Is the new distribution of early esophageal adenocarcinoma stages improving the prognostic prediction of the 8th edition of the TNM staging system for esophageal cancer?
Introduction
In the past, pathological staging after esophagectomy was the gold standard for the staging of esophageal tumors. Nowadays, the pathological stage is losing its clinical relevance because adjuvant therapy is gradually replacing simple esophagectomy in patients with advanced cancer (1). However, pathological staging is still closely related to the stage and prognosis of early cancer. In 2017, the latest 8th edition of the TNM staging system was released, and the previous common staging system is no longer used. The clinical, pathological and neoadjuvant pathological groups were separately staged (2,3). For pathological TNM staging, in stage I, pT1 was divided into pT1a and pT1b for subgroup analysis in both adenocarcinoma and squamous cell carcinoma. In addition, the updated pTNM staging system for esophageal adenocarcinoma also separated the original stage IA in the 7th edition (pT1N0M0 G1–2) into stage IA (pT1aN0M0 G1) and IB (pT1aN0M0 G2 and pT1bN0M0 G1–2) and the original stage IB to stage IC (pT1N0M0 G3 and pT2N0M0 G1–2).
Each update in the TNM staging system is usually accompanied by substantial skepticism. After the 7th edition of the staging system was updated for esophageal tumors, many studies proposed that the new staging system does not provide good differentiation of survival outcomes between adjacent stages (4-6). The American Joint Committee on Cancer (AJCC)/Union for International Cancer Control (UICC) subsequently makes corresponding adjustments based on the feedback. The changes in the eighth edition are also based on numerous clinical studies conducted to assess the seventh edition (7-9).
The large amount of patient data contained in the Surveillance, Epidemiology, and End Results (SEER) database can be a powerful tool for exploring early esophageal cancer outcomes. Therefore, to verify whether the new staging strategy for early esophageal adenocarcinoma is feasible, we used the SEER database (From 2004 to 2014) for retrospective analysis. In this study, our target was to provide an in-depth understanding of the treatment outcomes of early esophageal adenocarcinoma and to clarify whether the 8th edition of the staging system adequately reflects the prognosis of patients with early esophageal adenocarcinoma.
Methods
Patients were selected from the SEER program. The current SEER project is a population-based cancer registry sponsored by the National Cancer Institute. The SEER project has collected clinicopathologic data for 18 specified areas of the United States (US) since 1972 and includes 17 population-based cancer registries, representing approximately 28% of the US population.
According to the 8th edition of the TNM staging system for esophageal cancer, we selected all patients with histologically diagnosed stage IA (pT1aN0M0 G1), IB (pT1aN0M0 G2 and pT1bN0M0 G1–2), and IC (pT1N0M0 G3 and pT2N0M0 G1–2) cancer from 2004 to 2014, using the 8th edition TNM staging classification system for esophageal cancer. Patients were enrolled based on the following inclusion criteria: pathologically confirmed adenocarcinoma and presence of a primary tumor. Patients were excluded if they had received neoadjuvant therapy.
Baseline data including patient information (age, race/ethnicity and sex), tumor characteristics (location, size, and histology) and surgical type were obtained from the SEER program. Outcomes evaluated in this study included overall survival (OS) and esophageal cancer-specific survival (ECSS), which were collected from the SEER database through December 31, 2014. OS and ECSS were defined as the interval from diagnosis until death from any cause and death as a result of esophageal cancer, respectively.
Statistical analysis
All continuous and categorical variables with normal distributions were analyzed for heterogeneity using one-way ANOVA with multiple comparisons post hoc test and the Chi-square test. The Kruskal-Wallis test was used in analyzing data with non-normal distribution with adjustments for multiple comparisons. Survival curves were estimated by the Kaplan-Meier method and compared with the log-rank test. Cox regression analysis was performed to calculate hazard ratios (HRs) and 95% confidence intervals (CIs). After univariate analysis, risk factors with a P value <0.1 were selected for the multivariate model. A two-sided P value <0.05 was considered statistically significant. All analyses were performed using SPSS 22.0 (SPSS, Chicago, IL, USA) and GraphPad Prism 7.0 (GraphPad Software, San Diego, CA, USA). The study was approved by the ethics committee of Nanjing Drum Tower Hospital, the affiliated hospital of Nanjing University Medical School (2017-175-01).
Results
According to the 8th edition of the TNM staging system, we divided patients into the following three groups: IA (n=84), IB (n=386), and IC (n=244). All patients underwent local resection or surgical resection. However, the accurate surgical method was not explicitly listed in the SEER database. Other than the gradual increase in tumor size with stage (15.68±11.34 vs. 18.82±13.48 vs. 24.48±15.64 mm, P<0.01), there was no difference in other baseline parameters (Table 1).

Full table
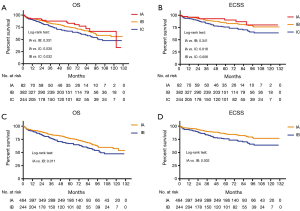
We next compared the OS and ECSS based on the two editions. The follow-up duration was 1–131 months. Two stage IA patients and 4 stage IB patients were not included in follow-up because of in-hospital deaths or insufficient follow-up time. In the 8th edition, there was no significant difference between groups IA and IB in OS (P=0.331) or ECSS (P=0.341) (Figure 1A,B). However, the survival rates of these two groups were significantly higher than those of group IC. In the 7th edition, both OS (P=0.011) and ECSS (P=0.002) rates of patients with stage IA disease were significantly higher than those of patients with stage IB disease (Figure 1C,D).
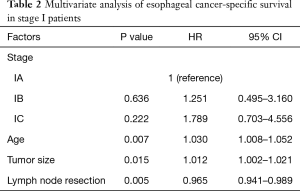
The multivariate Cox regression analysis also confirmed that the use of the new staging system was not a risk factor for the prognosis of early esophageal cancer (IB: HR =1.251, 95% CI: 0.495–3.160; IC: HR =1.789, 95% CI: 0.703–4.556) (Table 2). Older age (HR =1.030, 95% CI: 1.008–1.052) and larger tumor diameter (HR =1.012, 95% CI: 1.002–1.021) were predictors of unfavorable prognosis, and a high number of resected lymph nodes (HR =0.965, 95% CI: 0.941–0.989) was a significant indicator of favorable prognosis.
Full table
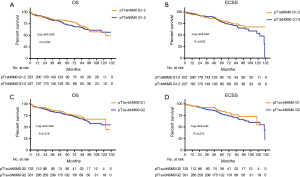
We next investigated whether there is a better method for the further refinement of stage IA tumors (T1N0M0 G1–2) in the 7th edition. To this end, we conducted further analyses on the staging system. We used two different staging methods, namely, pT1aN0M0 G1–2 vs. pT1bN0M0 G1–2 (Figure 2A,B), distinguished by the T stage, and pT1a+bN0M0 G1 vs. pT1a+bN0M0 G2, based on the degree of differentiation (Figure 2C,D). However, after separate analysis of OS and ECSS, we found no significant difference in either of the staging methods.
Discussion
In recent years, significant progress has been made in the prevention and treatment of early esophageal cancer. With continuous breakthroughs in the endoscopic treatment of gastrointestinal diseases, we have more knowledge about early esophageal cancer. The 7th edition of the TNM staging system was published in 2010. However, in the clinical application of this staging system over the years, several defects were found (10). Therefore, the 8th edition adjusted staging compared with that in the 7th edition, especially in both early esophageal squamous cell carcinoma and adenocarcinoma. The T1 stage of esophageal squamous cell carcinoma was further divided into T1a and T1b stages, and stage IA adenocarcinoma was divided into stage IA and IB (2). Zhang et al. (11) compared the 7th and 8th editions of the AJCC/UICC TNM staging system for esophageal squamous cell carcinoma patients who received radiotherapy and found that the 8th edition was superior to the 7th edition. The 8th edition better predicted 5-year survival rate of patients with stage IA disease (100%) than the 7th edition, while the prognosis of stage IA disease according to the 7th edition was similar to that of stage IB disease (89.0% vs. 87.0%). Therefore, the new staging system may be practical for use in early esophageal squamous cell carcinoma. Nevertheless, the use of the new staging system seemed unsuitable for early adenocarcinoma according to our study. The data from the SEER database did not indicate an advantage of using the new staging system for early esophageal adenocarcinoma. Neither the OS nor ECSS showed convincing differentiation based on the new stage IA and IB classification.
In the 8th edition of the AJCC/UICC TNM staging system for esophageal adenocarcinoma, pT1aN0M0 G1 is listed as a separate earliest stage, indicative of a favorable long-term survival rate. In contrast, pT1aN0M0 G2 and pT1bN0M0 G1–2 disease are considered to have relatively poor prognosis. This reflects the emphasis on the histological grading of early tumors. However, in the 7th edition, the histological grade had already been considered as a factor for staging—pT1N0M0 G1 esophageal squamous cell carcinoma is classified as stage IA, and pT1N0M0 G2–3 as stage IB. Nevertheless, Chen et al. (12) found no significant difference in long-term survival rates between the two patient groups. In addition, Situ et al. (13,14) conducted single-center retrospective analysis of T2N0M0 and T3N0M0 esophageal squamous cell carcinoma and found that histological grade was a prognostic factor. Kim et al. (6) analyzed gastric cardia adenocarcinoma and proposed to completely remove the histological grade from the staging system because of its lack of effect on prognosis. Similarly, histological grading is not an important aspect in Japanese esophageal cancer guidelines (15,16). Instead, these guidelines pay more attention to tumor location because of the ability of this parameter to more precisely detect the state of tumor spread (17). In our study, for patients with pT1a–bN0M0 and G1–2 esophageal adenocarcinoma, in addition to the 8th edition staging, we tried two new staging methods, namely, pT1a vs. pT1b and G1 vs. G2. Analysis of long-term survival rates revealed the lack of clear distinction between the two staging methods. These results also demonstrate that further classification of stage IA in the 7th edition may not be a good option after all.
Potential lymph node micrometastasis of early esophageal tumors may also be a risk factor for prognosis. Gertler et al. (5) proposed that the risk of lymph node metastasis differs between pT1a and pT1b tumors (1.4% vs. 20.0%), and Newton et al. (18) presented similar results (3.6% vs. 23.4%). The high metastatic risk of pT1b may also be accompanied by clinically undetectable micrometastases, which may explain the poor survival of patients with pT1b tumors. Tachibana et al. (19) reported their findings on pT1 and pT2 esophageal squamous cell carcinoma patients who were undergoing esophagectomy, and based on their results, in patients with negative lymph nodes metastasis, the cancer-specific survival rates for pT1 and pT2 tumors were similar. Similarly, in our attempted T1a vs. T1b classification, there was no significant difference in survival rates. Weksler et al. (20) constructed a new tumor risk model and found that the lack of difference in prognosis is probably because T1b patients can be further divided into two different cohorts with high and low risk of lymph node metastasis, and T1b patients with low risk of lymph node metastasis may be combined with T1a patients for the same tumor stage. However, this staging model needs further verification.
Limitations
Our study aimed to detect the effectiveness of the 8th edition of the TNM staging system. Nevertheless, our study has several limitations. First, the SEER database is based on multiple centers, and we were unable obtain the appropriate details on the surgical procedure. Different surgeons and surgical methods may have a significant impact on the assessment of lymph node metastasis and disease prognosis. Second, the data were obtained over a long duration, and radiotherapy and chemotherapy strategies may have greatly changed over that period. Furthermore, our exclusion of all patients who received neoadjuvant treatment may have had an impact on the final results.
Conclusions
We used the SEER database to compare the 7th and 8th editions of the AJCC/UICC TNM staging system for early esophageal adenocarcinoma. For patients who received surgery, the 8th edition was not superior to the 7th edition in early esophageal adenocarcinoma.
Acknowledgements
Funding: This work was supported by the National Natural Science Foundation of China (81800241).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the ethics committee of Nanjing Drum Tower Hospital, the affiliated hospital of Nanjing University Medical School (No. 2017-175-01).
References
- Schweigert M, Dubecz A, Stein HJ. Oesophageal cancer--an overview. Nat Rev Gastroenterol Hepatol 2013;10:230-44. [Crossref] [PubMed]
- Rice TW, Ishwaran H, Ferguson MK, et al. Cancer of the Esophagus and Esophagogastric Junction: An Eighth Edition Staging Primer. J Thorac Oncol 2017;12:36-42.
- Rice TW, Gress DM, Patil DT, et al. Cancer of the esophagus and esophagogastric junction-Major changes in the American Joint Committee on Cancer eighth edition cancer staging manual. CA Cancer J Clin 2017;67:304-17.
- Talsma K, van Hagen P, Grotenhuis BA, et al. Comparison of the 6th and 7th Editions of the UICC-AJCC TNM Classification for Esophageal Cancer. Ann Surg Oncol 2012;19:2142-8.
- Gertler R, Stein HJ, Langer R, et al. Long-term outcome of 2920 patients with cancers of the esophagus and esophagogastric junction: evaluation of the New Union Internationale Contre le Cancer/American Joint Cancer Committee staging system. Ann Surg 2011;253:689-98. [Crossref] [PubMed]
- Kim HI, Cheong JH, Song KJ, et al. Staging of adenocarcinoma of the esophagogastric junction: comparison of AJCC 6th and 7th gastric and 7th esophageal staging systems. Ann Surg Oncol 2013;20:2713-20. [Crossref] [PubMed]
- Rice TW, Ishwaran H, Blackstone EH, et al. Recommendations for clinical staging (cTNM) of cancer of the esophagus and esophagogastric junction for the 8th edition AJCC/UICC staging manuals. Dis Esophagus 2016;29:913-9.
- Rice TW, Ishwaran H, Hofstetter WL, et al. Recommendations for pathologic staging (pTNM) of cancer of the esophagus and esophagogastric junction for the 8th edition AJCC/UICC staging manuals. Dis Esophagus 2016;29:897-905.
- Rice TW, Ishwaran H, Kelsen DP, et al. Recommendations for neoadjuvant pathologic staging (ypTNM) of cancer of the esophagus and esophagogastric junction for the 8th edition AJCC/UICC staging manuals. Dis Esophagus 2016;29:906-12.
- Ning ZH, Wang ZG, Chen J, et al. Proposed Modification of Nodal Staging as an Alternative to the Seventh Edition of the American Joint Committee on Cancer Tumor-Node-Metastasis Staging System Improves the Prognostic Prediction in the Resected Esophageal Squamous-Cell Carcinoma. J Thorac Oncol 2015;10:1091-8.
- Zhang D, Zheng Y, Wang Z, et al. Comparison of the 7th and proposed 8th editions of the AJCC/UICC TNM staging system for esophageal squamous cell carcinoma underwent radical surgery. Eur J Surg Oncol 2017;43:1949-55.
- Chen SB, Weng HR, Wang G, et al. Prognostic factors and outcome for patients with esophageal squamous cell carcinoma underwent surgical resection alone: evaluation of the seventh edition of the American Joint Committee on Cancer staging system for esophageal squamous cell carcinoma. J Thorac Oncol 2013;8:495-501.
- Situ D, Wei W, Lin P, et al. Do tumor grade and location affect survival in esophageal squamous cell carcinoma? Survival analysis of 302 cases of pT3N0M0 esophageal squamous cell carcinoma. Ann Surg Oncol 2013;20:580-5. [Crossref] [PubMed]
- Situ D, Wang J, Lin P, et al. Do tumor location and grade affect survival in pT2N0M0 esophageal squamous cell carcinoma? J Thorac Cardiovasc Surg 2013;146:45-51. [Crossref] [PubMed]
- Japan Esophageal S. Japanese Classification of Esophageal Cancer, 11th Edition: part I. Esophagus 2017;14:1-36.
- Japan Esophageal S. Japanese Classification of Esophageal Cancer, 11th Edition: part II and III. Esophagus 2017;14:37-65.
- Udagawa H, Ueno M. Comparison of two major staging systems of esophageal cancer-toward more practical common scale for tumor staging. Ann Transl Med 2018;6:76. [Crossref] [PubMed]
- Newton AD, Predina JD, Xia L, et al. Surgical Management of Early-Stage Esophageal Adenocarcinoma Based on Lymph Node Metastasis Risk. Ann Surg Oncol 2018;25:318-25. [Crossref] [PubMed]
- Tachibana M, Kinugasa S, Dhar DK, et al. Prognostic factors in T1 and T2 squamous cell carcinoma of the thoracic esophagus. Arch Surg 1999;134:50-4. [Crossref] [PubMed]
- Weksler B, Kennedy KF, Sullivan JL. Using the National Cancer Database to create a scoring system that identifies patients with early-stage esophageal cancer at risk for nodal metastases. J Thorac Cardiovasc Surg 2017;154:1787-93. [Crossref] [PubMed]


