
Chronic dyspnoea: finding the cause to reduce mortality
Dyspnea or shortness-of-breath (SOB) is a subjective sensation that is uncomfortable and often results in anxiety when it is felt that the SOB is out of proportion to a given level of exertion (1,2). Furthermore, in the context of this exposition, we are interested in chronic dyspnea—defined as presence of dyspnea for at least one month (3,4). Chronic dyspnea can be detected simply by asking a question and getting a dichotomous (yes/no) response (1) and is generally elicited by questionnaire (1,5). The detection of chronic dyspnea is important as it is associated with a 2-fold greater increase in cardiovascular (3,6,7) and all-cause mortality (3,8,9) over 10 or more years (relative to those without dyspnea). Earlier detection means more timely diagnostic efforts to determine the underlying etiology of dyspnea, and more prompt treatment of the cause with longer survival.
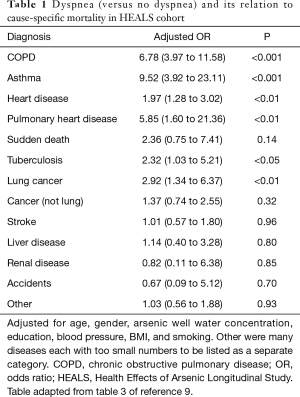
Diseases of the heart and lungs result in most causes of SOB (4,10-14), although psychological diseases (including anxiety) and deconditioning can also result in dyspnea (4,11-14). In addition, obesity has been noted to cause dyspnea in some studies (12,13,15). About two thirds of a dyspnea work-up finds heart and lung disease as the primary cause (3,4,11-14). Another important question asks what are the most likely causes of mortality in those with dyspnea (versus no dyspnea) when followed over time. This has only been determined in one study (9) which is summarized briefly in Table 1. The study followed 11,533 subjects from Bangladesh for 11−12 years and determined cause-specific mortality. If one has baseline dyspnea (versus no dyspnea), the odds are 2.0- to 9.5-fold higher that s/he will die from lung or heart related disease than from any other cause (9), as seen from Table 1. Mortality from stroke, liver disease, renal disease, nonrespiratory cancers, accidents, and others (a mixture of many diseases) was not related to dyspnea. Using COPD as an example, there were 247 excess deaths per 100,000 per year in those with baseline dyspnea relative to those without dyspnea (data from reference 9, table 2). Overall, those with dyspnea at baseline had 1,409 deaths/100,000/year and those without dyspnea had 518 deaths/100,000/year (9). These data illustrate why detection of the cause of dyspnea as early as possible has great potential for reducing long-term mortality.
Full table
Breathlessness is commonly noted slightly more in females than males (16). In adults, as one ages dyspnea prevalence increases. It varied from as low as 2.4% in a population aged 18 and over (1) to 32% in a population aged 70 and older who lived at home (17). Dyspnea was one of the top 10 reasons for being seen in the emergency department (ED) or for seeing a general internist (18,19). When following patients from the ED with dyspnea as the presenting complaint over 10 years (with no history of asthma and no wheezing on clinical exam), there was a 1.37-fold greater mortality compared with the general population (20). Finally, dyspnea, although just a symptom, appears to be a better predictor of mortality over 5 years compared to objective measures of airway obstruction in patients with COPD (21).
With the above overview, Huang et al. (22) have retrospectively determined what happened to 122 consecutive subjects referred from general to specialty clinics with the complaint of chronic dyspnea, defined as dyspnea of at least 8 weeks duration. The dyspnea had to be the primary complaint of the patient, not secondary as one of many other complaints. In addition, the dyspnea could be due to a disease referral to a specialty clinic with COPD, heart failure, etc. where dyspnea is part of the disease process and referral to the clinic is to get better control of the disease (assuming the specialty clinic agrees with the preliminary diagnosis given). In addition, the dyspnea could not be acute or emergent in nature; it had to be chronic as is consistent with a clinic referral. Six months after the referral, determination was made on whether a diagnosis was made (or not). The only two specialty clinics referred to were either cardiology or respiratory disease. Determination of whether a diagnosis for the cause of chronic dyspnea was made was from the specialty clinic as gold standard (22).
The preliminary diagnosis from the referral physician or clearly evident diagnosis was 61% (74/122). Therefore, an unclear diagnosis at referral was 39%. This was the first primary aim of the study (22). However, the fully concordant diagnosis comparing the final diagnosis (by the specialist) with the preliminary evident diagnosis was 26% (32/122). This was determined 6 months after referral to make sure at least one visit (if not more) had occurred to the specialist clinic. Clearly, therefore, referral was important (assuming the subspecialist was correct) since the evident diagnosis was poorly concordant. This would make sense because the specialist clinic has more advanced tests depending on clinical findings to better find the cause of the patient’s dyspnea. If the concordance had been very high this would have suggested that referral is often not necessary. This type of comparison has rarely been done before. Concordance between referral physician and specialist physician was the third primary aim of the study (22).
The 122 subjects with chronic dyspnea had an average age of 63±16 years (22). There were 67 (55%) females and 55 (45%) males. A definitive diagnosis of cause of dyspnea was made in 62% (76/122) of all referred patients. No definitive diagnosis was made in 12/122 or 10% of patients. In 28% (34/122) of patients the diagnosis was not completely certain, even for subspecialists. This illustrates the difficulty in making a definitive diagnosis of the etiology of SOB. Although it is unclear why 38% had no definitive diagnosis, part of the problem may have been related to making only one visit to a specialist clinic. It often requires many visits and serial testing to be sure of a given diagnosis, even for a specialist. In addition, this was an observational study and after referral there was no formal structured work-up required to find the etiology of dyspnea. The determination of a definitive diagnosis was the second primary aim of the study (22).
Given the above study (22), only three previous studies have made a systematic effort to find all diagnosis for people with dyspnea. The first study defined chronic dyspnea as SOB lasting at least 3 weeks and evaluated 100 consecutive patients (85 of whom completed the study) with a primary complaint of chronic dyspnea (11). Five board certified pulmonologists started with a chest-X-ray and then depending on clinical intuition used a battery of tests until a diagnosis was found. The tests included spirometry (with inspiratory loops), lung volumes, methacholine challenge testing (MCT), cardiopulmonary exercise testing (CPET), single-breath diffusion capacity, radionuclide ventriculography, 24-hour esophageal pH study, and cardiac exercise study. If a diagnosis was found early, all the tests were not done. They claimed to have a 100% diagnostic accuracy with a 76% response to treatment based on diagnosis. Two thirds of dyspnea outcomes were due to heart and lung disease (11).
A second study prospectively enrolled 72 patients with unexplained dyspnea of at least one month duration with a nondiagnostic chest-X-ray and normal baseline spirometry (4). This study had a similar standard work-up as the previous (11) until a diagnosis was found with addition of V/Q scan, Holter monitoring, and CT scan of the chest (if needed). As above (11), ECHO of the heart, CPET, and MCT were part of the work-up if needed. Fifty percent of diagnosis were heart or lung disease and 58/72 (81%) had a definitive diagnosis meaning 19% did not have a specific diagnosis (4). A strength of the study was a minimum 1-year follow-up period (up to 8 years in some) to make sure no other diagnosis revealed itself in those without a definitive diagnosis.
A third study prospectively studied 123 patients with at least 8 weeks of unexplained dyspnea and had the most organized and advanced approach (13). The work-up was in three tiers. The initial Tier I work-up included history and physical, CBC, TSH, BNP, full PFTs including MCT, and chest-X-ray. If negative, Tier II work-up included only CPET. Finally, if negative Tier III work-up included CT scan of chest, V/Q scan, bronchoscopy, thoracentesis, cardiac work-up (including stress ECHO, nuclear stress test, and cardiac catheterization if indicated), and upper GI endoscopy and sinus CT scan if indicated as well. The work-up could stop at any time if a diagnosis was found (13). Lung and heart disease comprised 62% of dyspneic disease causes. Cause was diagnosed in 122/123 (99%) and this study was the first to prominently list obesity as a cause of SOB in an organized work-up in 16% of subjects, consistent with the world-wide obesity epidemic (13). This finding was also consistent with the finding of dyspnea associated with obesity but not airflow obstruction found previously (15).
It should be noted that all three systematic studies that formally looked for the etiology of dyspnea (4,11,13) emphasized obtaining objective studies to determine disease entities since history and physical exam were often incorrect. These studies also emphasized the value of MCT in diagnosing unexpected disease and said MCT was underutilized even in their studies (4,11,13). These latter three studies (4,11,13) reveal that with a very aggressive work-up and follow-up which undoubtedly was expensive, most of the causes of dyspnea are either found or no serious cause of dyspnea is found (4). These latter three studies (4,11,13) also reveal that heart and lung disease still dominate as the cause of dyspnea. These studies are atypical of routine clinical practice.
The current study is similar to what is most likely seen in routine practice world-wide (22). A patient has dyspnea that is either explained or unclear and the patient is referred to pulmonary or cardiology clinic or often both. A work-up is then started in both clinics and some type of explanation for dyspnea is found and treatment is commenced if a definitive etiology is found. Many times no definitive cause is found in either clinic and the patient is then discharged from the specialty clinics. It is unlikely CPET is done routinely in most clinic systems. Those with de-conditioning, obesity, and hyperventilation syndromes are undoubtedly discharged from the specialty clinics with no clear-cut diagnosis. If one finds heart and/or lung disease causing dyspnea, then one has made major strides in decreasing or at least delaying mortality with treatment, since these diseases are well known to increase cause-specific (9), cardiovascular (3,6,7) and all-cause mortality (3,8,9,10).
Huang et al., should be congratulated on reminding us where the state of the diagnosis of chronic dyspnea currently lies i.e., with a diagnosis made on between 60% to 70% of referrals (22). In addition, concurrence between the initial diagnosis by the referrer and the specialty clinic should not be of any concern since it is very difficult to diagnose the cause of dyspnea even for the specialist. Referral with uncertainty should be expected and most likely an organized, methodical approach that leaves no stone unturned is the only way to find the answer (4,11,13). Objective testing is most important including MCT if everything else appears normal. Routine CPET testing is probably not something most clinic systems can refer for at this point, albeit normal testing rules out most diseases.
Screening for chronic dyspnea is important even though it can be argued that tertiary prevention, not secondary prevention (the traditional screening approach in asymptomatic subjects) is occurring (23). Although dyspnea screening is in the symptomatic, the heart and lung diseases that this screening may detect is extremely important since treatment (although tertiary in nature) will decrease morbidity and mortality over time.
Finally, two simple objective tests to direct the dyspnea work-up might be considered. First, a BNP (B-type natriuretic peptide) that is less than 100 (or even better less than 50) should direct initial screening toward a respiratory disease clinic since the yield may be higher there. Second, a room air pulse oximeter saturation less than 90% should alert one to a more aggressive early work-up since some type of disease will be present, whether it be cardiac or lung disease (1).
Acknowledgements
We dedicate this manuscript to Drs. Gerald Thomson and the memory of Gene H. Stollerman for previous generous support. They were former Chairmen of Medicine at Harlem Hospital/Columbia University, New York and the University of Tennessee affiliated hospitals, Memphis, Tenn., respectively.
Funding: This work was supported by the National Institutes of Health (grant number P42ES010349).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Pesola GR, Parvez F, Jasmin S, et al. Dyspnea reproducibility in a rural Bangladesh population. Clin Respir J 2009;3:222-8. [Crossref] [PubMed]
- Parshall MB, Schwartzstein RM, Adams L, et al. Update on the mechanisms, assessment, and management of dyspnea. Am J Respir Crit Care Med 2012;185:435-52. [Crossref] [PubMed]
- Pesola GR, Ahsan H. Dyspnea as an independent predictor of mortality. Clin Respir J 2016;10:142-52. [Crossref] [PubMed]
- DePaso WJ, Winterbauer RH, Lusk JA, et al. Chronic dyspnea unexplained by history, physical examination, chest roentgenogram, and spirometry. Analysis of a seven-year experience. Chest 1991;100:1293-9. [Crossref] [PubMed]
- Lebowitz MD, Burrows B. Comparison of questionnaires: the BMRC and NHLI respiratory questionnaires and a new self-completion questionnaire. Am Rev Respir Dis 1976;113:627-35. [PubMed]
- Ebi-Kryston KL. Respiratory symptoms and pulmonary function as predictors of 10-year mortality from respiratory disease, cardiovascular disease, and all causes in the Whitehall study. J Clin Epidemiol 1988;41:251-60. [Crossref] [PubMed]
- Ebi-Kryston KL, Hawthorne VM, Rose G, et al. Breathlessness, chronic bronchitis and reduced pulmonary function as predictors of cardiovascular disease mortality among men in England, Scotland, and the United States. Int J Epidemiol 1989;18:84-8. [Crossref] [PubMed]
- Waller K, Kaprio J, Kujala UM. Dyspnea and all-cause mortality. 28-yr follow-up study among adult twins. Med Sci Sports Exerc 2014;46:1538-45. [Crossref] [PubMed]
- Pesola GR, Argos M, Chinchilli VM, et al. Dyspnoea as a predictor of cause-specific heart/lung disease mortality in Bangladesh: a prospective cohort study. J Epidemiol Community Health 2016;70:689-95. [Crossref] [PubMed]
- Staats BA. Dyspnea – heart or lungs? Int J Cardiol 1988;19:13-7. [Crossref] [PubMed]
- Pratter MR, Curly FJ, Dubois J., et al. Cause and evaluation of chronic dyspnea in a pulmonary disease clinic. Arch Intern Med 1989;149:2277-82. [Crossref] [PubMed]
- Martinez FJ, Stanopoulos I, Acero R, et al. Graded comprehensive cardiopulmonary exercise testing in the evaluation of dyspnea unexplained by routine evaluation. Chest 1994;105:168-74. [Crossref] [PubMed]
- Pratter MR, Abouzgheib W, Akers S, et al. An algorithmic approach to chronic dyspnea. Respir Med 2011;105:1014-21. [Crossref] [PubMed]
- Karnani NG, Reisfield GM, Wilson GR. Evaluation of chronic dyspnea. Am Fam Physician 2005;71:1529-37. [PubMed]
- Sin DD, Jones RL, Man SF. Obesity is a risk factor for dyspnea but not for airflow obstruction. Arch Intern Med 2002;162:1477-81. [Crossref] [PubMed]
- Currow DC, Clark K, Mitchell GK, et al. Prospectively collected characteristics of adult patients, their consultations and outcomes as they report breathlessness when presenting to general practice in Australia. PLoS One 2013;8:e74814. [Crossref] [PubMed]
- Ho SF, O’Mahoney MS, Seward JA, et al. Dyspnoea and quality of life in older people at home. Age Ageing 2001;30:155-9. [Crossref] [PubMed]
- Niska R, Bhuiya F, Xu J. National hospital ambulatory medical care survey: 2007 emergency department summary. Natl Health Stat Report 2010;26:1-31. [PubMed]
- Woodwell DA. Office visits to internists, 1989. Adv Data 1992;209:1-11. [PubMed]
- Safwenberg U., Terent A, Lind L. Differences in long-term mortality for different emergency department presenting complaints. Acad Emerg Med 2008;15:9-16. [Crossref] [PubMed]
- Nishimura K, Izumi T, Tsukino M, et al. Dyspnea is a better predictor of 5-year survival than airway obstruction in patients with COPD. Chest 2002;121:1434-40. [Crossref] [PubMed]
- Huang YC, Ferry OR, McKenzie SC, et al. Diagnosis of the cause of chronic dyspnoea in primary and tertiary care: characterizing diagnostic confidence. J Thorac Dis 2018;10:3745-56. [Crossref] [PubMed]
- Pesola GR, Forde AT, Ahsan H. Screening for shortness of breath: stretching the screening paradigm to tertiary prevention. Am J Public Health 2017;107:386-8. [Crossref] [PubMed]


