Radical surgical resection after neoadjuvant targeted therapy in non-small cell lung cancer: a single-center retrospective study of 6 cases
Introduction
With the epidermal growth factor receptor (EGFR) tyrosine kinase inhibitor (TKI) recurrence, gefitinib is the first targeted drug to be approved for advanced non-small cell lung cancer (NSCLC) that failed to respond to chemotherapy (1). A great quantity studies show that gefitinib has fairly active anti-tumor activity, especially for tumors with mutations or a copy number gain of EGFR gene (2). However, there have been few data about the preoperative gefitinib treatment in NSCLC patients (3). At present, the first line treatment of patients with locally advanced NSCLC still mainly relay on neoadjuvant chemotherapy (4). While the effect of gefitinib as a neoadjuvant or preoperative therapy remains unclear (5). Preoperative neoadjuvant targeted treatment is a new departure (6).
To explore the efficacy of preoperative targeted adjuvant therapy, we describe one case of radical surgical resection of residual disease after dramatic response to gefitinib in patients with locally advanced lung adenocarcinoma harboring EGFR gene mutation in this report.
Methods
Patient
We retrospective collected 6 cases, clinical staging IIIA-IIIB from March 2017 to September 2018 (Table 1). This typical patient was a 43-year-old woman. She accepted the EBUS-TBNA first because complete resection of the tumor would not have been technically feasible. The pathological result of the 7th lymph node (LN) is adenocarcinoma while the L858R harbored a detectable mutation by the directed poly merase chain reaction-based sequencing analysis method. The patient accepted neoadjuvant gefitinib therapy for 8 weeks as the first-line therapy. The subsequent chest computed tomography (CT) examination had revealed that the lump located on the inferior left lobe and the mediastinal lymph nodes rebound significantly. The carcinoembryonic antigen (CEA) also descend from 20 to 7.2 ng/mL (6). Therefore, preoperative gefitinib treatment made it possible to perform radical resection in this case. Due to the patient have the indications for surgery, the lobectomy and mediastinal lymphadenectomy were performed.
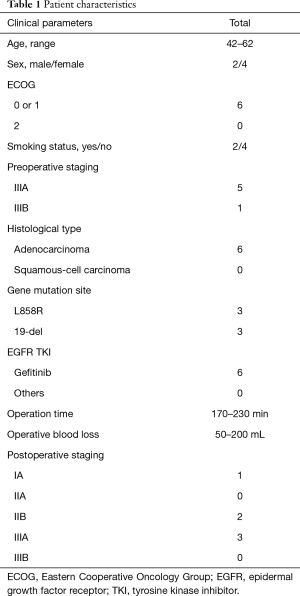
Full table
Operative technique
The surgery was performed under general anesthesia with double lumen tubes which ensure that the operated thoracic cavity had good visual field, along with contralateral one-lung ventilation. The patient was placed in a vertical lateral position, with a sponge mat under the right side of the chest. The left upper limbs were elevated to form a 90-degree angle with the trunk.
Three operating ports were used during the single-direction video-assisted thoracoscopic lobectomy. The three operating ports were located as follows: a 1.5-cm observation port was created in the 7th intercostal space at the left middle auxiliary line, a 3-cm incision was made in the 4th intercostal space at the left anterior line, and a 2-cm auxiliary port was made at the 7th intercostal space at the left posterior line. The operator stood at the abdominal side of the patient, and the assistants stood at the back side.
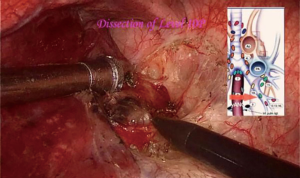
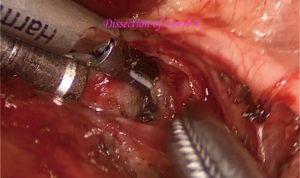
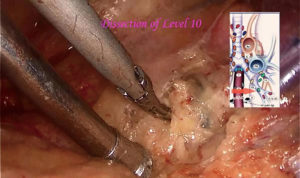
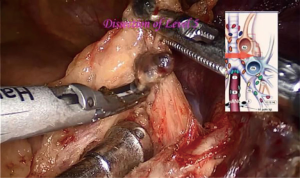
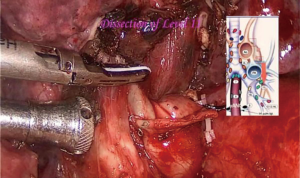
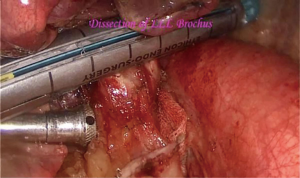
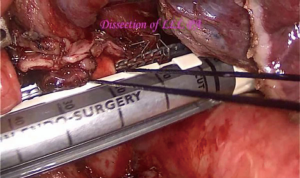
At first, the thoracoscope was inserted along the observation port, and the position of the tumor and the pleural cavity should be observed (1). With a thoracic exploration, the assistant inserted a forester forcep into the auxiliary port to track the left lower lobe towards the head side, to expose the left inferior pulmonary ligament (2). The metastatic mediastinal lymph node was dissected firstly before the lobectomy because the pathological result was confirmed by EBUS-TBNA before the neoadjuvant targeted therapy (4). The single-direction video-assisted thoracoscopic lobectomy was performed due to the fused oblique fissure (7). For traditional left lobectomy, the following structures are operated in the order: pulmonary vein—oblique fissure—pulmonary artery-poorly developed fissure—bronchus (3). In this case, the following structures are operated in this order: pulmonary vein—bronchus—pulmonary artery-fused oblique fissure.
The primary surgical procedure about the mediastinal lymph node dissection was illustrated below (Figures 1-8). The primary surgical procedure about lobectomy was illustrated below (Figures 9-11). The left inferior pulmonary vein was first isolated (Figure 9). The bronchus was isolated and dissected without flipping the lobe in the single-direction method (Figure 10). The inferior pulmonary artery was resected at last by endo straight cutting stapler (Figure 11). The fused pulmonary fissure was resected finally, and the specimen was removed.
Comments
Clinic result
The resected tumor exhibited components of adenocarcinoma. No metastasis was found in all the 11 resected lymph nodes in this case while the postoperative pathological result was ypT1N0M0, stage I. The patient was discharged without complications at the 5th postoperative days. The patient received targeted adjuvant therapy in 2 weeks after operation. The patient is still alive, without recurrence or metastasis for 12 months after the operation.
In our medical center, all the six patients with neoadjuvant targeted therapy were performed complete video-assisted thoracic surgery (cVATS) since Jan 2017. There is no conversion to hybrid VATS or thoracotomy. Neoadjuvant targeted therapy does not reduce the patient’s physical strength, allowing the patient to undergo surgery. Different from the cases who accepted neoadjuvant chemotherapy, no additional tissue adhesions, indistinct interface and increased fragility of the blood vessels were observed during the operation in these neoadjuvant targeted cases. The neoadjuvant targeted therapy eventually improves tumor resectability.
In conclusion, TKI therapy provided an alternative approach for neoadjuvant or preoperative treatment in patients with locally advanced NSCLC with EGFR mutations.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Liu M, Jiang G, He W, et al. Surgical resection of locally advanced pulmonary adenocarcinoma after gefitinib therapy. Ann Thorac Surg 2011;92:e11-2. [Crossref] [PubMed]
- Shen H, Zhong X, Ge XQ, et al. Surgical resection of lung adenocarcinoma without EGFR mutation after neoadjuvant gefitinib treatment. Clin Respir J 2010;4:192-3. [Crossref] [PubMed]
- Takamochi K, Suzuki K, Sugimura H, et al. Surgical resection after gefitinib treatment in patients with lung adenocarcinoma harboring epidermal growth factor receptor gene mutation. Lung Cancer 2007;58:149-55. [Crossref] [PubMed]
- Hishida T, Yoshida J, Aokage K, et al. Long-term outcome of surgical resection for residual or regrown advanced non-small cell lung carcinomas following EGFR-TKI treatment: report of four cases. Gen Thorac Cardiovasc Surg 2016;64:429-33. [Crossref] [PubMed]
- Kurishima K, Ohara G, Kagohashi K, et al. Adenosquamous cell lung cancer successfully treated with gefitinib: A case report. Mol Clin Oncol 2014;2:282-4. [Crossref] [PubMed]
- Zhou J, Ben S. Comparison of therapeutic effects of EGFR-tyrosine kinase inhibitors on 19Del and L858R mutations in advanced lung adenocarcinoma and effect on cellular immune function. Thorac Cancer 2018;9:228-33. [Crossref] [PubMed]
- Liu L, Che G, Pu Q, et al. A new concept of endoscopic lung cancer resection: Single-direction thoracoscopic lobectomy. Surg Oncol 2010;19:e71-7. [Crossref] [PubMed]