The carina is approximately 1-2 cm above the pericardial reflection among Chinese patients
Introduction
Central venous catheters (CVCs) and central venous pressure (CVP) monitor is essential in fluid resuscitation and management for critically ill patients. Accuracy of the CVP is mainly dependent on the proper position of the catheter. It is generally recommended that the CVC tip should lie in the superior vena cava (SVC) and outside the pericardial sac, so as to guarantee the catheter performance and spare the patient from life-threatening complications such as arrhythmia and pericardial tamponade.
However, it is very difficult to put the CVCs tips to the recommended position in clinical practice because the recommended pericardial reflection (PR) is not palpable and can not be seen on chest X-ray. Therefore, the carina, easily visualized on the chest X-ray, is alternatively used as the radiographic landmark to guide of the placement of the CVCs (1-4). Nevertheless, few data is available so far as to whether the recommended carina is also a good landmark for PR among Chinese patients. Thus, this study was designed to explore the topographic relationship between the trachea carina and PR among Chinese patients by using computed tomography (CT) images.
Methods
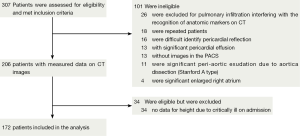
The study was a retrospective review of CT of all patients underwent CT pulmonary angiogram or CT angiogram for aorta from January 1, 2013 to November 30, 2013, to examine the distance between the carina and PR among Chinese patients. The institutional review board of Sir Run Run Shaw hospital approved the study protocol and waived from the need for a consent form. All CT examinations were performed for clinical indications. Patients with unrecognizable anatomic markers, significant pericardial effusion, peri-aortic exudation or significant enlarged right atrium were excluded (Figure 1).
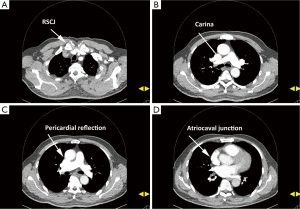
All examinations were performed on routine clinical CT scanners (SENSATION 16, SIEMENS, Germany). In all patients, the imaging was performed at end-inspiration. A tube current of 120 kV and rotation time of 0.5 s was used. Slice thickness varied between 0.75 and 2 mm, depending on the clinical protocol used. Images were evaluated on a standard clinical picture archiving and communication system workstation, and the reader of CT images was blinded to patient data. The preselected radiographic landmarks, most often used in our clinical practice, included the upper margin of the right clavicular notch (RSCJ), carina, PR, and atriocaval junction (ACJ). First of all, the ACJ was determined by the method described by Ridge and colleagues (5), i.e., localizing on the sagittal reformatted CT image as the midpoint of an oblique line drawn from the crista terminalis anteriorly to the crista dividens posteriorly. This point was then cross-referenced with axial CT images and the calibrated anteroposterior scout topogram to determine its horizontal level (5). After recognition of the above landmarks on CT images (Figure 2), likewise, the horizontal level of the RSCJ, carina and PR were also marked on the scout topogram. Thereafter, distances (in centimeters) between RSCJ, trachea carina, PR and ACJ were calculated using the table positions on axial images. The distance between PR and lower level of the junction of left and right innominate veins was referred as the length of extrapericardial SVC.
Statistical analysis
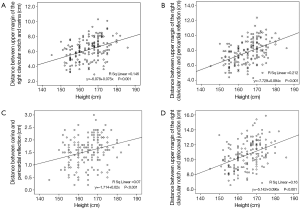
Descriptive data were reported as mean, standard deviation, and range. The relationship between RSCJ-ACJ (distance between upper margin of the right clavicular notch and atriocaval junction), RSCJ-Carina (distance between upper margin of the right clavicular notch and carina), RSCJ-PR (distance between upper margin of the right clavicular notch and pericardial reflection), Carina-PR (distance between carina and pericardial reflection) and patients’ height were examined, using a linear regression model. Statistical analysis was performed, using SPSS 16.0 (Chicago, Ill, USA). Significance was defined as a P value
Results
From January 2013 to November 2013, 172 patients were enrolled in this study (Figure 1). Of them, 122 were men and 50 were women, with a mean age of 53 years old (range, 18-80 years old).
Anatomical presentation in CT
The extrapericardial SVC, target segment of recommended CVCs tips placement, had a mean length of 2.5 cm, ranging from 0.3 to 4.8 cm. The average distances between upper margin of the right clavicular notch and carina and PR were 6.1 cm (range, 2.9-10.1 cm) and 7.7 cm (range, 4.3-11.3 cm) respectively. For all patients, the PR was lower than the carina. On average, the PR was 1.6 cm below the carina (Table 1).
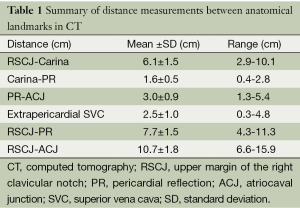
Full table
Correlation between the carina-pericardial reflection distance and height
As expected, the distances between upper margin of the right clavicular notch and carina, PR and ACJ were linear correlated with height (Figure 3). Consequently, distance between carina and PR was equivalent to –1.714+0.02× height (cm) (Figure 3).
Discussion
Our in vivo CT measurements demonstrated that the mean length of extrapericardial SVC was 2.5 cm and carina was averagely 1.6 cm higher than the PR among Chinese patients. Given this, placing the tips of CVCs averagely 1.6 cm lower the carina would be more reasonable among Chinese patients.
The incidence of intraatrial CVC tip position after conventional placement techniques ranges from 8% to 47% (6,7). Whilst incidence of vessel perforation associated with CVC placement ranged from approximately 0.25% to 0.4%. Vascular perforation or cardiac tamponade is rare but is one of the most serious complications in relation to CVCs. Perforation of the SVC is probably more likely with left-sided than with right-sided CVCs (8). This is influenced by the steep angle the left innominate vein makes with the SVC. Here the catheter will abut the wall of the SVC unless the tip is advanced around the curve into the lower SVC or right atrium. It has been shown in the laboratory that an angle of the CVC tip to vessel wall of greater than 40° is more likely to lead to vessel wall perforation (8). To prevent such complications, many suggestions have been made for assessing correct placement of CVCs, most based on clinical investigations and analysis of chest X-rays. Besides parallel to the vessel wall, the carina was firstly proposed by Schuster et al. (1) as a reliable landmark for the tip of CVCs. Nevertheless, optimal position of the CVC tip remains a subject of debate.
In the present study, the PR was always below the carina, with a mean distance of 1.6 cm. This was consistent with previous studies in ethanol-formalin-fixed (1) or fresh cadavers (2), in those the carina was 0.4 and 0.8 cm mean above the PR respectively. The gap of the distances between various studies may be explained by that tissue shrinkage in cadavers. Although in no case in this study and some other studies (1,2) was the carina located below the PR, a recent study of topographic analysis based on CT demonstrated 30% of the patients had a pericardium ending above the carina, with a maximum distance of 2.5 cm (9). The exact reasons for the variance were not elucidated. This may be because Chinese patients are somewhat anatomically different from other races with respect to the relation of carina and PR.
The influence of possible confounders such as age, weight, height, or gender on the distance between carina and PR is also of interest. The study demonstrated the distance between carina and pericardial reflection was equivalent to –1.714+0.02× height (cm). Given vast majority Chinese patients’ height was approximate 160 to 170 cm, using the carina as a surrogate for the PR to guide the tip position of CVCs may underestimate the depth of catheter insertion by around 1.6 cm.
Nevertheless, to place a CVC tip in the optimal position is still challenging. Uchida and colleagues (10) demonstrated the appropriate length of CVC inserted through the right internal jugular vein or right subclavian vein could be estimated by the “calculated measurement” of adding half the length of the right clavicle and the vertical length between the sternal head of the right clavicle and the carina on the previous X-ray. Meanwhile, Dulce and colleagues (9) suggested that a higher percentage of extrapericardial placements of the CVC would be achieved by using 85% of the SCJ-to-carina distance for orientation, with similar correct placement in 86% of case in CT. Taken ours and above studies together, using the calculated measurement of the distance from insertion point and carina on previous chest X-ray and a fixed distance approximate 1.6 cm below the carina appears to be the most practicable method to optimize the CVCs placement among Chinese patients.
Conclusions
In summary, the mean length of extrapericardial SVC was 2.5 cm and the PR was average 1.6 cm lower than the carina among Chinese patients.
Acknowledgements
Funding: This study was partially supported by the Natural Science Foundation of Zhejiang province, China (LY14H030002). The funding sources played no role in the design, conduct, or reporting of this study.
Disclosure: The authors declare no conflict of interest.
References
- Schuster M, Nave H, Piepenbrock S, et al. The carina as a landmark in central venous catheter placement. Br J Anaesth 2000;85:192-4. [PubMed]
- Albrecht K, Nave H, Breitmeier D, et al. Applied anatomy of the superior vena cava-the carina as a landmark to guide central venous catheter placement. Br J Anaesth 2004;92:75-7. [PubMed]
- Kim MC, Kim KS, Choi YK, et al. An estimation of right- and left-sided central venous catheter insertion depth using measurement of surface landmarks along the course of central veins. Anesth Analg 2011;112:1371-4. [PubMed]
- Ryu HG, Bahk JH, Kim JT, et al. Bedside prediction of the central venous catheter insertion depth. Br J Anaesth 2007;98:225-7. [PubMed]
- Ridge CA, Litmanovich D, Molinari F, et al. Radiographic evaluation of central venous catheter position: anatomic correlation using gated coronary computed tomographic angiography. J Thorac Imaging 2013;28:129-33. [PubMed]
- Wirsing M, Schummer C, Neumann R, et al. Is traditional reading of the bedside chest radiograph appropriate to detect intraatrial central venous catheter position? Chest 2008;134:527-33. [PubMed]
- Gebhard RE, Szmuk P, Pivalizza EG, et al. The accuracy of electrocardiogram-controlled central line placement. Anesth Analg 2007;104:65-70. [PubMed]
- Stonelake PA, Bodenham AR. The carina as a radiological landmark for central venous catheter tip position. Br J Anaesth 2006;96:335-40. [PubMed]
- Dulce M, Steffen IG, Preuss A, et al. Topographic analysis and evaluation of anatomical landmarks for placement of central venous catheters based on conventional chest X-ray and computed tomography. Br J Anaesth 2014;112:265-71. [PubMed]
- Uchida Y, Sakamoto M, Takahashi H, et al. Optimal prediction of the central venous catheter insertion depth on a routine chest x-ray. Nutrition 2011;27:557-60. [PubMed]