
Uniportal video-assisted thoracoscopic surgery for the treatment of thoracic emergencies
Introduction
Video-assisted thoracoscopic surgery (VATS) experienced a remarkable development in the last two decades (1). In recent years, VATS has been undergoing several modifications and implementations, in particular concerning the number and location of ports, to minimize the invasiveness of the procedure. Recently published data has shown that the minimally invasive uniportal VATS is comparable to multiport VATS regarding general complications, but seems to reduce hospital stay (2), and have a positive impact on the postoperative pain (3), even though further studies are required for definitive conclusions. Rocco and Gonzalez-Rivas were among the first clinicians who implemented this new technique (4,5). Supporters of the uniportal approach emphasize the benefit of a reduced recovery time due to the less invasive character of the procedure, whereas critics argue the possibly decremented oncological outcome. Nowadays the technique is implemented in the clinical practice worldwide (6). After performing uniportal VATS for wedge resections, lobectomies and pneumonectomies, the scope of application was extended to thoracic emergency cases (7). The first report of VATS in trauma patients was described in 1976 where thoracoscopy was used as a diagnostic means (8). Later, in 1981, Jones et al. published a series of 36 trauma patients with hemothoraces who underwent emergency thoracoscopy in local anesthesia. Thoracotomy was avoided in 44% (9). VATS compared to thoracotomy in trauma patients resulted in less postoperative pain and analgesic use, a better cosmetic outcome and a more frequent complete recovery and return to normal lifestyle after surgery (10). However, reports about emergency thoracoscopic procedures are scarce in scientific literature.
In the case of hemothorax, some authors suggest the use of early VATS for the exploration and treatment of the injury (11). Indeed, different cut-offs of chest tube output are mentioned. Mahoozi et al. recommend VATS for the treatment of hemothoraces with initial chest tube outputs of more than 300 milliliters (12).
According to other authors, the mortality could be higher in patients with a total chest tube output of 1,500 mL within 24 h compared to that of patients with a chest tube output <500 mL. Therefore, an explorative thoracotomy is recommended when an initial output of blood between 500 and 1,500 or >250–500 mL within the first 1–3 h is observed (13).
Other indications for an immediate emergency anterolateral thoracotomy or sternotomy are penetrating injuries, hemodynamic shock, signs of pericardial tamponade, severe bleeding, missing peripheral pulses and acute cardiac arrest (14).
The aim of this study was to evaluate the feasibility and safety of uniportal VATS for the management of emergency cases.
Methods
The uniportal VATS technique was introduced at our clinic in 2012. Since then, 642 uniportal VATS procedures have been performed. After becoming familiar with the technique and the successful application on minor procedures, the spectrum of indications was gradually extended. All uniportal VATS performed for emergency cases, between June 2012 and September 2017 were retrospectively reviewed.
The inclusion criteria were: uniportal VATS approach for the management of active bleeding after penetrating injuries or a chest-drain output of more than 250–500 mL of blood within the first 1–3 h. All patients were hemodynamically stable. Two patients presented with a hemorrhagic shock, caused by an intrathoracic bleeding after thoracentesis, they were stabilized prior to the operation. A preoperative CT scan was performed in 10 cases. Two cases had a preoperative X-ray. Three patients got a chest tube preoperatively. One in the emergency room (1,800 mL/12 h) and two at the intensive care unit (ICU) (1.5 and 1 L spontaneously).
All patients were intubated with a double-lumen tube, positioned in left lateral or right lateral position and ventilated using a single-lung ventilation during the procedure according to the side of injury. The approach was a single incision (3–4 cm) in the 5th intercostal space or through the chest tube incision. A wound protector was always in place. A 30° scope was applied and purpose- designed instruments with proximal and distal articulations were used. Intraoperatively, the source of bleeding was identified and treated. If necessary, lung injuries were sutured or a wedge resection was performed. At the end of the operation a chest tube (24 Ch.) was placed. Twelve patients were included in this pilot study.
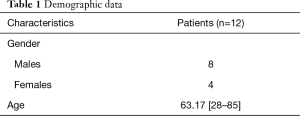
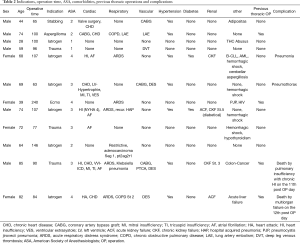
The demographic details are shown in Table 1. Preliminary results were evaluated and the outcomes in terms of mortality, conversion rate, operation time and duration of hospital and ICU stay were analyzed. In two cases (iatrogenic hemothoraces) we adjusted the duration of “postoperative ICU and hospital stay” for the number of hospital days caused by the postoperative treatment itself. The total duration of hospitalization was prolonged due to multiple comorbidities. These two cases were long-term hospitalized preoperatively and presented with an iatrogenic hemothorax after thoracentesis. After the uniportal VATS was performed, they were admitted in thoracic surgery department until the end of postoperative treatments was finished. Since these two patients still needed to be hospitalized due to other comorbidities, the postoperative ICU and hospital stay were adjusted to the number of days until the thoracic surgical treatment was completed. The prolonged hospitalization was not caused by the surgical treatment.
Full table
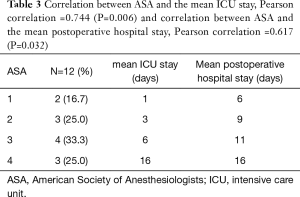
The parameter “ASA-Physical Status” [American Society of Anesthesiologists (ASA)] was approximately normally distributed, as assessed by the Kolmogorow-Smirnow-test, P>0.05 and by the Shapiro-Wilk-test, P>0.05. Afterwards, we have analyzed possible correlations between the ASA and the post-operative hospital stay, as well as between the ASA and the mean postoperative ICU stay, as well as between the ASA and the days until the chest tube was removed, as well as between the ASA and the operation time, using the Pearson correlation. A P value <0.05 was considered significant.
Results
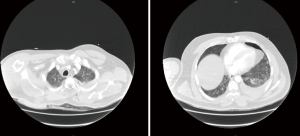
Eight (66.7%) patients were male and four (33.3%) female (Table 1). The mean age was 63.17 [28–85] years (Table 1). The indications were active bleeding hemothoraces of iatrogenic origin (n=6), by a stabbing injury (n=1) (Figure 1, Table 2), by dull trauma (n=3), by an aspergilloma (n=1) and under extracorporeal membrane oxygenation (ECMO) therapy (n=1).
Full table
The mean operative time was 106.25 minutes [63–240] and the chest tube was removed between the first and 25th post-operative day (average =6.75 days). In two thirds of the cases the chest tube was removed during the first 5 days. The postoperative hospital stays ranged from 4 to 26 days. The mean postoperative hospital stay was 10.67 days.
All patients were transferred to the ICU after surgery, 3 (25%) of them stayed for surveillance for only one night. Fifty-eight percent (n=7) of patients stayed at ICU for 4 days or less. The average stay was 6.75 days. A significant correlation was shown between the ASA and the post-operative hospital stay (r=0.617, P=0.032), as well as between the ASA and the mean postoperative ICU stay (r=0.812, P=0.006) (Table 3). All other calculated correlations were not significant. There were no conversions. All cases were managed exclusively by uniportal VATS and there was no need of revision surgery. The intraoperative mortality was nil.
Full table
One patient acquired a post-operative pneumonia and one patient developed a pneumothorax. Two patients died on the 11th and 12th postoperative day of multi-organ-failure caused by their multiple comorbidities (Table 2). The four patients with a complication were ASA 3 or 4 and had multiple comorbidities, but there was no direct correlation between the two factors.
Conclusions
As stated in the German polytrauma guidelines, the standard approach for an emergency thoracotomy is anterolateral but VATS can be used for diagnostic and therapeutic indications in hemodynamically stable patients (14). VATS via single-incision has seen a huge growth over the last years. This development was initiated by Rocco and Gonzalez-Rivas (1,5). One of the main strengths of the uniportal technique is the better intraoperative view as shown by Bertolaccini et al. (15). With only one intercostal space involved and no trocars used or rib spreading, the irritation and injury of intercostal nerves is reduced or even completely avoided (16). Furthermore, the technique presents important advantages also for the surgeons, ensuring a direct view of the target and a more comfortable instrumentation and for the patient the reduction in postoperative pain and a better cosmetic outcome. Therefore, several centers have chosen uniportal VATS as their routine approach.
Due to the high mortality of thoracic trauma, fast and safe diagnostics are important. Uniportal VATS is suitable for diagnosis, inspection and exploration (17). In case of an emergency, the uniportal incision can be enlarged into a lateral thoracotomy very quickly and with less chest wall trauma compared to other, multiportal, incisions.
VATS has a favorable postoperative course, a greater patient satisfaction and a superior long-term outcome compared to open surgery in hemodynamically stable patients with blunt and penetrating chest trauma (10). Due to the small single incision uniportal VATS is also superior to other thoracic methods in the cosmetic result (18) and in postoperative mobilization (19). All these aspects are, particularly beneficial for elderly and multimorbid patients undergoing an emergency thoracic surgery.
Divisi et al. had already shown in 2004 the effectiveness for multiportal VATS approaches in a diagnostic and therapeutic role for cardiopulmonary stable patients with a chest trauma (20).
Potentially, uniportal VATS is suitable for all kinds of thoracic surgery emergency indications, such as bleeding control, stab injury, removal of foreign bodies, pneumothorax (4,17).
Reasons not to perform uniportal VATS include hemodynamically instable patients, insufficient training or less experienced surgeons.
Our paper presented the preliminary results about our series of uniportal thoracic emergency cases. The main limitations of the study are: the retrospective analysis, the small sample of patients and the lack of a control group.
However according to our preliminary results, uniportal VATS seems to be a safe and feasible approach for managing thoracic emergency, in experienced hands, but further research with a larger population size is needed to confirm these findings.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the Institutional Review Board of Charité – Universitätsmedizin Berlin.
References
- Rocco G. Fact checking in the history of uniportal video-assisted thoracoscopic surgery. J Thorac Dis 2016;8:1849-50. [Crossref] [PubMed]
- Akter F, Routledge T, Toufektzian L, et al. In minor and major thoracic procedures is uniport superior to multiport video-assisted thoracoscopic surgery? Interact Cardiovasc Thorac Surg 2015;20:550-5. [Crossref] [PubMed]
- Young R, McElnay P, Leslie R, et al. Is uniport thoracoscopic surgery less painful than multiple port approaches? Interact Cardiovasc Thorac Surg 2015;20:409-14. [Crossref] [PubMed]
- Rocco G, Martucci N, La Manna C, et al. Ten-year experience on 644 patients undergoing single-port (uniportal) video-assisted thoracoscopic surgery. Ann Thorac Surg 2013;96:434-8. [Crossref] [PubMed]
- Gonzalez D, de la Torre M, Paradela M, et al. Video-assisted thoracic surgery lobectomy: 3-year initial experience with 200 cases. Eur J Cardiothorac Surg 2011;40:e21-8. [Crossref] [PubMed]
- Guerra M, Fernandes P, Martins D, et al. Uniportal thoracoscopic lobectomy. Rev Port Cir Cardiotorac Vasc 2014;21:99-105. [PubMed]
- Ismail M, Helmig M, Swierzy M, et al. Uniportal VATS: the first German experience. J Thorac Dis 2014;6:S650-5. [PubMed]
- Jackson AM, Ferreira AA. Thoracoscopy as an aid to the diagnosis of diaphragmatic injury in penetrating wounds of the left lower chest: a preliminary report. Injury 1976;7:213-7. [Crossref] [PubMed]
- Jones JW, Kitahama A, Webb WR, et al. Emergency thoracoscopy: a logical approach to chest trauma management. J Trauma 1981;21:280-4. [Crossref] [PubMed]
- Ben-Nun A, Orlovsky M, Best LA. Video-assisted thoracoscopic surgery in the treatment of chest trauma: long-term benefit. Ann Thorac Surg 2007;83:383-7. [Crossref] [PubMed]
- Vassiliu P, Velmahos GC, Toutouzas KG. Timing, safety, and efficacy of thoracoscopic evacuation of undrained post-traumatic hemothorax. Am Surg 2001;67:1165-9. [PubMed]
- Mahoozi HR, Volmerig J, Hecker E, et al. Modern Management of Traumatic Hemothorax. J Trauma Treat 2016;5:326. [Crossref]
- Karmy-Jones R, Jurkovich GJ, Nathens AB, et al. Timing of urgent thoracotomy for hemorrhage after trauma: a multicenter study. Arch Surg 2001;136:513-8. [Crossref] [PubMed]
- AMWF. S3 – Leitlinie Polytrauma / Schwerverletzten-Behandlung. Deutsche Gesellschaft für Unfallchirurgie. 2017. Available online: http://www.awmf.org/uploads/tx_szleitlinien/012-019l_S3_Polytrauma_Schwerverletzten-Behandlung_2017-03.pdf
- Bertolaccini L, Viti A, Terzi A, et al. Geometric and ergonomic characteristics of the uniportal video-assisted thoracoscopic surgery (VATS) approach. Ann Cardiothorac Surg 2016;5:118-22. [Crossref] [PubMed]
- Tamura M, Shimizu Y, Hashizume Y. Pain following thoracoscopic surgery: retrospective analysis between single-incision and three-port video-assisted thoracoscopic surgery. J Cardiothorac Surg 2013;8:153. [Crossref] [PubMed]
- Rocco G, Khalil M, Jutley R. Uniportal video-assisted thoracoscopic surgery wedge lung biopsy in the diagnosis of interstitial lung diseases. J Thorac Cardiovasc Surg 2005;129:947-8. [Crossref] [PubMed]
- Yang HC, Cho S, Jheon S. Single-incision thoracoscopic surgery for primary spontaneous pneumothorax using the SILS port compared with conventional three-port surgery. Surg Endosc 2013;27:139-45. [Crossref] [PubMed]
- Salati M, Brunelli A, Rocco G. Uniportal video-assisted thoracic surgery for diagnosis and treatment of intrathoracic conditions. Thorac Surg Clin 2008;18:305-10. vii. [Crossref] [PubMed]
- Divisi D, Battaglia C, De Berardis B, et al. Video-assisted thoracoscopy in thoracic injury: early or delayed indication? Acta Biomed 2004;75:158-63. [PubMed]


