Conservative management of post-intubation tracheal tears—report of three cases
Introduction
These patients, as presented below, underwent routine otolaryngological surgery in a tertiary referral center. We tried to elucidate these cases in critical incident audits. A multidisciplinary team, consisting of otolaryngologists (the operating surgeons involved), anesthetists and an external thoracic surgeon consultant, discussed the course of events. We carried out literature research in PubMed, Web of Science and Cochrane databases with the search strings “subcutaneous emphysema, otolaryngology”, “subcutaneous emphysema, laryngoscopy”, “iatrogenic tracheal rupture”, or “tracheal rupture, intubation”.
Case reports
Clinical history of our three cases is listed in Table 1. Two operations were carried out by an attending surgeon and one was performed by a resident registrar under the supervision of an attending surgeon. Operating teams and anesthetists were different in each case. All operations were done in the same operating theater. Instruments for general anesthesia were checked regularly and after all events. During this period, we used the products from the same endotracheal tube manufacturer and supplier. Difficult but atraumatic intubation was noted in case 3. Operations under anesthetic were uneventful except for case 1.
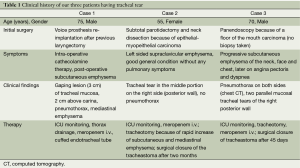
Full table
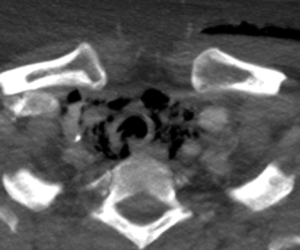
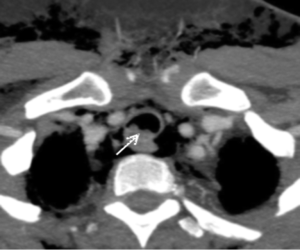
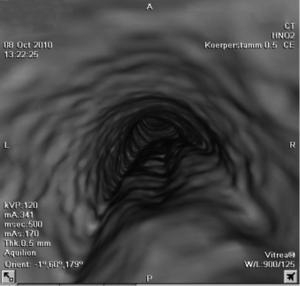
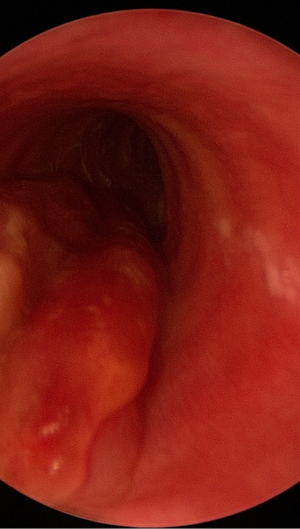
In case 1, the tracheal lesion was diagnosed intra-operatively and the patient was transferred to the ICU immediately after surgery (Figure 1). In this previously laryngectomized patient, we positioned a tracheal tube with cuff distally to the tear to prevent further air leakage through the injury site (1-3). A prerequisite for this method was an intact portion of trachea above the carina (3). Bridging the rupture with the tube and drainage of concomitant pneumothorax allowed a rapid stabilization of vital signs. As this individual was considered a high-risk patient for open-chest surgery (repair of the tear), conservative treatment was initialized. This multimorbid patient had a favorable outcome without closure of the tracheal rupture. A video clip about shows the healed trachea three weeks after injury (Figure 2). In the other two cases, tracheal laceration was diagnosed post-operatively. Subcutaneous emphysema was the first symptom of mucosal injury in these two cases, always appearing post-operatively with a delay of 3-15 h. Once the diagnosis of tracheal injury was made, all patients were continuously monitored for vital signs. Empiric broad-spectrum antibiotic therapy was administered to all patients to prevent mediastinitis. Since these patients presented progressive subcutaneous and mediastinal emphysema or dyspnea or both, we performed tracheostomy to maintain safe airways and to decrease intra-tracheal pressure and air leakage. In these two cases, the need for a secure airway emerged, when the symptoms progressed post-operatively at various intervals. In case 2 for example, this delayed progress appeared one week after the injury. Our experience supports literature data reporting a rapid settling of subcutaneous emphysema and pneumomediastinum after tracheotomy (3-5).
Surgical and anesthesiological procedures were evaluated by an external consultant specialist, who found no abnormalities. The accumulation of events was considered as accidental. After analyzing the possible promoting factors in our case series, we believe that repeated ex- and intubations led to tracheal injury in case 1. In case 2, chronic tracheo-bronchitis and inhalative corticoid treatment might have contributed to increased vulnerability of the tracheal mucosa. In case 3, we did not find any risk factor for the injury.


Discussion
Diagnostic process in post-operative subcutaneous emphysema
If patients develop subcutaneous emphysema after surgery, mucosal injury must be identified, and potential concomitant pneumomediastinum or pneumothorax should be excluded or diagnosed. Emphysema is not specific to tracheal laceration. Diffuse air entrapment in soft tissues of the neck, head and chest may impede the localization of the lesion, and the extent of emphysema does not necessarily reflect the severity of injury (6).
In the literature, combination of chest computed tomography (CT) scans and tracheoscopy are recommended to diagnose a suspected tracheal injury. CT gives evidence of air leakage into the mediastinum and detects a pneumothorax, however, the tracheal injury site seen on CT scans does not always correspond with tracheoscopy findings. CT scans have only 85% sensitivity for detecting tracheal injury (7). Therefore, endoscopic evaluation of the upper aero-digestive tract is the mainstay of diagnosis of tracheal lacerations.
Causes of post-intubation tracheal laceration
Surgical trauma of the mucosa is the main cause of emphysema. However, elevated intrathoracic pressure (physical strain, forced blowing, ventilation with positive pressure, coughing when the expiration vent is closed), lung diseases such as bronchial asthma, or perforation of a lung bulla may provoke subcutaneous emphysema. Iatrogenic tracheal rupture after intubation is very rare. Incidence ranges between 1:20,000 and 1:75,000 for intubation with a ‘single lumen’ endotracheal tube. ‘Double lumen’ endotracheal tubes have a larger diameter and intubation with these tubes causes tracheal rupture more frequently (0.05-0.19%) (8,9). Typically, these lesions are longitudinal lacerations of the posterior tracheal wall (paries membranaceus) (8,10). Due to the anatomic situation with the esophagus supporting the membranous trachea on the left side, tracheal tears are localized more frequently on the right side. Seldom, tracheal lacerations spread out into the bronchi (10).
A meta-analysis of 182 cases (50 reports) demonstrated that emergency intubation is a risk factor of tracheal tears (1). Tracheal rupture occurs mainly in women, the reason is that airways in females have a narrower diameter and tracheas are shorter and less resistant (8,10-14). The precise cause of post-intubation tracheal tears is unclear. It may occur during passage of the endotracheal tube, when the tube’s tip wounds the mucosa, even without difficult intubation (10,15). The use of a stylet as a guide for the tube may also cause tracheal injury by the same mechanism (15). Overinflation of the endotracheal tube cuff is the most common cause of tracheal tears (15-17). Since “high-volume-low-pressure” cuffs have been introduced, this complication is found less frequently, even though not completely eliminated. Accidental cuff overinflation with higher pressure is an obvious explanation; relative overinflation is possible if the cuff is filled just above the carina where the trachea has its largest diameter and the tube is pulled back to its correct position (12). Generally, tube repositioning without cuff deflation should be avoided to prevent mucosal injury. Intra-operative repositioning of the patient’s head or body can also displace an endotracheal tube and promote tracheal injury (1,18). Diffusion of anesthetic N2O gas into the cuff can also increase pressure by overinflating the cuff (19,20), however, N2O was not given in our cases.
Therapeutic approaches for tracheal tears
If a tracheal lesion is confirmed in a patient, anesthetists and thoracic surgeons should be consulted to set up an individualized therapy regime. Delayed clinical presentation of subcutaneous emphysema prolongs diagnosis and therapeutic intervention. Any delay in diagnosis favors deterioration of the clinical situation, i.e., mediastinitis and pneumothorax. Miñambres et al., however, found that diagnosis time does not have an influence on mortality (1). Presumably, the cause that required intubation is a greater factor in clinical outcome than the tracheal injury itself (1).
Traditionally, tracheal tears have usually been treated surgically (1,9,12,17,21). For example, lesions discovered during an open thoracic surgery procedure are repaired at the same time (1,10,21). Nevertheless, delayed surgical repair of the tear doubles the risk of death in patients whose tracheal rupture is detected after surgery, compared to a patient group with simultaneous repair (1). In particular, in severely ill patients, surgical closure via open chest surgery has a mortality up to 71% (13). Increasing evidence is being presented in case series consisting of small numbers of patients, suggesting conservative management of lacerations as a viable option (1). There is a trend toward non-surgical therapy although consensus has not been reached and clear guidelines are lacking (1,14).
The main factors discussed in the literature determining the treatment of choice are, first, the clinical situation of the patient and, second, the properties of the tracheal lesion (localization, length and depth). Recent studies suggest conservative management of tracheal lacerations when patients have minimal, non-progressive symptoms (subcutaneous emphysema or pneumomediastinum), no air leakage, no respiration difficulty, no esophageal injury, and patients who are breathing spontaneously or whose extubation is expected within 24 h (1,10,17).
Some authors emphasized the significance of the length of the rupture and suggested conservative treatment in selected, clinically stable patients having tracheal ruptures less than 2 cm (1,22). Lesions over 2 cm in length are thought to be better treated surgically (1,17,19); others, however, perform conservative therapy in cases with tears up to 4 cm in length (23). Small tracheal lesions localized in the upper third of the trachea can be managed conservatively in patients without respiratory distress or mediastinitis (19). Lacerations of the upper two-thirds of the trachea, and not involving all tracheal layers, are also suitable for non-surgical therapy (2). Cardillo et al. underlined the significance of the depth of the lesion for determining further treatment (14). They suggest immediate surgical repair for cases with esophageal injury and/or mediastinitis. All other injuries of the tracheal wall, including fully penetrating lacerations are managed conservatively with fibrin glue (14).
Tracheal stenting of post-intubation lacerations is a relatively new therapeutic approach (24-26). Expandable tracheal stents represent an alternative to surgical therapy, especially in patients with an unacceptably high risk of surgery-related mortality (26). Problems of airway stents such as halitosis or granulation tissue formation can be treated with inhalation and intraluminal laser vaporization (26). Newly developed removable tracheal stents can prevent these late complications (25).
Tracheotomy is a simple, less invasive alternative to surgical repair as it reduces intratracheal pressure and air leakage through the tear, thereby allowing spontaneous healing of the rupture (3,4,6). Additional CT-scans and endoscopic findings are presented demonstrating the stages of tear healing (Figures 3-7). Direct intraluminal suture of proximal tracheal lacerations can be performed through the tracheal stoma in a minimally invasive manner (18). Moreover, a tracheal stoma makes tracheoscopic control easier.

Failure management after the reported events
In our department we changed anesthetic management to prevent further tracheal injuries. In patient’s informed consent, the possibility of unforeseeable and very rare airway injuries is now explicit mentioned. Continuous cuff pressure monitoring was introduced and all anesthesia devices were supervised. To be able to examine potential material faults, used endotracheal tubes are retained until the discharge of each patient. Ultimately, the manufacturer of endotracheal tubes was changed. After these measures were taken, we have not diagnosed a new case with tracheal injury.
Conclusions
In our three cases, a conservative management (tracheotomy + empiric broad-spectrum antibiotic therapy) of post-intubation tracheal laceration proved to be a safe and effective procedure. All tracheal ruptures healed without sequelae. No mediastinitis or injury-related deaths occurred. Tracheal stoma was surgically closed in all but one case (laryngectomized patient) with good cosmetic results.
Nevertheless, we believe that the risk for intubation-related tracheal injuries can only be minimized but not completely eliminated, being inherent complications of the procedure.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Miñambres E, Burón J, Ballesteros MA, et al. Tracheal rupture after endotracheal intubation: a literature systematic review. Eur J Cardiothorac Surg 2009;35:1056-62. [PubMed]
- Gabor S, Renner H, Pinter H, et al. Indications for surgery in tracheobronchial ruptures. Eur J Cardiothorac Surg 2001;20:399-404. [PubMed]
- Mullan GP, Georgalas C, Arora A, et al. Conservative management of a major post-intubation tracheal injury and review of current management. Eur Arch Otorhinolaryngol 2007;264:685-8. [PubMed]
- Peña MT, Aujla PK, Choi SS, et al. Acute airway distress from endotracheal intubation injury in the pediatric aerodigestive tract. Otolaryngol Head Neck Surg 2004;130:575-8. [PubMed]
- Óvári A, Just T, Dommerich S, et al. Conservative management of post-intubation tracheal tears—report of three cases. Asvide 2014;1:242.
- Seidl RO, Todt I, Nielitz T, et al. Tracheal ruptures in endotracheal intubation. Diagnosis and therapy. HNO 2002;50:134-8. [PubMed]
- Chen JD, Shanmuganathan K, Mirvis SE, et al. Using CT to diagnose tracheal rupture. AJR Am J Roentgenol 2001;176:1273-80. [PubMed]
- Lampl L. Tracheobronchial injuries. Conservative treatment. Interact Cardiovasc Thorac Surg 2004;3:401-5. [PubMed]
- Schneider T, Volz K, Dienemann H, et al. Incidence and treatment modalities of tracheobronchial injuries in Germany. Interact Cardiovasc Thorac Surg 2009;8:571-6. [PubMed]
- Conti M, Pougeoise M, Wurtz A, et al. Management of postintubation tracheobronchial ruptures. Chest 2006;130:412-8. [PubMed]
- Hofmann HS, Rettig G, Radke J, et al. Iatrogenic ruptures of the tracheobronchial tree. Eur J Cardiothorac Surg 2002;21:649-52. [PubMed]
- Massard G, Rougé C, Dabbagh A, et al. Tracheobronchial lacerations after intubation and tracheostomy. Ann Thorac Surg 1996;61:1483-7. [PubMed]
- Meyer M. Latrogenic tracheobronchial lesions--a report on 13 cases. Thorac Cardiovasc Surg 2001;49:115-9. [PubMed]
- Cardillo G, Carbone L, Carleo F, et al. Tracheal lacerations after endotracheal intubation: a proposed morphological classification to guide non-surgical treatment. Eur J Cardiothorac Surg 2010;37:581-7. [PubMed]
- Jo YY, Park WY, Choi E, et al. Delayed detection of subcutaneous emphysema following routine endotracheal intubation -A case report-. Korean J Anesthesiol 2010;59:220-3. [PubMed]
- Striebel HW, Pinkwart LU, Karavias T. Tracheal rupture caused by overinflation of endotracheal tube cuff. Anaesthesist 1995;44:186-8. [PubMed]
- Marty-Ané CH, Picard E, Jonquet O, et al. Membranous tracheal rupture after endotracheal intubation. Ann Thorac Surg 1995;60:1367-71. [PubMed]
- Walles T, Friedel G, Stöltzing H, et al. Case studies of iatrogenic tracheal injury during intraoperative ventral positioning. Symptoms, diagnostics, and differential therapy. Chirurg 2007;78:374-8. [PubMed]
- Sippel M, Putensen C, Hirner A, et al. Tracheal rupture after endotracheal intubation: experience with management in 13 cases. Thorac Cardiovasc Surg 2006;54:51-6. [PubMed]
- Tu HN, Saidi N, Leiutaud T, et al. Nitrous oxide increases endotracheal cuff pressure and the incidence of tracheal lesions in anesthetized patients. Anesth Analg 1999;89:187-90. [PubMed]
- Borasio P, Ardissone F, Chiampo G. Post-intubation tracheal rupture. A report on ten cases. Eur J Cardiothorac Surg 1997;12:98-100. [PubMed]
- Carbognani P, Bobbio A, Cattelani L, et al. Management of postintubation membranous tracheal rupture. Ann Thorac Surg 2004;77:406-9. [PubMed]
- Jougon J, Ballester M, Choukroun E, et al. Conservative treatment for postintubation tracheobronchial rupture. Ann Thorac Surg 2000;69:216-20. [PubMed]
- Yopp AC, Eckstein JG, Savel RH, et al. Tracheal stenting of iatrogenic tracheal injury: a novel management approach. Ann Thorac Surg 2007;83:1897-9. [PubMed]
- Creagh-Brown B, Sheth A, Crerar-Gilbert A, et al. A novel approach to the management of acute tracheal tear. J Laryngol Otol 2008;122:1392-3. [PubMed]
- Madden BP, Sheth A, Ho TB, et al. Novel approach to management of a posterior tracheal tear complicating percutaneous tracheostomy. Br J Anaesth 2004;92:437-9. [PubMed]


