Management of traumatic esophageal injuries
Introduction
Traumatic esophageal perforations are rare injuries but one associated with significant morbidity. Primary mechanisms of esophageal injury are penetrating trauma with gunshot wounds accounting for 70–80% of cases, followed by stab injuries in 15–20%. Less than 1% of cases are caused by blunt esophageal trauma. Overall mortality in patients is estimated at 20–30% mostly because of presence of other high grade injuries (1,2). Furthermore, delayed diagnosis of injury contributes to increased morbidity and mortality.
General symptoms of esophageal trauma are non-specific and can include hematemesis, hemoptysis, hoarseness, odynophagia and dysphagia. Physical exam features include subcutaneous emphysema, neck hematoma, and neck tenderness. Thoracic esophageal injuries may be associated with mediastinal crunch on auscultation known as Hamman’s sign (3). Overt violation of the platysma is an indication for neck exploration in addition to other hard signs [subcutaneous emphysema/air bubbling through wound, expanding or pulsatile hematoma, active bleeding, neurologic deficit, hematemesis (4)].
Work-up
A chest and abdominal X-ray are usually standard baseline images obtained in the trauma bay. X-rays may demonstrate air within the soft tissues of the neck, pneumomediastinum or free air within the abdomen. Although these could possibly indicate esophageal injury, such findings are non-specific and warrant complete investigation for other associated injuries.
Unstable patients need surgical exploration. Further investigations of esophageal injury in stable patients can begin with water soluble contrast esophagrams. Complementing the esophagogram with esophagoscopy provides a nearly 100% specificity to rule out injury. The role of CT scans in identification of esophageal injury is limited. Scan findings such as pneumomediastinum require further workup with esophagogram/esophagoscopy (5). Surgical exploration of the neck does not exclude esophageal injury reliably especially in the setting of extensive associated injuries and inflammation. In these circumstances, further work-up is also indicated to avoid the morbidity of missed injuries. Therefore when the circumstances allow for it, a combined esophagogram/esophagoscopy approach is best accomplished before exploration in patients who have a possibility of esophageal perforation on other clinical grounds.
Management
Initial management
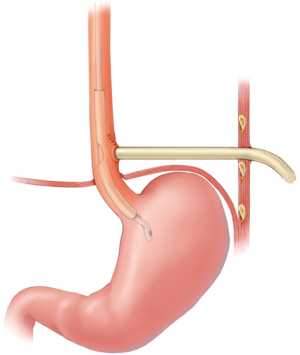
Initial management principles for an identified esophageal injury include nil-per-os status, internal drainage by careful insertion of a nasogastric tube (under endoscopic guidance), broad spectrum antibiotics and fluid resuscitation. Otherwise, initial surgical management is directed towards life and limb threatening conditions.
General principles of esophageal perforation management regardless of location include: (I) excellent exposure; (II) debridement of non-viable tissue; (III) closure of defect; (IV) use of buttress (muscle preferred); and (V) adequate tube drainage.
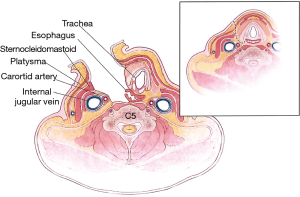
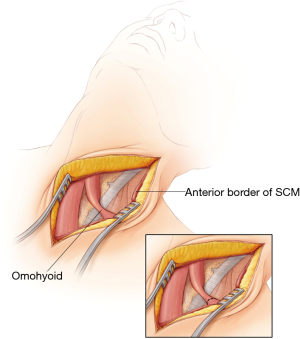
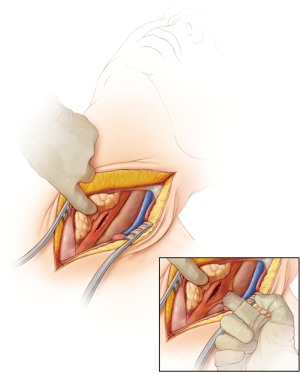
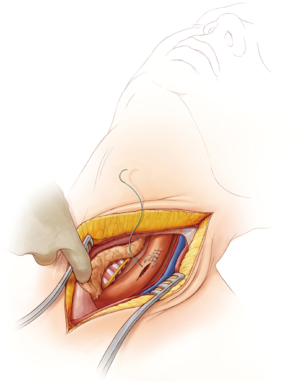
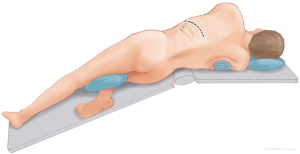
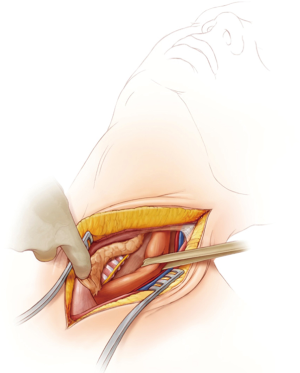
Cervical esophageal
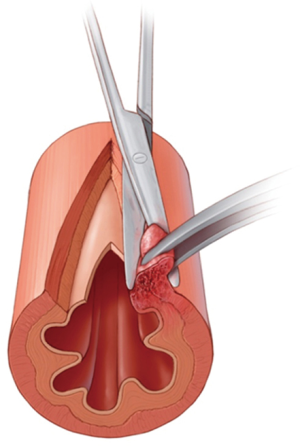
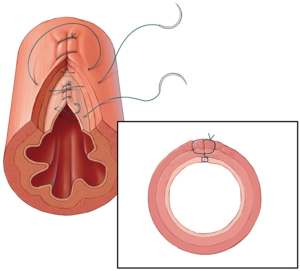
Approaches to the cervical esophagus include a collar incision or incision just anterior to the sternocleidomastoid muscle (Figure 1). Division of the omohyoid is usually required to access the esophagus however a more lateral division allows usage of this muscle as a potential pedicled muscle buttress (Figure 2). The esophagus is located posterior to the trachea with the recurrent laryngeal nerve running in the trachea-esophageal groove. Exposure of the esophagus posteriorly is obtained by blunt dissection between the trachea and the esophagus along the longitudinal plane kept directly on the esophagus to decrease potential for injury to the recurrent laryngeal nerve (Figure 3). Insertion of a nasogastric tube can aid in identification of the esophagus in a difficult field. Once dissection is completed circumferentially, a penrose drain is used to encircle the esophagus (Figure 4). This permits close examination of the cervical esophagus and facilitates manipulation. Upon identification of the injury, the non-viable edges are debrided and the defect is closed in a single or double layer with absorbable sutures (Figure 5). Muscle flaps that include the sternocleidomastoid, strap, or omohyoid are used to buttress the coverage of the closure. Drainage of the neck is completed with insertion of a Jackson Pratt drain exiting though a separate lateral stab incision. In cases of severe inflammation or delayed injury recognition the site of perforation may not be identifiable. In such cases wide drainage and buttress with a muscle flap is the preferred management.
Thoracic esophagus
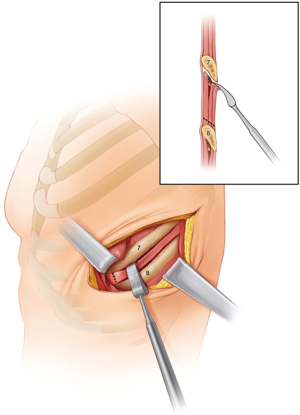
The approach to the thoracic esophagus is dependent on the location of the injury. Distal esophageal injuries are best accessed through a left thoracotomy through the 7th or 8th intercostal space (Figure 6). Mid esophageal injuries are best approached through a right thoracotomy at the level of the 5th intercostal space. Treatment of associated injuries will also modify the access incision. Thoracic esophageal perforations are associated with inflammation hence decortication of the thoracic cavity and mediastinal irrigation is indicated. The presence of a nasogastric tube or a carefully inserted bougie can aid in identification of the esophagus in cases of severe inflammation. The myotomy at the level of the perforation is extended to expose the full extent of the mucosal defect with debridement of non-viable tissue (Figures 7,8). The defect is then closed in two layers (mucosa and submucosa, then muscle) using absorbable sutures over a bougie (Figure 9). Insertion of a muscle flap buttress is an important adjunct to overlap on the perforation or between the trachea and esophagus in cases of concomitant injury. Intercostal muscle flaps can be rapidly harvested and generally reach the esophagus in most locations (Figure 10). In order to maximize the availability of an intercostal flap it should be harvested at the time of the initial thoracotomy. Serratus anterior flaps provide greater bulk however their reach in very low perforations may be limited. The latissimus dorsi flap is an option however its use in the unstable patient is limited given the greater time it takes to harvest. Other buttressing options described include the rhomboid muscle, pedicled diaphragm flaps and pedicled thymic flaps. Early wide drainage of the mediastinum is indicated and placement of a feeding jejunostomy is recommended to secure enteral access for post-operative nutrition. Insertion of a gastrostomy tube permits decompression of the esophagus and frees the patient from prolonged use of a nasogastric tube.

Abdominal esophageal injuries
Isolated abdominal esophageal injuries are rare and are generally found as an extension of thoracic esophageal injuries or with significant intra-abdominal trauma. Access is obtained through a laparotomy however a left thoracotomy or thoracoabdominal incisions need to be considered depending on extension of the injury. Similar principles as described earlier apply to the abdominal esophagus including debridement, primary closure and buttress of repair. A thal patch, partial fundoplication, omental and diaphragmatic patches are all useful materials for an effective buttress. A draining gastrostomy and feeding jejunostomy are inserted in addition to local drainage.
Delayed and extensive injuries
In certain cases, primary closure of the esophagus may not be feasible. These circumstances are exceedingly rare. One strategy for the irreparably damaged esophagus is an emergency esophagectomy and diversion. However, it should be noted that even in high volume trauma centers this type of management is rarely necessary (6,7). Another strategy is creation of a controlled fistula using a T tube (Figure 11). Large unrepairable injuries can be covered with a muscle onlay after insertion of a T tube in the perforation which exits through the chest wall. A nasogastric tube is inserted through the T tube for decompression.
Stent placement for esophageal perforation due to trauma remains a limited experience. The use of endoluminal stenting for spontaneous (Boerhaave) perforation or for leaks after esophageal procedures is increasing. In general the favorable factors for success in these etiologies include an intrathoracic location of the perforation and smaller perforation sizes (<6 cm). Since traumatic esophageal perforations generally have other indications for a thoracotomy (for management of associated injuries) esophageal stenting currently is not a routine strategy for the trauma patient (8).
Increased postoperative morbidity is associated with delayed diagnosis and also dependent on the severity of associated injuries. Leaks from repaired perforations result in mediastinitis and respiratory morbidity. Most can be managed non-operatively with antibiotics, chest drainage, withholding oral intake and distal enteral nutrition.
Conclusions
Traumatic esophageal injuries are rare but highly morbid. Management is dictated by location of the perforation and any concurrent injuries. The majority of cases are amenable to primary repair with flap re-enforcement. Other principles include adequate drainage around the repair, decompression of the esophagus and stomach (via nasogastric tube or gastrostomy tube) and distal enteral nutrition (feeding jejunostomy).
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Asensio JA, Chahwan S, Forno W, et al. Penetrating esophageal injuries: multicenter study of the American Association for the Surgery of Trauma. J Trauma 2001;50:289-96. [Crossref] [PubMed]
- Patel MS, Malinoski DJ, Zhou L, et al. Penetrating oesophageal injury: a contemporary analysis of the National Trauma Data Bank. Injury 2013;44:48-55. [Crossref] [PubMed]
- Biffl WL, Moore EE, Feliciano DV, et al. Western Trauma Association Critical Decisions in Trauma: Diagnosis and management of esophageal injuries. J Trauma Acute Care Surg 2015;79:1089-95. [Crossref] [PubMed]
- Sperry JL, Moore EE, Coimbra R, et al. Western Trauma Association critical decisions in trauma: penetrating neck trauma. J Trauma Acute Care Surg 2013;75:936-40. [Crossref] [PubMed]
- Makhani M, Midani D, Goldberg A, et al. Pathogenesis and outcomes of traumatic injuries of the esophagus. Dis Esophagus 2014;27:630-6. [Crossref] [PubMed]
- Sudarshan M, Elharram M, Spicer J, et al. Management of esophageal perforation in the endoscopic era: Is operative repair still relevant? Surgery 2016;160:1104-10. [Crossref] [PubMed]
- Biancari F, D'Andrea V, Paone R, et al. Current treatment and outcome of esophageal perforations in adults: systematic review and meta-analysis of 75 studies. World J Surg 2013;37:1051-9. [Crossref] [PubMed]
- Herrera A, Freeman RK. The evolution and current utility of esophageal stent placement for the treatment of acute esophageal perforation. Thorac Surg Clin 2016;26:305-14. [Crossref] [PubMed]