
ICD-10-CM/PCS: potential methodologic strengths and challenges for thoracic surgery researchers and reviewers
Background
The International Classification of Diseases, 10th Revision (ICD-10), is a set of agreed upon diagnosis codes developed by the World Health Organization (WHO) as part of its Family of International Classifications. This system provides a robust coding system for classifying diagnoses and other clinical concepts. The previous iteration, the International Classification of Diseases, 9th Revision (ICD-9), was developed by the WHO in 1975. Soon after, the National Center for Health Statistics (NCHS) applied the WHO’s system to classify diseases and morbidities in the inpatient hospital setting, creating the ICD-9 Clinical Modification (ICD-9-CM), comprising approximately 14,000 different diagnosis codes (1). An additional classification for procedures (not part of the WHO system) was added as Volume 3 of ICD-9-CM, comprising approximately 4,000 procedure codes. This system was adopted by most payers in the United States for managing provider payments, at the behest of the Health Care Financing Administration (HCFA), which required it in documentation of diagnosis and procedures for billing purposes in 1989. The HCFA was renamed to the Centers for Medicare and Medicaid Services (CMS) in 2001, and ICD-9-CM was adopted as a required code set for covered entities under the Health Insurance Portability and Accountability Act (HIPAA) transaction standards.
With the ongoing rapid expansion of diagnoses since 1975, the WHO published ICD-10 in 1993. The ICD-10 Clinical Modification (ICD-10-CM), developed by the NCHS in 2002, contains approximately 68,000 diagnosis codes (2). The ICD-10 Procedure Coding System (ICD-10-PCS), built by HCFA and 3M Health Information Systems and initially released in 1998, encompasses nearly 73,000 procedure codes (3). After several delays, CMS finally required providers and payers to transition to ICD-10-CM/PCS on October 1st, 2015, 22 years after the WHO first published the 10th revision.
ICD-9-CM has been utilized extensively for large database health services research studies evaluating thoracic surgical outcomes (4-6). ICD-9-CM, Volume 3, has been used in a number of thoracic surgical outcome studies, including those demonstrating positive volume-outcome relationships in video-assisted thoracic surgery (VATS) (7), increasing utilization of VATS over open thoracotomy from 2010–2014 (8), and decreased complication rates and shorter hospital stays among patients undergoing robotically assisted as opposed to VATS lobectomy (9). ICD-9-CM has been an important tool supporting the use of large, readily available administrative datasets in healthcare quality and surgical outcomes research. With the transition to ICD-10-CM/PCS, it is vital to understand the changes involved in the code structure, and how these will affect study design and dataset analysis. We anticipate that health services research with ICD-10-CM/PCS codes will be challenged in selecting appropriate codes and understanding how those code choices impact study methodology, accuracy of results, interpretation of data and the ability to compare studies from different institutions. There are currently no large-scale studies of surgical outcomes utilizing the ICD-10-CM/PCS coding system, though these types of studies are on the horizon given that data from 2016, the first full year of use of ICD-10-CM/PCS, are becoming available. The purpose of this review is to describe ICD-10-CM/PCS, demonstrate the strengths of the new format relative to thoracic surgical research and reveal potential challenges that may be encountered in utilizing administrative datasets with ICD-10-CM/PCS codes.
Structure of ICD-10-CM
ICD-10-CM describes diagnosis codes used for a variety of purposes, featured prominently in hospital, ambulatory surgical and clinic reimbursement (10). Each code consists of 3 to 7 alphanumeric characters starting with a letter and containing a decimal point after the third character. The first three characters define which of the 21 chapters of disease categories contain the pathology in question. For instance, malignancies of the respiratory tract or other intrathoracic organs are contained in the C30 through C39 section. Specifically, lung cancer would be defined by C34.x, where “x” indicates additional numeric values to describe anatomic locations for a malignant lung neoplasm including laterality, upper, middle, lower lobe, overlapping sites or otherwise unspecified pulmonary sites. ICD-10-CM presents 16 different codes for lung cancer due to the inclusion of laterality options in the disease definition (Table 1).
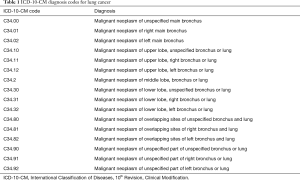
Full table
Structure of ICD-10-PCS
ICD-10-PCS provides the facility billing framework for procedures utilized by most hospital systems, as opposed to the Current Procedural Terminology (CPT) coding system (maintained by the American Medical Association) which is more frequently used for professional service billing by physician groups in the United States (11). While CPT codes often describe procedures in the context of a specific disease process, ICD-10-PCS procedures remain nonspecific to an underlying disease. A combination of seven alphanumeric characters with no decimal points make up every ICD-10-PCS code, with each character describing a unique aspect of the procedure definition, as seen in the example of a thoracoscopic left upper lobectomy (Figure 1). The first character represents the “Section” of the ICD-10-PCS from which the procedure derives, with virtually all surgical procedures found under “0” for “Medical and Surgical.” The second character defines the “Body System,” with “B” representing the Respiratory System. The “Operation” character is important in defining the actual physical action performed during the procedure. These “Operation” definitions include 31 possible options, each of which has a precise definition that may not comport with use of these terms outside of the context of coding. Thus, users must carefully select the appropriate “Operation(s)” in determining which code(s) apply. In the aforementioned example, “T” represents “resection.” Once an “Operation” is chosen, the fourth character represents the “Body Part,” giving precise definitions to distinguish laterality as well as anatomic components such as the pulmonary lobe that was resected. The fifth character, “Approach”, provides the full spectrum of potential surgical approaches such as “percutaneous endoscopic,” which indicates a thoracoscopic or laparoscopic technique, and “via natural or artificial opening, endoscopic” for bronchoscopic procedures. The sixth character, “Device”, provides supplemental information on any implantation of autologous or synthetic tissues. The final character “Qualifier” provides unique additional information for each type of “Operation”.
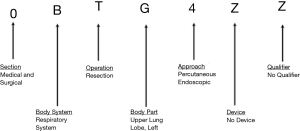
A sublobar resection such as a wedge resection can be distinguished from a lobectomy by the “Operation” character of “B” for “excision,” indicating removal of a portion of rather than the full anatomic body part as defined by the “Body Part” characteristic (Figure 2). Additionally, the “Qualifier” portion can be coded as “X” when a procedure is done for diagnostic rather than therapeutic purposes, as seen in the example of an open right upper lobe diagnostic wedge excision. A total pneumonectomy would be coded with a “T” (resection) for the “Operation” character, but the distinction from a lobectomy comes from the “Body Part” designation of “K” or “L” for the right lung or left lung in totality, respectively.

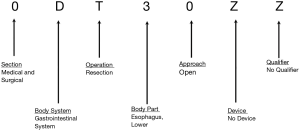
By comparison, an esophagectomy is coded again in the “0” “Section” followed by “D” for “Body System” representing the gastrointestinal system. One example of an esophagectomy utilizes the “Operation” characteristic of “T” indicating a resection (Figure 3), however the use of an excision “Operation” characteristic of “B” seems equally appropriate because the boundaries of the body part options under 0DB and 0DT are not precisely defined, nor are surgeons likely to always describe the extent of esophageal resection in such a way that coders could readily determine whether the upper, middle, or lower esophagus was “excised” or “resected.” Coders could conceivably describe a transhiatal esophagectomy using the “Operation” root of “extraction” (0DD). The “Body Part” gives some detail as to the location of the tumor and which portion of the esophagus was resected, with “3” representing the lower third of the esophagus. There is some additional detail available with a “Body Part” of “4” representing an esophagogastric junction resection. Resection involving more than one third of the esophagus but not a total esophagectomy (which would be signified by a “Body Part” indicator of “5”, would require either a code for “excision” of the entire esophagus or “resection” of more than one esophageal body part. Similar to pulmonary resections, the “Approach” character allows for distinction between open and minimally invasive procedures, with “0” indicating an open approach, “3” for “percutaneous,” “4” for “percutaneous endoscopic,” “7” for “via natural or artificial opening,” and “8” for “via natural or artificial opening, endoscopic” options, depending on whether the “resection” or “excision” root applies. There is no additional detail in the “Device” or “Qualifier” characteristics for esophageal “resection” procedures.
Strengths of ICD-10-CM/PCS
With the expansion in number of diagnosis and procedure codes available in ICD-10-CM/PCS, there is new detail within each code that can benefit both health facilities and researchers. For instance, while ICD-9-CM distinguished between upper, middle and lower lung lobes as the site of malignancy, ICD-10-CM adds specificity for laterality. ICD-9-CM previously redundantly coded esophageal malignancies either as cervical, thoracic or abdominal, as well as either upper, middle or lower third of the esophagus. ICD-10-CM simplifies the diagnoses to neoplasms of the upper, middle or lower third of the esophagus, while adding a designation for overlapping sites of the esophagus.
The transition to ICD-10-PCS provides more specificity to track details of the operation. ICD-10-PCS provides in-depth anatomic specificity through the “Body Part” designation. Lobectomies can be designated by lobe as well as laterality, a distinction absent from the CPT coding system. Lobectomies can be defined in significant detail using the “resection” “Operation” designation, with 12 possible unique ICD-10-PCS codes defining a lobectomy (Table 2). Wedge resections and segmentectomies, while not differentiable from each other, can be coded with significant anatomic detail utilizing the “excision” “Operation” designation. Diagnostic and therapeutic excisions can be distinguished with the “Qualifier” characteristic. There are 36 clinically plausible codes in ICD-10-PCS for defining a wedge resection or segmentectomy (Table 3). Of note, one must consider that a wedge resection might be coded correctly, albeit with less anatomic detail, utilizing the “Body Part” designations “K” and “L” for right lung and left lung, respectively, particularly if coders are unable to discern from the available documentation which lobe of the lung was involved. Such “Body Part” designations are not included for lobectomies (Table 2) as they would instead represent a pneumonectomy when paired with a “resection” “Operation” designation. Also, codes with approaches other than “open” or “percutaneous endoscopic” for lung tissue excisions (0BB) could not plausibly involve segmentectomy or wedge excision (Table 3), and instead would represent primarily bronchoscopic or percutaneous needle biopsies.

Full table
Full table
There is significant specificity under “Body Parts” for bronchial anatomy, allowing for the pairing of a code for a lobectomy “resection” with that of the appropriate bronchial “resection” to describe a sleeve lobectomy. One could even use an isolated “resection” or “excision” code with the “Body Part” of “Main Bronchus, Right” or “Main Bronchus, Left” to describe a bronchoplastic sleeve resection without lobectomy that would be used for an isolated airway tumor.
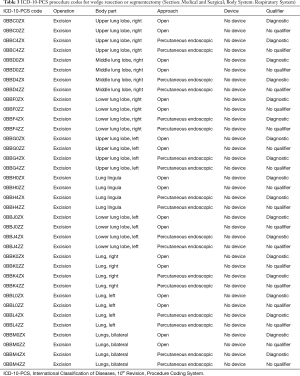
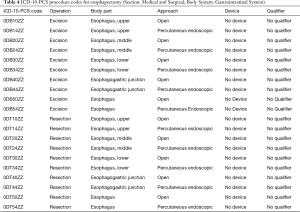
Esophagectomies also have enhanced specificity in ICD-10-PCS coding, which allows for defining a specific subset of patients (e.g., for research purposes) using 20 of the most clinically plausible ICD-10-PCS codes (Table 4). Notably, both the “excision” and “resection” “Operation” designations are valid for an esophagectomy. Use of the “bypass” “Operation” indicator of “1” would not adequately describe an esophagectomy on its own, but it would describe the reconstruction or anastomosis portion of the esophagectomy procedure (just as a “drainage” operation root would apply to esophagostomy). However, depending on the context, both a code for esophagectomy and a code for reconstruction or diversion may be necessary to define circumstances of esophagectomy.
Full table
The “Approach” designation becomes important in distinguishing thoracoscopic versus open techniques. A “percutaneous endoscopic” approach is used to code for thoracoscopic and laparoscopic techniques. There is presently no method to differentiate between a video-assisted versus a robotic-assisted thoracoscopic surgery utilizing ICD-10-PCS, as the “Approach” designation of “percutaneous endoscopic” is employed for both procedure types with no further differentiation available within the “Device” or “Qualifier” designations. Of note, bronchoscopy, including endobronchial ultrasound, and esophagogastroduodenoscopy (EGD) procedures are coded as “via a natural or artificial opening endoscopic” (though there is no additional “Device” or “Qualifier” designations to account for use of ultrasound during an EGD). Mediastinoscopy is coded as a percutaneous endoscopic approach, although it is important to note that mediastinoscopy falls under the “Anatomic Regions, General” “Body System” coded as “0W.” Official guidelines instruct coders that, if an intended procedure is discontinued, they should code the procedure to the root operation performed. This practice will allow researchers to utilize this “Approach” designation to evaluate questions such as which patients undergo intraoperative conversion from thoracoscopic approach to a thoracotomy by sampling for patients with both procedure codes (e.g., combination of a “percutaneous endoscopic” “inspection” code along with an “open” “resection” code). Thus, the significant detail enwrapped in each procedure code is potentially beneficial to researchers investigating specific topics.
Challenges of ICD-10-CM/PCS
With the 10th revision of ICD come a number of new challenges in both billing and utilization of administrative datasets for outcomes research. While ICD-10-PCS will be highly pertinent for clinicians analyzing surgical outcomes, these coding data will often need to be paired with ICD-10-CM diagnosis data because of the lack of disease-specific information in the new procedural codes. ICD-10-PCS procedure codes are agnostic to the underlying disease process associated with the procedure. A thoracotomy can be performed for a myriad of reasons such as diagnosis, therapy for a benign process, therapy for a cancer process or palliation. It therefore becomes vital to use more involved logic based on the ICD-10-CM diagnosis codes when a specific patient cohort is desired, such as those undergoing therapeutic lobectomy for lung cancer. Unfortunately, the ICD-10-CM codes for neoplasms are non-specific for cancer staging information or histology, so users will have to obtain more detailed oncologic characteristics from other data sources.
The ICD-10-PCS “Operation” character is vital to selecting the correct procedure codes, and prospective researchers should be familiar with the definitions of the 31 root operations. Of particular importance is the definition of “excision,” which refers to partial removal of a body part, as opposed to “resection,” which involves the complete removal of a body part. The definition of a complete body part is variable depending on the relevant anatomy. A pulmonary lobectomy of the right upper lobe is the removal of a complete right upper pulmonary lobe, and thus is a “resection” of a complete anatomical unit (Table 2). A segmentectomy of the right apical segment, though removing the entire segment, does not remove an entire body part as defined by the “Body Part” options within the Respiratory System chapter of ICD-10-PCS, and would thus constitute an “excision” (Table 3). A pulmonary wedge resection would also constitute an “excision,” and therefore cannot be differentiated from a segmentectomy. As such, researchers may need to define such surgical populations as patients undergoing sublobar resections without the specificity of a segmentectomy versus wedge resection. In comparison, ICD-9-CM offered procedure codes for “thoracoscopic segmental resection of the lung” (32.30) versus “other excision of lung” (32.90), “thoracoscopic lung biopsy” (33.20), “closed endoscopic biopsy of lung” (33.27), and “open biopsy of lung” (33.28), which might signify wedge resections. Additionally, one must be aware that ICD-10-PCS codes for “excision” under the “Body System” “Respiratory System” allow for a variety of “Approaches” including “percutaneous,” “via natural or artificial opening,” and “via natural or artificial opening endoscopic approaches.” These three “Approaches” are not consistent with how a sublobar resection would clinically be performed, but researchers should be aware of their existence to account for the possibility of miscoding by coders.
There is some ambiguity in the coding of bilobectomy, as a coder might apply two codes with the “resection” “Operation” character to describe the two individual lobes that were resected. Alternatively, a coder could conceivably use a code under the “excision” “Operation” character such as 0BBK0ZZ (excision of the right lung via an open approach) to describe removal of less than the total right lung as a representation of a bilobectomy. Additionally, as previously discussed there is some ambiguity in the coding of a sleeve lobectomy which could lead to coder error in accurately defining the operation. While clinically it would be most logical to pair a lobectomy “resection” code with the appropriate bronchus “resection” code, one could conceivably utilize a bronchus “excision” code as well. It is also unclear what a bronchus “resection” would consist of without pairing the code with the appropriate lobectomy “resection” because a lobar bronchus “resection” by its nature has to include the pulmonary parenchyma associated with the bronchus.
A thoracic lymph node biopsy via mediastinoscopy should commonly be coded as an excision (07B74ZX) when individual lymph nodes from specific lymph node stations are sampled (12). As such, the potential assemblage of procedure codes needed to capture all patients undergoing a specific procedure quickly becomes large and complex. While coders are instructed by the Official Guidelines for Coding and Reporting to apply the correct root “Operation” character regardless of how the operating physician words the procedure in their documentation, there is certainly room for ambiguity and unintentional miscoding, which could affect accurate sampling of patient cohorts for research (11). An institution might incorrectly code their lobectomies as an “excision” of a lung rather than a “resection” of a lung lobe, leading to under-selection of available patients for a research cohort.
The complexity of the “Operation” characteristic is exemplified in the potential codes required to capture all possible instances of an esophagectomy (Table 4). It is not clear which “Operation” codes are most correct in defining an esophagectomy. An esophagectomy involving the lower third of the esophagus might correctly be coded as a “resection” when the entire lower third of the esophagus is removed, whereas it might be more accurate to code as an “excision” when less than the entirety of the lower third of the esophagus is removed. Coding an esophagectomy as an “excision” then clouds the distinction between esophagectomy and excisional biopsy, unless the diagnostic “Qualifier” is appropriately applied. A third “Operation” characteristic that appears to accurately describe portions of an esophagectomy operation is the “bypass” operation. While this “Operation” appears to add some detail in describing the altered route of passage of the contents of a tubular body part, the Official Guidelines for Coding and Reporting part B3.1b state that components of a procedure (such as anastomosis of a tubular body part) that are a part of the root operation definition (such as resection of a tubular body part) are not coded separately (11). The resulting interpretation—which we believe is problematic—is that an esophagectomy implies that an anastomosis was also performed, thus making a “bypass” code redundant and unnecessary. However, an esophagectomy could be performed with reanastomosis, creation of a cervical esophagostomy, or leaving a portion of the esophagus in situ as a blind pouch. In such situations, the ambiguity of the “resection” “Operation” alone seems to require further specification by an additional “bypass” or “drainage” code. The “bypass” “Operation” adds some limited additional information regarding the nature of the bypass conduit. The “Body Part” characteristic specifies the body part bypassed from, while the “Qualifier” in bypass coding refers specifically to the distal body part that is being bypassed to. As such, a direct esophagojejunal anastomosis (0D150ZA) is definable when a total gastrectomy with partial esophagectomy is required, using the proximal “Body Part” of esophagus and the distal “Qualifier” of jejunum. A cervical esophagostomy (0D110Z4) is definable using the “Esophagus, Upper” as the proximal and “Cutaneous” as the distal sites of the “bypass.” Use of the “Device” characteristic allows for differentiation between an esophagectomy with a gastric conduit (0D150Z6) using “No Device” as compared to a colonic interposition or jejunal interposition bypass conduit (0D15076) using “Autologous Tissue Substitute” for the “Device.” Unfortunately, there does not appear to be a way to distinguish between a colonic or jejunal interposition bypass conduit. Such detail was definable in the ICD-9-CM Volume 3 with codes for “intrathoracic esophago-esophagostomy,” “intrathoracic esophagogastrostomy,” “intrathoracic esophageal anastomosis with interposition of small bowel,” or “intrathoracic esophageal anastomosis with interposition of colon,” in addition to “antesternal” codes for all of the above procedures. Thus significant anatomic detail has been removed from ICD-10-PCS. In any case, many ICD-10-PCS codes remain and must be employed to capture all appropriate subjects in any analysis evaluating esophagectomy patients (Table 4).
While an open versus minimally invasive esophagectomy can be differentiated based on the “Approach,” there is no reliable way—even with all the complexity of ICD-10-PCS—to differentiate between common esophagectomy techniques such as transhiatal, McKeown 3-hole, Ivor Lewis, or thoracoabdominal esophagectomy, although some procedure categorization may be inferred based on the use of thoracotomy and location of the anastomosis, i.e., cervical or intrathoracic. Eponyms are generally not permitted in ICD-10-PCS; coding guidelines encourage the use of a combination of codes to describe all of the relevant components of a complex procedure. As a result, strategies for patient population selection from administrative datasets using ICD-10-PCS may require specific combinations of multiple codes (e.g., at least one from List A and at least one from List B). To select reproducible patient cohorts without selection bias, users should account for the numerous coding possibilities present in ICD-10-CM/PCS. Accurate descriptions of the data selection method to create a patient cohort from population based administrative datasets should be included in the Methods section of any such studies. In fact, the REporting of studies Conducted using Observational Routinely-collected Data (RECORD) group collaborative guidelines recommends documentation as such: “RECORD 6.1: The methods of study population selection (such as codes or algorithms used to identify subjects) should be listed in detail. If this is not possible, an explanation should be provided. RECORD 6.2: Any validation studies of the codes or algorithms used to select the population should be referenced. If validation was conducted for this study and not published elsewhere, detailed methods and results should be provided” (13).
Finally, one must be aware that the detail inherent in ICD-10-PCS can lead to coding of some procedures that are impractical or implausible. Some examples of such unrealistic or unlikely procedures include percutaneous endoscopic resection of the lungs (bilateral), percutaneous fragmentation of the carina, endoscopic resection of the entire esophagus and endoscopic bypass from the upper esophagus to the ileum with a synthetic substitute. While these possibilities have little or no clinical use, they exist in ICD-10-PCS and therefore could inadvertently be selected by a misinformed coder. Such procedures of dubious merit could be pruned from the coding classification through the ICD-10-CM/PCS Coordination and Maintenance Committee, but until that time researchers must consider the possibility of miscoding of procedures that are of actual interest.
Conclusions
ICD-10-CM/PCS is a robust tool for the clinical researcher aiming to harness the power of large administrative datasets. It is vitally important that coders work in conjunction with surgeons to ensure that correct and optimized codes are consistently used for specific procedures. Additionally, a keen understanding of the workings of the coding system is necessary to employ it as a patient selection tool for large population datasets in a logical manner. There are many potential missteps to navigate, and it is therefore vitally important for researchers and journal editors alike to understand and agree upon research methods that are accurate and coherent when utilizing ICD-10-CM/PCS diagnosis and procedure codes. This article proposes some of the procedure codes that may be relevant in defining a population of thoracic surgery patients, but future work will need to establish and validate additional good practices for the application of this coding system to thoracic surgical clinical research efforts.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- World Health Organization. History of the development of the ICD [Internet]. WHO. 2018 [cited 2018 Aug 24]. Available online: http://www.who.int/classifications/icd/en/HistoryOfICD.pdf
- Plummer AL. International Classification of Diseases, Tenth Revision, Clinical Modification for the Pulmonary, Critical Care, and Sleep Physician. Chest 2015;148:1353-60. [Crossref] [PubMed]
- Utter GH, Cox GL, Owens PL, et al. Challenges and opportunities with ICD-10-CM/PCS: implications for surgical research involving administrative data. J Am Coll Surg 2013;217:516-26. [Crossref] [PubMed]
- Launer H, Nguyen DV, Cooke DT. National perioperative outcomes of pulmonary lobectomy for cancer in the obese patient: a propensity score matched analysis. J Thorac Cardiovasc Surg 2013;145:1312-8. [Crossref] [PubMed]
- Cooke DT, Nguyen DV, Yang Y, et al. Survival comparison of adenosquamous, squamous cell, and adenocarcinoma of the lung after lobectomy. Ann Thorac Surg 2010;90:943-8. [Crossref] [PubMed]
- Zheng DJ, Cooke DT. A survival comparison of mucin-producing adenocarcinoma of the esophagus to conventional adenocarcinoma after esophagectomy. Am Surg 2013;79:49-53. [PubMed]
- David G, Gunnarsson CL, Moore M, et al. Surgeons' volume-outcome relationship for lobectomies and wedge resections for cancer using video-assisted thoracoscopic techniques. Minim Invasive Surg 2012;2012:760292. [Crossref] [PubMed]
- Blasberg JD, Seder CW, Leverson G, et al. Video-Assisted Thoracoscopic Lobectomy for Lung Cancer: Current Practice Patterns and Predictors of Adoption. Ann Thorac Surg 2016;102:1854-62. [Crossref] [PubMed]
- Oh DS, Reddy RM, Gorrepati ML, et al. Robotic-Assisted, Video-Assisted Thoracoscopic and Open Lobectomy: Propensity-Matched Analysis of Recent Premier Data. Ann Thorac Surg 2017;104:1733-40. [Crossref] [PubMed]
- Centers for Medicare and Medicaid Services. ICD-10-CM Official Guidelines for Coding and Reporting [Internet]. 2018 [cited 2018 Aug 27]. Available online: https://www.cms.gov/Medicare/Coding/ICD10/Downloads/2018-ICD-10-CM-Coding-Guidelines.pdf
- Centers for Medicare and Medicaid Services. ICD-10-PCS Official Guidelines for Coding and Reporting [Internet]. 2018 [cited 2018 Aug 27]. Available online: https://www.cms.gov/Medicare/Coding/ICD10/Downloads/2017-Official-ICD-10-PCS-Coding-Guidelines.pdf
- Lymph Node Sampling. AHA Coding Clin ICD-10-CM PCS, 3Q 2014. 2014;1:9–11.
- Benchimol EI, Smeeth L, Guttmann A, et al. The REporting of studies Conducted using Observational Routinely-collected health Data (RECORD) statement. PLoS Med 2015;12:e1001885. [Crossref] [PubMed]


