Lophomonas blattarum infection presented as acute exacerbation of chronic obstructive pulmonary disease
Introduction
Lophomonas blattarum (L. blattarum) is a rare protozoan, which parasitizes in intestinal tracts of some special arthropods, such as termites and cockroaches (1). The presenting data supports that L. blattarum is a kind of opportunistic pathogens, causing bronchopulmonary infection in immunocompromised cases, especially in the organ transplantation patients with immunosuppression treatment (2-4).
Chronic obstructive pulmonary disease (COPD) is defined as progressive and persistent airflow limitation with chronic cough, sputum, dyspnea and some other diversity symptoms (5). Acute exacerbation of chronic obstructive pulmonary disease (AECOPD) is characterized as worsen of symptoms beyond daily variation, which might result from bacterial and viral infection. On the other hand, due to the long term use of corticosteroids and bacterial colonization, bronchopulmonary infection is frequently seen in COPD patients, which might mimic or aggravate exacerbation of COPD. Here we presented a L. blattarum infection case, which was misdiagnosed as AECOPD initially.
Case (Figure 1)
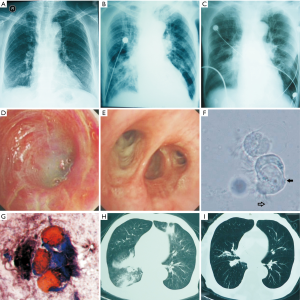
 , body of Lophomonas blattarum;
, body of Lophomonas blattarum;  , wave flagellates; (H) pulmonary CT scan presented bilateral effusion, infiltrated, at the twenty fifth day from onset; (I) pulmonary CT scan presented improvement and resolved of lesion, 3 months later after discharge.
, wave flagellates; (H) pulmonary CT scan presented bilateral effusion, infiltrated, at the twenty fifth day from onset; (I) pulmonary CT scan presented improvement and resolved of lesion, 3 months later after discharge.A 70-year-old male farmworker with COPD (group D) had been hospitalized 3 times in the previous 12 months for exacerbations. His latest pulmonary function showed forced expiratory volume in the first second was 0.92 L, 32% predicted; and forced vital capacity was 2.6 L, after bronchodilating. He was on inhaled tiotropium 18 mcg once daily and fluticasone-salmeterol 500/50 mcg twice daily. For the serious carbon dioxide retention (arterial CO2 pressure 55 mmHg in stable stage), this patient was ventilated with noninvasive Bipap (S/T-D Ventilatory Support System, inspiratory positive airway pressure: 12 cm H2O, and expiratory positive airway pressure: 4 cm H2O) 6 hours daily. Fortunately, except COPD history, this man donot have any other disease histories.
At an outside hospital, the patient complained of worsening cough, sputum and dyspnea for 5 days. Physical examination revealed a temperature of 36.2 °C, heart rate of 102 beats per minute, respiratory rate of 20 beats per minute, blood pressure of 120/80 mmHg and an oxygen saturation of 92% on 2 L/min nasal oxygen supplement. Lung examination only found coarse, but decreased breath sounds. And the other system examinations were all unremarkable. Blood routine revealed white blood cell count of 7.5×109/L and an increased neutriphil percentage of 80.3%. Chest radiography did not find any infiltration, masses and lymphadenopathy (Figure 1A). This patient was presumed as AECOPD with a possible infection of bronchus, and treated in the institute with intravenous ceftazidime and azithromycin, and nebulized ipratropium and budesonide. Due to the increased pCO2 of 60 mmHg, the Bipap ventilation was prolonged to 12 hours per day with the same index.
After 4 days of treatment, the patient was transferred to our ward emergently with a marked exacerbation of dyspnea and cough, and a newly unconsciousness. Physical examination revealed cyanosis and an oxygen saturation of 80% on 4 L/min nasal oxygen supplement. Lung examination showed decreased breath sounds, and small amount of bilateral rhonchi and rales, and the other signs were almost the same as previous. Blood routine showed: white blood cell count of 9.1×109/L and neutriphil percentage of 87.94%. The arterial gas analysis showed highly increased CO2 pressure, 145 mmHg, with a crucial PH 7.18. This critical case was diagnosed as hospital acquired pneumonia, COPD with pulmonary encephalopathy, and type 2 respiratory failure. He was nasal intubation immediately, and ventilated in synchronized intermittent mandatory ventilation mode. Bronchoscopy showed a lot of purulent sputum, diffusely swelling and congestion mucus on bronchus, especially in bilateral superior lobar trachea and right midtrachea (Figure 1D,E). Meropenem was used, plus bronchodilators, mucolytic and nutritional supports. Despite the strong treatment, the chest X-ray presented bilateral effusion, infiltrated and linear opacities (Figure 1B) with unimproved symptoms. The laboratory studies including erythrocyte sedimentation rate, glucose, liver test, renal function, IgE, human immunodeficiency virus, tuberculosis, virus and fungus were negative. Fortunately, the sputum smear directly from bronchoscopy revealed motile organism with wave flagellates, which was identified as L. blattarum (Figure 1F,G). Then intravenous tinidazole 0.4 g once daily had been administrated. One week later, the symptoms and images were improved (Figure 1C), and intubation ventilation was turned to noninvasive Bipap (S/T-D Ventilatory Support System, inspiratory positive airway pressure: from 16 to 12 cm H2O, and expiratory positive airway pressure: from 6 to 4 cm H2O). After discharge, tinidazole 0.5 g had been orally administrated twice daily for 1 month. The follow up found the variation of symptoms and image opacities were resolved (Figure 1H,I).
Discussion
L. blattarum is a rare and host-specific protozoan in the muggy environment (1), and it could be spread by waste and dust during the crawling of host. The infection of L. blattarum in only found in respiratory system so far (2-4), it might indicate the most possible transmitting pattern is air borne.Though it needs further study, it seems that L. blattarum infection is an organ specific disease, indicting bronchopulmonary epithelium and microenviroment might be beneficial for L. blattarum.
L. blattarum infection presents untypical symptoms, such as cough, sputum and dyspnea (2-4). All of these symptoms are commonly attributed to common bronchopulmonary infection or AECOPD, which might obscure the diagnosis and treatment. Reflecting in this case, it happened that the patient had worse respiratory symptoms and underlied with COPD. Though it was initially suspected as AECOPD, the empirical treatment for AECOPD did not show any improvement in the case. Even the ordinary sputum smear did not find any clues to protozoan and fungus infection. Diagnosis was delayed until the direct suction smear under bronchoscopy revealed the appearance of motive L. blattarum. This present case suggests the importantce of L. blattarum infection in the differential diagnosis of AECOPD and other common bronchopulmonary infection cases, especially who fails to empiric antibiotic treatments. As other cases, this patient recovered after the single tinidazole treatment, despite the failure of the initial antibiotic treatments. It seems tinidazole is enough for L. blattarum infection, and some other antibiotic or anti-fungus drugs might be unnecessary or even useless.
L. blattarum infection is so rare that only reported less than 70 cases in the whole world (2-4). It often based on immunocompromise, especially renal transplantation with receiving immunosuppression. Though high-dose inhaled corticosteroids have been demonstrated to increase the risk of bacteria, virus and fungus infection, this case is not a classical immunocompromised host. And we did not find any evidences of virus and fungus infection, which frequently occur in immunodeficiency cases. Since there are not any reliable L. blattarum infection models, the immunity pathogenesis is still unclear. There is an unbalance of CD8+ and CD4+ T cell in COPD pathogenesis (5). And the unbalance also exists in the protozoan infection. It is presumptively that COPD is an additional predisposing factor in L. blattarum infection beyond corticosteroids.
Sometimes, it is difficult to differentiate L. blattarum and bronchial ciliated cells. In Leifson’s stain, the bronchial ciliated cell is also presented with columnar shape, red nuclei, bluish cytoplasms, and inserted cilia, which is like waving flagella. However, the ciliated cells are often degeneration or necrosis in the bronchial secretion. In this case, these cells were still alive after 72 hours culture, indicating these cells were different from the bronchial ciliated cell. On the other hand, rather than meropenem and some other broad-spectrum antibiotics, the tinidazole brought exciting improvement in the case, suggesting there was L. blattarum infection. Because of the augment of chronic patients impairing the immunity by diseases or medications, the incidence of opportunistic diseases is mounting. Due to the specific host location, cases of L. blattarum infection are all found in warm and muggy districts (4). It suggests that chronic patients should keep clean and dry of residence and ventilation duct.
Conclusions
This case illustrated the misdiagnosis of L. blattarum, a rare opportunistic pathogen, until the bronchoscopy provided the positive direct sputum smear. It indicates though in the untraditional immunocompromised case, the suspect of opportunistic diseases is necessary, especially in the cases failed to improvement under empirical treatment.
Acknowledgements
Consent: This work was approved by the Ethical Committee of the Second Xiangya Hospital. Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Authors’ contributions: HZ carried out the following up and drafting. XK carried out the picture and radiograph collecting. XC participated the identification of Lophomonas blattarum HL and PC supervised the diagnosis and treatments in this case. YC diagnosed and treated this case, and coordinated and helped to draft the manuscript.
Funding: This study was supported by National Nature Science Foundation of China 30770931, 30800503, 81070039 and the National Natural Science Foundation of Hunan Province 09JJ3036.
Disclosure: The authors declare no conflict of interest.
References
- Ohkuma M, Noda S, Hongoh Y, et al. Inheritance and diversification of symbiotic trichonymphid flagellates from a common ancestor of termites and the cockroach Cryptocercus. Proc Biol Sci 2009;276:239-45. [PubMed]
- Wang Y, Tang Z, Ji S, et al. Pulmonary Lophomonas blattarum infection in patients with kidney allograft transplantation. Transpl Int 2006;19:1006-13. [PubMed]
- He Q, Chen X, Lin B, et al. Late onset pulmonary Lophomonas blattarum infection in renal transplantation: a report of two cases. Intern Med 2011;50:1039-43. [PubMed]
- Martinez-Girón R, van Woerden HC. Lophomonas blattarum and bronchopulmonary disease. J Med Microbiol 2013;62:1641-8. [PubMed]
- Vestbo J, Hurd SS, Agustí AG, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med 2013;187:347-65. [PubMed]


