Takayasu’s arteritis misdiagnosed as mediastinal malignant lymphoma: a case report and review of the literature
Takayasu’s arteritis (TA) is a rare chronic granulomatous large-vessel vasculitis, predominantly the aorta and its major branches. Due to lack of characteristic clinical manifestations, it’s easy to be misdiagnosed or never diagnosed. Recent studies have found that 18F-FDG PET/CT not only could show the morphological changes of artery wall but also indicate the tissue metabolic activity, providing a powerful evidence for the early detection of TA (1). In this paper, we reported a TA case of young female even was misdiagnosed as infectious diseases due to persistent fever for one month, but no response to anti-infection treatment. 18F-FDG PET/CT showed abnormal changes of aorta and mediastinal lymphoma enlarged. She was again misdiagnosed as mediastinal malignant lymphoma, due to insufficient understanding about TA. Mediastinoscope biopsy was performed and found that tissue adjacent to the aortic arch pathological changes were in accord with the TA, the condition was greatly improved after treated with glucocorticoid.
Case report
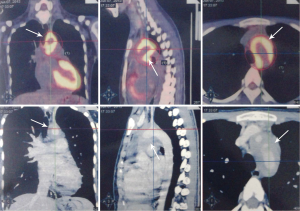
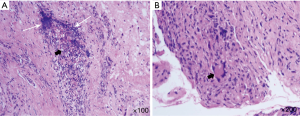
A 19-year-old female patient was enrolled in a local hospital due to “persistent fever more than one month”. The physical examinations on admission were as follows: body temperature 38.7 °C; pulse 105 times/min; breathing rate 20 times/min; BP 110/73 mmHg (1 mmHg =0.133 kPa). Other physical examinations were normal on admission and medical history and family history were negative. The results of blood tests including, blood biochemistry, immunology and oncology examinations, as well as Weil-Felix and Widal test on admission were normal, except the erythrocyte sedimentation rate was up to 64 mm/h. Infectious diseases was considered firstly and antibiotic with clindamycin, moxifloxacin and cefuroxime were successively administrated, but the fever remained after treated for two weeks. After that, the patient was transferred to a tertiary hospital for further treatment. Medical examination was basically same to before. In laboratory tests, no obvious abnormities were seen, except the higher erythrocyte sedimentation rate of 89 mm/h and a positive serum mycoplasma antibody. The causes of fever were analyzed including infectious disease (might be infective endocarditic or tuberculosis), tumor disease or connective tissue disease. Advanced antibiotics including imipenem/cilastatin and azithromycin were administrated for the anti-infection treatment, but the fever was still persistent, the highest temperature up to 39 °C. In order to differentiate from tumor, the 18F-FDG PET/CT was performed and result found that soft tissue thickening adjacent to the aortic arch and descending aorta thickening was visible as well as the lumen of aortic arch narrowed, the standard uptake value (SUV) of thickened soft tissues was 9.4 (Figure 1), some enlarged lymph nodes with SUV 3.9 in mediastinal were visible. Mediastinal malignant lymphoma was suspected and mediastinoscopy was carried out to obtain lymph nodes and thickened soft tissue for pathological examination. Biopsy report shown that the lymph node tissue, structure normal, hyperplasia of lymphoid follicles, abnormal lymphocytes no found. Special staining examination including PAS, anti-acid, hexamine silver were all negative, so reactive hyperplasia of enlarged lymph node was considered and malignant diseases were excluded. The patient still had a fever, transferred to our institute for further treatment. The physical examination results on admission were as follows: body temperature 38.5 °C; BP 113/70 mmHg (upper left limb); 108/68 mmHg (upper right limb); the rest were negative as before. Reviewing the soft tissue pathological slides again, we found that many lymphocytes and plasma cells infiltration were visible in vessel wall and the elastic fibers were fractured, smooth muscle fibers were necrotized in small vessel. Multinucleated giant cell granulomatous lesions can be visualized. These pathological changes were in accord with arteritis (Figure 2). TA was diagnosed and oral 40 mg/d of prednisone was administrated according to the weight of the patient was 45 kg. The body temperature gradually decreased after treated for three days, and became normal after one week, the dose of prednisone was gradually reduced after treated for one month, at present patient is in a stable condition after treated for three months, and in good health. For economic reason, the patient couldn’t offer again PET/CT examination.
Discussion and literature review
TA is commonly seen in Japan, Southeast Asia, India and Mexico, which was firstly described in 1905 by Mikito Takayasu. TA commonly occurs in people younger than 30 years old, account for approximately 90%, and less in people older than 40 years old (2). Females are more likely to be affected than males, which was once regarded as “Asian young women disease”, but recently founded to occur in men, the morbidity of male:female ratio is about 1:8-9. The prevalence of TA appears to vary greatly in different countries, about 1-2/million in Japan and 0.8/million in Sweden and in the UK (3,4). The etiology is still unknown, may be associated with immune injury caused by infection. Pathological manifestations are as follows: lymphocytes and plasma cells infiltration are visible in the vessel wall at early period, and occasional polymorphonuclear neutrophils and multinucleated giant cell infiltration. Inflammation causes the vessel adventitial thickening, elastic fibers and smooth muscle fiber necrosis of the tunica media, and intimal hyperplasia, resulting in the vessel stenosis and occlusion of lumina. Local aneurysm was formed because elastic fibers were severely damaged in the tunica media (5). Clinical manifestations can be divided into two phases, in the early phase patients may complain of symptoms including fever, weight loss, fatigue, myalgia, headache and other uncharacteristic presentations, vascular stenosis and occlusion are involved with the development of disease, which can be divided into four types according to the anatomical location of the affected arteries: brachiocephalic arterial type, the stenosis and occlusion of carotid and vertebral artery lead to brain ischemia, subclavian artery involvement leads to the unilateral or bilateral upper limb weakness, cold, pain numb, pulse weak or disappeared (pulselessness); thoraco-abdominal arterial type, the thoraco-abdominal aorta involvement is characterized with lower limb weakness, pain and intermittent claudication; Renal arterial type, appears high blood pressure; advanced pulmonary artery involvement appears pulmonary hypertension (2).
TA is easy to be misdiagnosed and early diagnosis is difficult. The mean delay in diagnosis varied from 10 months to 4.9 years (6,7), 91% patients reported seeing more than one physician prior to diagnosis (8). Renal artery vasculits was often misdiagnosed as hypertension (9), aorta vasculitis was often confused with other artery lesions, like syphilitic arteritis, tuberculous arteritis, giant cell arteritis, Bechet’s disease and atherosclerosis. In this case, the patient was a young female, mainly complaining of fever without obvious deficiency in limb artery blood supply, no marked blood pressure different between bilateral upper limbs was found in physical examinations, and no vascular murmur was heard on the subclavian aorta and abdominal aorta. She had been misdiagnosed as infectious diseases, no response to antibiotic treatment. To exclude the possibility of tumor diseases, 18F-FDG PET/CT was performed, the results showed an obvious thickening of soft tissue adjacent to the aortic arch and descending aorta wall, with active metabolism, as well as a mediastinal lymph node enlargement with active metabolism. Due to insufficient understanding of 18F-FDG PET/CT abnormal manifestation about the condition, it’s misdiagnosed as malignant lymphoma. Mediastinoscopy was performed to obtain mediastinal lymph nodes and the thickened soft tissues for confirm diagnosis. Pathological results showed that no abnormal lymphocyte was present in lymph node tissue, in the thickened soft tissue the manifestations were in accord with arteritis. Based on the above results, TA was considered. After treated with glucocorticoid, the body temperature gradually decreased to normal, and the condition was improved. For economic reason, the patient couldn’t afford a PET/CT review again, but according to the clinical characteristics, PET/CT and pathological results, as well as the glucocorticoid treatment respond, it’s in accord with the diagnosis of TA. Although significant blood pressure discrepancy between bilateral upper limbs and ischemic change were often appeared in the aortic arch type TA, but no significant signs were found in the physical examinations of this patient, which might be due to an unobvious stenosis and occlusion in subclavian artery and vertebral artery. TA is one kind of autoimmune disease, corticosteroids or combined with immunosuppressant therapy at early period can relieve the inflammation of blood vessel wall, avoid vascular injury and improve the prognosis. But the early diagnosis of TA is extremely difficult. Recent studies have found that 18F- FDG PET/CT has high sensitivity and specificity for the early diagnosis of TA, but also can judge the curative effect (1,10).
Percutaneous arterial angiography was the gold standard for the diagnosis of TA, but its invasiveness, the damage of X-ray radiation and contrast agent limited the clinical application. More important reason was that angiography indirectly revealed the luminal lesions only through the filling defect of contrast agents, couldn’t display the structure and morphology of blood vessel wall, lack of early diagnostic capacity (2). 18F-FDG PET/CT can not only display the anatomical morphological changes of lesions with CT image, but also reflect the cellular FDG metabolic activity. Therefore, it’s widely used in the diagnosis of tumor and inflammatory lesions, as well as the judgment of curative effect (11). Some recent studies have shown that 18F-FDG PET/CT have value in early diagnosis of TA. Kobayashi et al. (12) found that in 11 cases of acute active TA, 2 cases were characterized with obviously concentrated 18F- FDG in vascular system, whose SUVmax were 2.7 or higher, other 9 cases of mild concentrated, whose SUVmax were between 1.2 to 2.3; for the other 3 cases of inactive TA, SUVmax were 1.2 or less; for the 6 cases of healthy subjects, SUVmax were 1.3 or less. Setting SUVmax at 1.3 as the cut-off, the sensitivity of 18F-FDG PET/CT for the diagnosis of TA was 90.9%, specificity 88.8%. Research believed that 18F-FDG PET/CT were helpful to the early diagnosis of TA, as well as the confirmation of the location of lesions and scope. Webb M, et al. (13) found that the sensitivity and specificity of 18F-FDG PET/CT for diagnosing TA were 92% and 100%, respectively, negative and positive predictive value were 85% and 100%, respectively. Andrews J, et al. (14) reported that 18F-FDG PET/CT provided a more favourable basis for the judgment of disease activity than arteriography. In this case, although PET/CT examination had found abnormal manifestations of the aorta, but due to insufficient understand about the rare disease, the attention only focused on the enlarged mediastinum and metabolically active lymph nodes, mediastinal malignant lymphoma was considered, and performed mediastinoscopy, increasing the pain and economic burden of patient.
Through retrospective analysis of this case and review of the pertinent literatures, we hope to improve the understanding of TA in physicians of different clinical departments. In clinical work, attention should be paid to young patients of persistent fever, which failed to antibiotic treatment, as well as young patients with high blood pressure, whose unilateral limb was cold, pain and pulselessness, it should arouse a suspicion of TA. In physical examination, it’s requisite to measure the blood pressure of bilateral upper limbs, auscultate the subclavian aorta and abdominal aorta area, also 18F-FDG PET/CT is suggested to visualize the morphology and metabolism of systemic aortas.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Lee KH, Cho A, Choi YJ, et al. The role of (18) F-fluorodeoxyglucose-positron emission tomography in the assessment of disease activity in patients with takayasu arteritis. Arthritis Rheum 2012;64:866-75. [PubMed]
- Johnston SL, Lock RJ, Gompels MM. Takayasu arteritis: a review. J Clin Pathol 2002;55:481-6. [PubMed]
- Koide K. Takayasu arteritis in Japan. Heart Vessels Suppl 1992;7:48-54. [PubMed]
- Watts R, Al-Taiar A, Mooney J, et al. The epidemiology of Takayasu arteritis in the UK. Rheumatology (Oxford) 2009;48:1008-11. [PubMed]
- Mason JC. Takayasu arteritis--advances in diagnosis and management. Nat Rev Rheumatol 2010;6:406-15. [PubMed]
- Kerr GS, Hallahan CW, Giordano J, et al. Takayasu arteritis. Ann Intern Med 1994;120:919-29. [PubMed]
- Ishikawa K, Maetani S. Long-term outcome for 120 Japanese patients with Takayasu’s disease. Clinical and statistical analyses of related prognostic factors. Circulation 1994;90:1855-60. [PubMed]
- Abularrage CJ, Slidell MB, Sidawy AN, et al. Quality of life of patients with Takayasu’s arteritis. J Vasc Surg 2008;47:131-6; discussion 136-7. [PubMed]
- Chaudhry MA, Latif F. Takayasu’s arteritis and its role in causing renal artery stenosis. Am J Med Sci 2013;346:314-8. [PubMed]
- Mavrogeni S, Dimitroulas T, Chatziioannou SN, et al. The role of multimodality imaging in the evaluation of Takayasu arteritis. Semin Arthritis Rheum 2013;42:401-12. [PubMed]
- Jerusalem G, Warland V, Najjar F, et al. Whole-body 18F-FDG PET for the evaluation of patients with Hodgkin’s disease and non-Hodgkin’s lymphoma. Nucl Med Commun 1999;20:13-20. [PubMed]
- Kobayashi Y, Ishii K, Oda K, et al. Aortic wall inflammation due to Takayasu arteritis imaged with 18F-FDG PET coregistered with enhanced CT. J Nucl Med 2005;46:917-22. [PubMed]
- Nathan DM, Buse JB, Davidson MB, et al. Management of hyperglycemia in type 2 diabetes: A consensus algorithm for the initiation and adjustment of therapy: a consensus statement from the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care 2006;29:1963-72. [PubMed]
- Andrews J, Al-Nahhas A, Pennell DJ, et al. Non-invasive imaging in the diagnosis and management of Takayasu’s arteritis. Ann Rheum Dis 2004;63:995-1000. [PubMed]


