
Lung volume reduction surgery in patients with low diffusion capacity
Lung volume reduction surgery (LVRS) has been shown to reduce dyspnoea and provide symptomatic improvement for a sub-set of patients with severe emphysema. The National Emphysema Treatment Trial (NETT) demonstrated prognostic benefit in those with heterogenous disease, upper lobe predominance, and low baseline exercise capacity (1). This trial also identified patients at high risk of early mortality over the baseline risk of usual care. These patients had a forced expiratory volume in one second (FEV1) of <20% predicted and either homogenous disease or diffusion capacity (DLCO) <20% predicted. The perceived high risk of LVRS has reduced physician willingness for referral, despite its proven benefits (2).
Low DLCO is well recognized as a risk factor for all lung resections, irrespective of procedure. The primary concern is that if DLCO is too low, there will be insufficient diffusion capacity in the remaining lung parenchyma post-resection. In the NETT, DLCO was measured but was not an exclusion factor for the trial (1,3). LVRS aims to resect largely non-functioning lung parenchyma and improve respiratory mechanics and so low pre-operative DLCO may not be a contraindication to this surgery. Peri-operative risk may be further increased, due to the stresses of single lung ventilation placed on the respiratory reserve. Low DLCO and reduced respiratory reserve place this cohort of patients at higher perioperative risk and this impacts on their access to LVRS.
In our centre, all patients undergoing surgical intervention for emphysema are discussed in a specialist LVRS multidisciplinary team meeting (MDT) (4). Patient specific factors and disease characteristics are considered to identify patients most appropriate for LVRS but also possible candidates for the newer, less invasive, endobronchial procedures of endobronchial valves (EBV) or endobronchial coils (EBC).
Individualised patient risk is calculated for all potential LVR candidates using the Glenfield BFG score, which allows better decision making on whether to proceed with LVR and which intervention may be most appropriate. This approach has seen a reduction in our local mortality rate. This risk prediction score was developed by analysis of various factors independently predicting 90-day mortality. The multivariate analysis factors associated independently with death were: body mass index (BMI) <18.5 kg/m2 [odds ratio (OR) 2.83, P=0.059], FEV1 <0.71 L (OR 5.47, P=0.011) and TLCO <20% (OR 5.56, P=0.031). A risk score was calculated and a total score assigned. Area under the receiver operating characteristic (AUROC) for the risk score was 0.80 and a better predictor than individual components (P<0.01) (4). Importantly the patients are offered a realistic risk benefit discussion as an informed decision can be made based on multiple risk factors, rather than individual components (5).
A recent paper by Caviezel et al. [2018] demonstrated that DLCO actually significantly improves post-LVRS in patients with a pre-operative DLCO less than 20%, strengthening the argument that resection of non-contributing parenchyma increases function in the remaining lung tissue. The series reported no mortality in this “higher risk” patient group but did show increased post-operative complications (prolonged air leak >7 days) when compared to patients with a DLCO >20% (48% versus 35%) (6). Caviezel et al. concluded that LVRS should be carefully considered in patients with reduced transfusion factor because of potentially significant benefits and, in their experience, avoidance of the need for lung transplantation.
In our centre we have performed 22 LVRS procedures in patients with DLCO less than, or equal to, 20% from September 1997 to July 2015. Baseline characteristics and pulmonary function tests are shown in Table 1. All surgical procedures were unilateral video-assisted thoracoscopic surgery (VATS), apart from one, which was initially VATS then converted to open. The 30-day mortality was 13.6% (3 patients, including the patient who had a VATS converted to open procedure). All patients who died developed lower respiratory tract infections post-operatively and died as a result of this; one of these patients had actually been discharged but later developed infection and died in their local hospital on post-operative day 21. The median air leak duration was 13 days (interquartile range, 8–20 days).
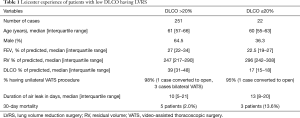
Full table
Unfortunately, post-operative pulmonary function testing in the DLCO ≤20% patients has been limited due to the large referral base. The median DLCO at 1 year post-surgery was 23% (interquartile range, 16–32%), median FEV1 24.5% predicted (interquartile range, 20.5–33.3%) and median residual volume (RV) 223% (interquartile range, 201–243% predicted). Although these appear to show improvement post-operatively, there is insufficient data for statistical analysis. Our cohort is slightly different from the Swiss cohort as we cater to a population covering areas which were formerly part of the British mining industry with possible greater compromise in their respiratory reserve.
It is our opinion LVRS in patients with low transfusion factor may be higher risk than patients with higher DLCO but patients should not be excluded from surgical intervention on the basis of this alone as the surgery remains potentially beneficial. Each patient’s case should be assessed and discussed in a specialist MDT and the risks and benefits of all potential options for intervention considered and appropriately discussed with the patient. Further work is required to establish the most appropriate intervention for these higher risk patients.
Acknowledgements
Funding: Dr. Greening is funded by a NIHR post-doctoral fellowship (PDF-2017-10-052). Support was also provided by the NIHR Leicester Biomedical Research Centre-Respiratory Theme.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Disclaimer: The views expressed in this publication are those of the author(s) and not necessarily those of the NHS, the National Institute for Health Research, Health Education England or the Department of Health.
References
- Fishman A, Martinez F, Naunheim K, et al. A randomized trial comparing lung-volume-reduction surgery with medical therapy for severe emphysema. N Engl J Med 2003;348:2059-73. [Crossref] [PubMed]
- McNulty W, Jordan S, Hopkinson NS. Attitudes and access to lung volume reduction surgery for COPD: a survey by the British Thoracic Society. BMJ Open Respir Res 2014;1:e000023. [Crossref] [PubMed]
- National Emphysema Treatment Trial Research Group, Fishman A, Fessler H, et al. Patients at high risk of death after lung-volume-reduction surgery. N Engl J Med 2001;345:1075-83. [Crossref] [PubMed]
- Rathinam S, Oey I, Steiner M, et al. The role of the emphysema multidisciplinary team in a successful lung volume reduction surgery programme†. Eur J Cardiothorac Surg 2014;46:1021-6; discussion 1026. [Crossref] [PubMed]
- Greening NJ, Vaughan P, Oey I, et al. Individualised risk in patients undergoing lung volume reduction surgery: the Glenfield BFG score. Eur Respir J 2017;49. [Crossref] [PubMed]
- Caviezel C, Schaffter N, Schneiter D, et al. Outcome After Lung Volume Reduction Surgery in Patients With Severely Impaired Diffusion Capacity. Ann Thorac Surg 2018;105:379-85. [Crossref] [PubMed]


