A plastic whistle incarcerated in bronchus diagnosed fourteen years after ‘swallowed’: a case report
Tracheobronchial foreign body aspiration (FBA) is more often happened in younger children, and it rarely happens in school-age children (1,2). Most FBs are food or food-related, whereas the proportion of plastic FBs in US or worldwide is about 7% and 2% respectively (3). The most frequently reported symptoms, signs, radiological findings and complications may vary due to bronchial foreign bodies. We report a case with latent manifestations of bronchial foreign body in an adult and concerned with the clinical features of this.
A 23-year-old male went to the respiratory clinic of a university hospital with suspicion of FBA as he watched news which reported a child diagnosed FBA 5 years after choking. He had no respiratory history of interest or drug allergies. Upon being questioned further regarding his concerns, he admitted that he got “colds” every two or three months since swallowing a plastic toy 14 years ago. He was evaluated the next day of the incident by a pulmonologist, but chest X-ray and upper gastrointestinal barium meal revealed nothing specific.
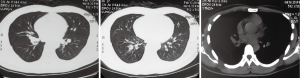
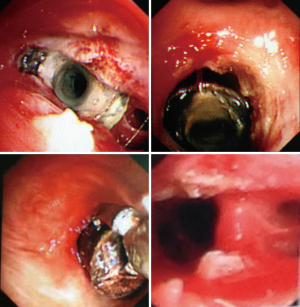
Before the diagnostic bronchoscopy, a computed tomography (CT) was performed at local hospital, which only reported slight infection at right lower lob (Figure 1). Flexible bronchoscopy revealed inflammatory bronchial stricture of the bronchus intermedius. After the obstructing lesion released, a bronchoscope with 4.8 mm external diameter can pass through and found that the foreign body was embedded in granulation tissue of basal stem bronchus (Figure 2). Further treatment was not performed considering the complexity of the case. He was advised to be hospitalized for the retrieval and returned home without any uncomfortable. That night he presented with chills, fever (39 degree centigrade) and cough productive of white sputum. He was admitted to Emergency Room and then transferred to in-patient department. On examination he was febrile, and clubbed-fingers could be observed. Auscultation of the chest revealed rhonchi and wheezing involving right lower lung. Tactile fremitus was decreased at right lower thorax. Pulse oxygen saturation was 97% on room air. An emergency CT scan reported multiple opacities and patchy shadows of right lower lung, and mucous plug was suspected in bronchus (Figure 3). Symptoms remitted as intravenous avelox (0.4 g per day) was given to patient. To reduce the oedema of bronchial mucous, 15 mg methylprednisolone per day was given to him.
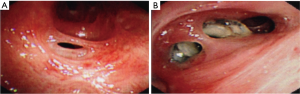
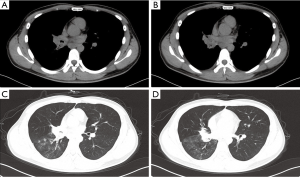
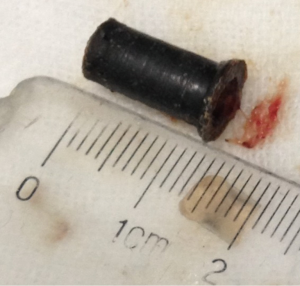
Retrieval was successfully performed by flexible bronchoscopy (Figure 4) under general anesthesia. The foreign body was found to be a pin-shaped plastic whistle with a larger head after the adhesion released. The bronchial stenosis is released by electrocautery, at last the foreign body was removed by forceps after several attempts (Figure 5).
FBA is easily overlooked by physicians when history and manifestations are not typical. In this case, symptoms such as coughing, dyspnea or expectoration are not remarkable after the hollow plastic cylinder aspirated; unlike other FBs, there is no obvious airway obstruction, no respiratory function compromises, but mild bronchus stricture due to a 14-year irritation. Take home message is: plastic foreign body could be overshadowed by mucous secretions or the bronchial wall. Carefully physical examination and scrutinize over CT scans may provide clues of FBA. Flexible fiberoptic bronchoscopy under adequate anesthesia is indicated both in establishing diagnosis and attempting removal of foreign bodies with bronchial stricture. In these compromised patients, the airway might need repeated bronchoscopy to release adhesion and debride secretion, and to some extent surgical treatment might be needed. To avoid worsened stenosis after bronchoscopy, patient should have regular check-ups to monitor progress, if necessary balloon bronchoplasty should be performed (4). For better diagnosis and clinical management of such rare cases, more cases needed to be reported (Video 1).
Acknowledgements
We thank the staff of the Department of Endoscopy Centre, West-China Hospital, Sichuan University.
Disclosure: Xin Wang does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript. Guowei Che received National Science Foundation (NO.81071929, to Guowei Che) as funding for lung cancer related research.
References
- Gang W, Zhengxia P, Hongbo L, et al. Diagnosis and treatment of tracheobronchial foreign bodies in 1024 children. J Pediatr Surg 2012;47:2004-10. [PubMed]
- Huankang Z, Kuanlin X, Xiaolin H, et al. Comparison between tracheal foreign body and bronchial foreign body: a review of 1,007 cases. Int J Pediatr Otorhinolaryngol 2012;76:1719-25. [PubMed]
- Kaushal P, Brown DJ, Lander L, et al. Aspirated foreign bodies in pediatric patients, 1968-2010: a comparison between the United States and other countries. Int J Pediatr Otorhinolaryngol 2011;75:1322-6. [PubMed]
- Jimenez Rodriguez BM, de Jesús SC, Merinas López CM, et al. Bronchial stenosis after iron pill aspiration. J Bronchology Interv Pulmonol 2013;20:96-7. [PubMed]