Thoracic ultrasound versus artificial pneumothorax in complications of medical thoracoscopy—a propensity score matching analysis
Introduction
Medical thoracoscopy which is defined as the thoracoscopy with intravenous sedation combining local anesthesia, is now widely used in clinical medicine. One of the most important contraindication of medical thoracoscopy is extensive pleural adhesion (1). Therefore, evaluation and location of the approaches is the key step. And the previous standard for the step in many countries is artificial pneumothorax (AP) (2-4), which is complained with the risks of radiation exposure, air embolism and so on (5). Recently, thoracic ultrasound (TU) has been considered as one of the choices to evaluate pleural adhesions and locate approaches for the development of technology (6). The aim of this study was to investigate the complications of medical thoracoscopy locating approach with AP comparing TU.
Methods
Patients and investigations
A total of 108 patients who underwent medical thoracoscopy in Peking University First Hospital were all retrospectively observed from January 2011 to April 2017, including 92 patients of the AP group and 16 patients of the TU group. The indications of the operations were diagnostic intent, which have conformed to the guideline of British Thoracic Society published in 2010 (2). All the subjects were hospitalized in our department, and had been taken medical histories, routine blood tests, chest computed tomography (CT) scans, etc. The patients were closely monitored during and after the operations, and the complications were recorded as follows: prolonged air leak, hemorrhage requiring treatment, operative incision disunion, mediastinal/subcutaneous emphysema requiring treatment, empyema, respiratory infection, respiratory failure, lung laceration, incision metastasis, local neurovascular injury, acute cerebrovascular event, acute cardiovascular event and death within 28 days after the operations. All patients had signed the informed consent before the operations.
AP
In the AP group, the pleural effusion was removed as much as possible before injecting room air or carbon dioxide. Then a chest X-ray was performed immediately to evaluate the pleura adhesion and determine the location of approach. When the chest X-ray didn’t show the extrapulmonary air located inside the pleural cavity, the making pneumothorax step should be repeated (2,7).
TU
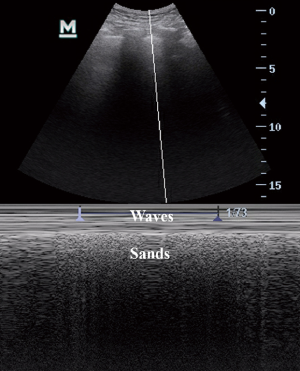
In the TU group, we used an ultrasound machine (U.S. General Electric Company, Venue 50) with convex (3.5 MHz) and linear (7.5 MHz) probes (8). The thoracic ultrasonography was performed two times in each patient by the same operator. The first time on the day before medical thoracoscopy in the bed-ward was to evaluated systematically with ultrasound the dorsal, lateral, and anterior chest wall. The operator detected pleural adhesion, measured the depth of pleural effusion, looked for “sliding sign” (Figure 1) and “seashore sign” (Figure 2) by convex probes, measured the thickness of chest wall and the distribution of blood vessels by linear probe. The initial selected points of approach should be got. When the patient was resting on the healthy side position and fixed by decubitus fixation instrument in the operating room, the position might have a little different from that in the bed-ward. As a result, the second TU was performed to detect the initial selected points to identified the finial ideal approach.

Medical thoracoscopic technique
All subjects had received medical thoracoscopy as follows. Local anesthesia was induced by injection 2% lidocaine with or without midazolam administered through intravenous line. After premedication, we made a small skin incision to gently introduced curved blunt-point scissors following a medical thoracoscopic trocar into the chest wall as far as the pleural space. Then room air was allowed spontaneously to enter the pleural space with consequent lung collapse. We used a rigid thoracoscope (Germany, Karl Storz GmbH & Co) or semi-rigid thoracoscope (Japan, Olympus Corporation) to take the residual effusion until the pleural cavity was emptied. The lung and pleura were observed, and biopsies were taken in each subject. Other procedures might be performed depends on different cases, while talc poudrage were performed in no one.
Statistical analysis
All statistical analyses were processed by the SPSS for windows, version 22.0 (SPSS Inc., Chicago, IL, USA) software. The continuous variables were described as mean and standard deviations (SD), and compared using the independent sample t-test. The discrete variables were described as frequencies and proportion, and compared using the Pearson χ2-test or Fisher’s exact test. Propensity score matching (PSM) was used to balance the covariance with 2:1 matched between the two groups. A P-value of less than 0.05 was deemed significant.
Results
A total of 108 subjects were recruited with mean age of 65 (SD ±9; range, 37–84) years, and 71 (65.7%) subjects were males. As regards smoking, 36 (33.3%) cases were current smokers, 26 (24.1%) cases were former smokers, and 46 (42.6%) cases had no history of smoking. Malignant pleural disease was diagnosed in 60 (55.6%) cases, and benign pleural disease was diagnosed in 48 (44.4%) cases. Ninety-two subjects were in the AP group, 16 subjects were in the TU group, and there was significant difference in ages between the two groups (P=0.032). The details are shown in Table 1.
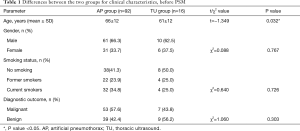
Full table
The total rate of complications was 7.4% (n=8), with one case in the TU group, and seven cases in the AP group. No death within 28 days was related to the procedure. In two cases, there were two or more complications being observed. They were respiratory infection and acute cerebrovascular event suspected air embolism in one case, and respiratory infection complicated with respiratory failure in the other. There was no significant difference in the rate of complications between the two groups (P=0.848). The details are shown in Table 2.

Full table
PSM was used to balance the covariance between the two groups. With 2:1 matched, the overall complication rate was 9.4% (3/32) in the AP group, comparing 6.2% (1/16) in the TU group. There was still no significant difference between the two groups (P=0.712). The details are shown in Table 3.

Full table
Acute cerebrovascular event suspected air embolism was observed in one case of the AP group. The patient had suffered from suddenly disorders on movement and speech. The cerebrovascular computed tomography angiography (CTA) scan showed newly onset multiple cerebral infarction and filling defect in the vessels with the CT value similar with air’s. Fortunately, the patient had been fully recovered within 2 weeks. Furthermore, there were three cases had to repeat the making pneumothorax step, because the chest X-ray didn’t show the extrapulmonary air located inside the pleural cavity. The reason was considered as the rapid absorption of carbon dioxide for making the AP.
Discussion
Previously reported in the literatures, the complication rate of medical thoracoscopy was 6.3–16.5%, and the mortality was 0.00–0.54% (2,9,10). The complications related to the approach procedure are including lung laceration, hemorrhage, local neurovascular injury, subcutaneous emphysema, and so on (11). Being one of the key steps in medical thoracoscopy, the approach procedure has potential impact on other complications such as acute cardiovascular events. Therefore, the improvement of locating approach methods may help to reduce the incidence of complications.
AP is the previous standard for evaluating and locating approach in medical thoracoscopy, while real-time observation is not available and the risk of radiation exposure is unavoidable (12). By contrast, the advantages of TU are real-time imaging on bedside and, of course, without risk of radiation exposure (13). At the meantime, the capacity of TU for evaluating and locating approach had been fully confirmed recently. TU can well identify the nature of pleural effusion like hemothorax and empyema (14-16). Even if the pneumothorax occurs, TU can also be a good assessment instrument because of some special signs such as the absence of “lung point” and “sliding sign” (17-19). Besides, a cohort study had showed a strong tend to reduction in single port medical thoracoscopy pleural approach failure with TU comparing AP (20).
However, TU is not flawless. Some of the areas are difficult to visualize because of the bony chest cage (21). Furthermore, the ultrasound wave cannot travel through air. As a result, bullae or extensive subcutaneous air make TU hard to examine the pleural (8). Another limitation is that ultrasound image prefers experienced operators (22).
On the other hand, there are different opinions in the specific application of TU for evaluating approach. Some authors advocated TU following by AP to prevent the occurrence of lung laceration (9). However, another study had showed that TU could guide medical thoracoscopy approach without pneumothorax even in the complete absence of pleural effusion (23).
While there was spare data in investigating the complications of locating approach with AP comparing TU. After PSM analysis, the overall complication rate of the TU group was a little less than that of the AP group in our study, without significant difference (TU group vs. AP group, 6.2% vs. 9.4%, P=0.712). We should be noticed that cases of acute cerebrovascular suspected air embolism and repeating making pneumothorax step were observed in the AP group, which could be prevented by TU. Moreover, we used high frequency linear probe to provide definition of chest wall’s superficial structures like nerve and blood vessel. This step may reduce the risk of local neurovascular injury.
Conclusions
We believe that our study suggests that TU is a locating approach method which does not increase the complication rate comparing with AP. And it could be a good choice in medical thoracoscopy.
Acknowledgements
We would like to thank the nurses who helped operating medical thoracoscopy in Peking University First Hospital. We would also like to thank Pengkang He, MD, of Peking University First Hospital for linguistic advice.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: All patients provided written informed consent, and this study was approved by the Ethical Committee of Peking University First Hospital under approval number 2016[1130].
References
- Lee P, Colt HG. Pleuroscopy in 2013. Clin Chest Med 2013;34:81-91. [Crossref] [PubMed]
- Rahman NM, Ali NJ, Brown G, et al. Local anaesthetic thoracoscopy: British Thoracic Society pleural disease guideline 2010. Thorax 2010;65 Suppl 2:ii54-60. [Crossref] [PubMed]
- Loddenkemper R. Thoracoscopy-state of the art. Eur Respir J 1998;11:213-21. [Crossref] [PubMed]
- Jing FG, Li SY, Li WP, et al. The expert consensus of medical thoracoscopy. Chin J Lung Dis 2018;11:6-13. (electronic edition).
- Casal RF, Eapen GA, Morice RC, et al. Medical thoracoscopy. Curr Opin Pulm Med 2009;15:313-20. [Crossref] [PubMed]
- Medford AR. Additional cost benefits of chest physician operated thoracic ultrasound (TUS) prior to medical thoracoscopy (MT). Respir Med 2010;104:1077-8. [Crossref] [PubMed]
- Light RW. Thoracoscopy. In: Pleural diseases. Sixth edition. Philadelphia: Lippincott Williams & Wilkins, 2012:481.
- Shojaee S, Argento AC. Ultrasound-guided pleural access. Semin Respir Crit Care Med 2014;35:693-705. [PubMed]
- Adv Med 2016;2016:3794791. Safety and Complications of Medical Thoracoscopy. Adv Med 2016;2016. [PubMed]
- Czarnecka K, Yasufuku K. Interventional pulmonology: focus on pulmonary diagnostics. Respirology 2013;18:47-60. [Crossref] [PubMed]
- Shojaee S, Lee HJ. Thoracoscopy: medical versus surgical-in the management of pleural diseases. J Thorac Dis 2015;7:S339-51. [PubMed]
- Brenner DJ, Hall EJ. Computed tomography--an increasing source of radiation exposure. N Engl J Med 2007;357:2277-84. [Crossref] [PubMed]
- Bhatnagar R, Corcoran JP, Maldonado F, et al. Advanced medical interventions in pleural disease. Eur Respir Rev 2016;25:199-213. [Crossref] [PubMed]
- Tu CY, Hsu WH, Hsia TC, et al. Pleural effusions in febrile medical ICU patients: chest ultrasound study. Chest 2004;126:1274-80. [Crossref] [PubMed]
- Sajadieh H, Afzali F, Sajadieh V, et al. Ultrasound as an alternative to aspiration for determining the nature of pleural effusion, especially in older people. Ann N Y Acad Sci 2004;1019:585-92. [Crossref] [PubMed]
- Marcun R, Sustic A. Sonographic evaluation of unexplained pleural exudate: a prospective case series. Wien Klin Wochenschr 2009;121:334-8. [Crossref] [PubMed]
- Soldati G, Testa A, Sher S, et al. Occult traumatic pneumothorax: diagnostic accuracy of lung ultrasonography in the emergency department. Chest 2008;133:204-11. [Crossref] [PubMed]
- Rowan KR, Kirkpatrick AW, Liu D, et al. Traumatic pneumothorax detection with thoracic US: correlation with chest radiography and CT-initial experience. Radiology 2002;225:210-4. [Crossref] [PubMed]
- Alrajhi K, Woo MY, Vaillancourt C. Test characteristics of ultrasonography for the detection of pneumothorax: a systematic review and meta-analysis. Chest 2012;141:703-8. [Crossref] [PubMed]
- Medford AR, Agrawal S, Bennett JA, et al. Thoracic ultrasound prior to medical thoracoscopy improves pleural access and predicts fibrous septation. Respirology 2010;15:804-8. [Crossref] [PubMed]
- Mathis G. Thoraxsonography--Part 1: Chest wall and pleura. Praxis (Bern 1994) 2004;93:615-21.
- Mayo PH, Beaulieu Y, Doelken P, et al. American College of Chest Physicians/La Société de Réanimation de Langue Française statement on competence in critical care ultrasonography. Chest 2009;135:1050-60. [Crossref] [PubMed]
- Marchetti G, Valsecchi A, Indellicati D, et al. Ultrasound-guided medical thoracoscopy in the absence of pleural effusion. Chest 2015;147:1008-12. [Crossref] [PubMed]


