two group of normal and elevated blood pressure group (described in subjects and data collection section). The binary logistic regression analysis demonstrated that whether in men or women, the level of Hb was an important independent risk factor for elevated blood pressure (OR =1.216; 95% CI: 1.138-1.293, P=0.000 in men; OR =1.287; 95% CI: 1.229-1.363, P=0.000 in women), as shown in Table 3.
Full table
Discussion
The current study for the first time showed that increasing Hb were associated with consistent increased levels of a range of cardiovascular risk factors, including general obesity, adverse lipid profile, higher blood pressure, IFG and high UA and increased blood pressure, and this positive association still can be seen in patients within normal Hb levels.
Some earlier cross-sectional studies found significant Pearson correlations between Hb level and arterial blood pressure, TC and UA in healthy or hypertensive persons. A recent study has demonstrated that Hb level was positively related to the level of blood pressure in a large cohort of healthy blood donors (5). In accordance with their results, our results also demonstrated that the blood pressure is increased with the increasing of Hb level both in SBP and DBP in normal individuals. In addition, our results demonstrated that the level of Hb was an important risk factor for hypertension both in men and women participants, and positive correlation remained between Hb and blood pressure when adjusted with age whether in SBP or DBP in women. Although significant difference between Hb and blood pressure can be observed in our study and reported elsewhere, the exact mechanisms for Hb lead to an elevated blood pressure are not entirely known. Present viewpoints indicate that Hb can have direct or indirect effects on vascular system. Studies have demonstrated that several biological mechanisms for the Hb-blood pressure association might partial explain their relationship. Firstly, Hb may be a scavenger of NO, which is produced in endothelial cells. As the NO can relax the muscle cells surroundings the vessel, the changed levels of Hb may then control the blood pressure (15). Furthermore, Hb has been reported to be strongly related to arterial stiffness which, in turn, can increase SBP and DBP (10). Another explanation for blood pressure increase with increased Hb levels would be increased blood viscosity. It has been reported that elevation of hematocrit and Hb levels increases blood viscosity and that increased viscosity partly through an effect on blood pressure may worsen cardiovascular function (16).
Besides with relationship to blood pressure, our study further demonstrated that even modestly elevated levels of Hb were associated with well recognized cardiovascular risk factors such as diabetes mellitus, hypertension and obesity, and the association is a continuum. Interestingly, Kawamoto et al. (10) also found that Hb per se was associated with other confounding factors such as increased BMI, blood pressure, and TG. Furthermore, our results demonstrated that high levels of Hb were associated with high incidence of obesity and hyperuricemia, even the incidence of diabetes mellitus also has the trend to increase with Hb level. Hyperuricemia has been well proved to link to endothelial cells dysfunction, inflammatory cytokines release and thus increase blood pressure, which is an independent predictor for cardiovascular death (17-19). Although the exact mechanisms between such cardiovascular risk factors and the level of Hb remain unknown, we still may tentatively say that slightly decreased level of Hb within normal range may be beneficial to Chinese community-dwellings.
The limitations in our study still should be noted. The first limitation was the cross-sectional nature of the data. We therefore could not assess the temporal relationship between Hb level and the cardiovascular risk factors. Furthermore, Hb levels and blood pressure values were measured within the same visits. Consequently, drawing conclusions about causality is difficult. However compared to most previous studies, our study has a large sample size, allowing the data to be analyzed separately for men and women. We also controlled for a wide range of potential confounders. In conclusion, there was a significant dose-response association between a wide range of cardiovascular risk factors, especially the blood pressure with Hb level even in subjects with both normal blood pressure and normal Hb levels. Therefore, further studies are thus warranted to quantify the clinical significance in those subjects with high Hb state.
Acknowledgements
This work was supported by the National Natural Science Foundation of China (NSFC 30900602, Junhong Wang) and National Natural Science Foundation of Jiangsu Province (SBK2012879 to Junhong Wang, BK2012648 to Hui Wang and BK2011382 to Yan Guo); Dr. Junhong Wang was also supported by the Chinese Scholar Council (CSC) and “Sixth-Peak Talent” of Jiangsu Province (2013WSN-036).
Disclosure: The authors declare no conflict of interest.
References
- Lawes CM, Vander Hoorn S, Rodgers A, et al. Global burden of blood-pressure-related disease, 2001. Lancet 2008;371:1513-8. [PubMed]
- Brook RD, Appel LJ, Rubenfire M, et al. Beyond medications and diet: alternative approaches to lowering blood pressure: a scientific statement from the american heart association. Hypertension 2013;61:1360-83. [PubMed]
- Cheng HM, Chuang SY, Sung SH, et al. Derivation and validation of diagnostic thresholds for central blood pressure measurements based on long-term cardiovascular risks. J Am Coll Cardiol 2013;62:1780-7. [PubMed]
- Göbel BO, Schulte-Göbel A, Weisser B, et al. Arterial blood pressure. Correlation with erythrocyte count, hematocrit, and hemoglobin concentration. Am J Hypertens 1991;4:14-9. [PubMed]
- Atsma F, Veldhuizen I, de Kort W, et al. Hemoglobin level is positively associated with blood pressure in a large cohort of healthy individuals. Hypertension 2012;60:936-41. [PubMed]
- Barbieri M, Ragno E, Benvenuti E, et al. New aspects of the insulin resistance syndrome: impact on haematological parameters. Diabetologia 2001;44:1232-7. [PubMed]
- Choi KM, Lee J, Kim YH, et al. Relation between insulin resistance and hematological parameters in elderly Koreans-Southwest Seoul (SWS) Study. Diabetes Res Clin Pract 2003;60:205-12. [PubMed]
- Ellinger VC, Carlini LT, Moreira RO, et al. Relation between insulin resistance and hematological parameters in a Brazilian sample. Arq Bras Endocrinol Metabol 2006;50:114-7. [PubMed]
- Ozdemir A, Sevinç C, Selamet U, et al. Age- and body mass index-dependent relationship between correction of iron deficiency anemia and insulin resistance in non-diabetic premenopausal women. Ann Saudi Med 2007;27:356-61. [PubMed]
- Kawamoto R, Tabara Y, Kohara K, et al. A slightly low hemoglobin level is beneficially associated with arterial stiffness in Japanese community-dwelling women. Clin Exp Hypertens 2012;34:92-8. [PubMed]
- Jin YL, Zhu T, Xu L, et al. Uric acid levels, even in the normal range, are associated with increased cardiovascular risk: the Guangzhou Biobank Cohort Study. Int J Cardiol 2013;168:2238-41. [PubMed]
- Preda C, Duhamel A, Picavet M, et al. Tools for statistical analysis with missing data: application to a large medical database. Stud Health Technol Inform 2005;116:181-6. [PubMed]
- Qiu L, Cheng XQ, Wu J, et al. Prevalence of hyperuricemia and its related risk factors in healthy adults from Northern and Northeastern Chinese provinces. BMC Public Health 2013;13:664. [PubMed]
- Thomas GN, Jiang CQ, McGhee SM, et al. Association of vascular risk factors with increasing glycemia even in normoglycemic subjects in an older Chinese population: the Guangzhou Biobank Cohort Study. Metabolism 2006;55:1035-41. [PubMed]
- Cabrales P, Han G, Nacharaju P, et al. Reversal of hemoglobin-induced vasoconstriction with sustained release of nitric oxide. Am J Physiol Heart Circ Physiol 2011;300:H49-56. [PubMed]
- Lowe GD, Lee AJ, Rumley A, et al. Blood viscosity and risk of cardiovascular events: the Edinburgh Artery Study. Br J Haematol 1997;96:168-73. [PubMed]
- Kanbay M, Huddam B, Azak A, et al. A randomized study of allopurinol on endothelial function and estimated glomular filtration rate in asymptomatic hyperuricemic subjects with normal renal function. Clin J Am Soc Nephrol 2011;6:1887-94. [PubMed]
- Jin M, Yang F, Yang I, et al. Uric acid, hyperuricemia and vascular diseases. Front Biosci (Landmark Ed) 2012;17:656-69. [PubMed]
- Gür M, Sahin DY, Elbasan Z, et al. Uric acid and high sensitive C-reactive protein are associated with subclinical thoracic aortic atherosclerosis. J Cardiol 2013;61:144-8. [PubMed]


