
Perioperative change in neutrophil-to-lymphocyte ratio (NLR) is a prognostic factor in patients with completely resected primary pulmonary sarcomatoid carcinoma
Introduction
Inflammation is known to increase the risk of many types of cancers (including bladder, cervical, gastric, intestinal, esophageal, ovarian, prostate and thyroid cancer) through oncogenic mutations, angiogenesis, and change in the tumor microenvironment (1). Neutrophils, as a key inflammatory cell type, are known to progress tumor by upregulating inducible NO synthase (iNOS) which results in increased release of reactive oxygen species that directly damages DNA. Neutrophils are also known to play an important role in tumor angiogenesis by expressing vascular endothelial growth factor (VEGF) and releasing matrix metalloproteinase-9 (MMP-9) which have been shown to have the most profound effects in mediating tumor angiogenesis (2). Many recent reports have revealed that serum neutrophil-to-lymphocyte ratio (NLR) is related to the prognosis of various type of cancers from multiple organs (3-13). Many studies have demonstrated a relationship between the initial preoperative NLR and prognosis in patients with various type of cancers including NSCLC, and some of the more recent studies demonstrated prognostic significance of postoperative NLR and change in NLR in gastric cancer and non-small cell lung cancer (NSCLC) as well, emphasizing the prognostic significance of the dynamic change in the NLR after the treatment (3-12).
Primary pulmonary sarcomatoid carcinoma (PSC) is a rare variety of tumors which is included in NSCLC category with its incidence reported to vary from 0.1% to 4.1% (14). Previous reports have shown poorer prognosis after surgical resection than other types of NSCLCs with prognostic factors such as complete resection, lymph node (LN) metastasis (14-18). Primary PSC is also known to be refractory to conventional chemotherapy and radiotherapy with higher possibility of earlier metastases (19). Therefore, we tried to investigate the effect of immunologic factor on this rare type of cancer. Because of its rare incidence, the actual prognosis and its risk factors of completely resected primary sarcomatoid carcinoma is not well known. We performed this study to evaluate if there is prognostic significance between perioperative change in NLR and survival in patients with completely resected primary PSC.
Methods
This study was approved by the Institutional Review Board of our institution (IRB Number: B-1809-495-111, Seoul National University Bundang Hospital). From October 2003 to September 2015, a total of 50 patients underwent surgical resection for primary PSC at our institution. After excluding incompletely resected cases, pM0 and patients who had any history of another type of cancer, a total of 37 patients were included in the analysis. Clinical and pathological data of the patients were retrospectively retrieved from our prospectively collected lung cancer database and from our electronic medical record system. The preoperative evaluation included a detailed clinical history of the patient and physical examination, complete blood count (CBC) and blood chemistry analysis, bronchoscopy, computed tomography (CT) scan of the chest and upper abdomen, positive-emission tomography (PET) scan of the whole torso, brain magnetic resonance imaging (MRI), and pulmonary function tests. If lymph nodal metastasis was suspicious from the imaging studies, transbronchial needle biopsy with an endobronchial ultrasound (EBUS) was performed. The histologic diagnosis of the primary sarcomatoid carcinoma was made according to the 8th edition of the American Joint Committee on Cancer (AJCC) staging system. Every patient underwent an anatomical resection (at least segmentectomy) of the cancer. Surgery of the patients was performed by thoracotomy or video-assisted thoracoscopic surgery (VATS) under general anesthesia. All the patients were regularly followed up at the outpatient department. The initial neutrophil-to-lymphocyte ratio (iNLR) was calculated from the CBC which was obtained within 1 week before the surgery, and the postoperative NLR (pNLR) was obtained from the immediate postoperative CBC. iNLR subtracted from pNLR (pNLR-iNLR) was defined as change in NLR (ΔNLR).
Statistical analysis
Statistical analysis was performed using the SPSS for Windows, version 20.0 (IBM Corporation, Armonk, NY, USA) and R 2.13.0 (The R foundation). Maximally selected chi-square test was used for estimating the cutoff point number. Chi-square test, Student’s t-test, and log-rank test were used for the univariate analysis of the variables. Kaplan-Meier survival curve was used for estimating the overall survival and disease-free survival. Cox regression model was used for the multivariate analysis of the overall survival and disease-free survival.
Results
Patient characteristics and clinicopathologic results
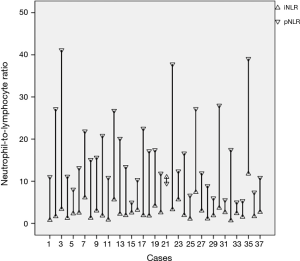
The mean age of the overall cohort was 62.2±1.9 years. Thirty-one patients (83.8%) were male. The mean size of the primary tumor and mean maximum standardized uptake value (SUV) from PET-CT was 4.5±0.3 cm and 10.4±0.9, respectively. Twelve patients (32.4%) underwent surgery by VATS. Only one patient (2.7%) underwent segmentectomy, the others underwent lobectomy (75.7%), bilobectomy (10.8%), or pneumonectomy (10.8%). Five (13.5%) patients revealed to be stage pT1 and among these pT1 patients, there was no case of pT1a, but only pT1b and pT1c. Mean number of dissected LNs was 20.6±1.9, and 20 patients (54.1%), 9 patients (24.3%), and 7 patients (18.9%) were staged as pN0, pN1, and pN2 respectively. A total of 25 patients (67.5%) underwent adjuvant chemotherapy. Seven patients (18.9%) revealed mixed cell types, and 25 patients (67.6%) revealed pure sarcomatoid carcinoma. The preoperative and postoperative NLR for each case of the patients are depicted in Figure 1. The mean value of the iNLR and ΔNLR were 3.1±0.4 and 13.0±1.4, respectively. Median follow-up duration was 4.62 years. During this follow-up period, a total of 17 patients (45.9%) had recurrences. Two patients (5.4%) had only locoregional recurrences, 8 patients (21.6%) had only distant recurrences, and 7 patients (18.9%) had locoregional and distant recurrences together. Among the 17 recurred patients, 7 patients (41.2%) recurred within 0.5 years after the surgical resection.
Analysis of the NLR
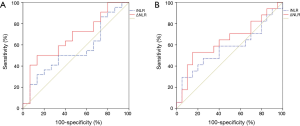
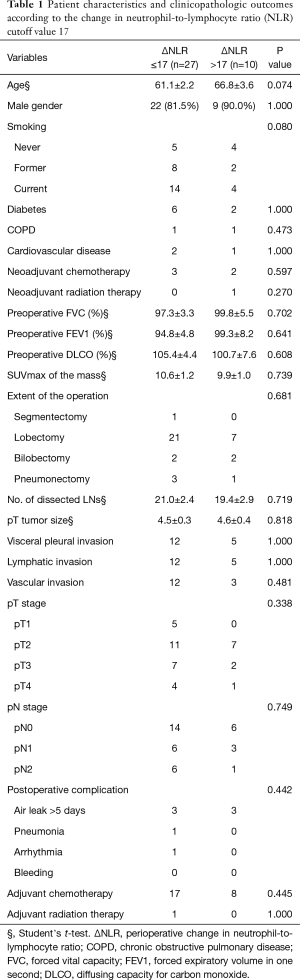
We used the receiver operating characteristics (ROC) curve to analyze the effect of the iNLR and ΔNLR on the overall survival and recurrence (Figure 2). The sensitivity and specificity of iNLR for overall survival were 50.0% and 60.0% with the area under the curve (AUC) 55.2%, and the sensitivity and specificity of ΔNLR for overall survival were 63.6% and 60.0% with the AUC 67.3%. The sensitivity and specificity of iNLR for recurrence were 58.8% and 60.0% with the AUC 55.2%, and the sensitivity and specificity of ΔNLR for recurrence were 64.7% and 60.0% with the AUC 64.4%, respectively. From these results showing the better profile of ΔNLR over iNLR, we decided to estimate the cutoff point of the ΔNLR for the overall survival. We performed the maximally selected chi-square test by downloading and using the maxstat package in R statistics which is freely downloadable (https://www.r-project.org), then the cutoff point of ΔNLR revealed to be 17 (20). We divided the 37 patients into two groups—the patients with ΔNLR ≤17 (n=27) and the patients with ΔNLR >17 (n=10). The 5-year overall survival rate was significantly poorer in the ΔNLR >17 group than in ΔNLR ≤17 group (10.0% vs. 66.1%, P=0.005). There was no significant difference in the patients’ characteristics and the other clinicopathologic results between the two groups (Table 1).
Full table
Survival analysis
Median overall survival of the whole cohort was 5.69 years and the median disease-free survival was 3.15 years. The 5-year overall survival rate (5-YSR) and 5-year disease-free survival rate for the whole cohort was 50.3% and 45.2%, respectively. When comparing the two groups by ΔNLR, the group with ΔNLR >17 showed significantly poorer 5-year overall survival rate than the group with ΔNLR 17 or less (10.0% vs. 66.1%, P=0.005), and poorer 5-year disease survival as well (10.0% vs. 60.4%, P=0.018) (Figure 3).
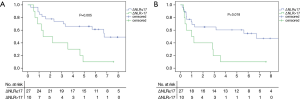
Univariate analysis of the overall survival by the log-rank test revealed age more than 70 years (P=0.009) and ΔNLR >17 (P=0.005) to be the risk factors. Higher iNLR (2 or less vs. >2, P=0.794), higher pathologic T stage (pT1–2 vs. pT3–4, P=0.416), lymphatic invasion (P=0.509), vascular invasion (P=0.813), presence of LN metastasis (P=0.744), and pure or mixed cell type (P=0.655) revealed no significant effect on overall survival. Neither neoadjuvant nor adjuvant chemotherapy had a significant effect on overall survival (P=0.442 and 0.662, respectively) as well. Age more than 70 years and ΔNLR >17 were also the risk factors for disease-free survival from the univariate analysis (P=0.036 and P=0.018 respectively). Multivariate Cox regression analysis revealed age >70 and ΔNLR >17 to be independent risk factors for the overall survival, and ΔNLR >17 to be the only independent risk factor for the disease-free survival (Table 2). This cut-off value 17 is just a value calculated only from our data which is not externally validated.
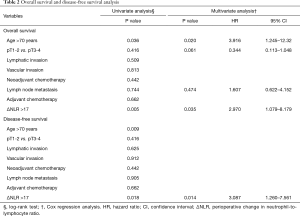
Full table
Discussion
Our data demonstrate the long-term clinical outcomes after complete resection of the pM0 primary PSC with the change in neutrophil-to-lymphocyte ratio as a significant prognostic factor. Fishback et al. reported in the year 1994 about 76 cases of pleomorphic sarcoma with a poor median survival of 0.83 years, but this study included who are not surgical candidates, and 12% of stage IV disease (21). Chang et al. reported a similar smaller series of 16 cases (7 underwent surgery) with a median survival of 0.25 years (22). Raveglia et al. reported in the year 2004 about 20 patients who all underwent surgical resection, and the patient all turned out to be pM0. The median overall survival was 0.67 years with early relapse of the disease, and the clinical outcomes seemed pessimistic even after surgery and adjuvant chemotherapy due to this early relapse (15). Park et al. reported in 2011 about outcomes after curative resection for sarcomatoid carcinoma of the lung with 5-YSR of 54.3%. In their series 43 patients (43.4%) had recurrence and 77.6% of the recurrences (33/43) were distant metastasis (23). Huang et al. reported in 2013 about 51 (37 patients underwent surgery) with a 5-YSR of 20.1%, and revealed tumor size and M stage as independent risk factors for prognosis (18). More recently, Okuda et al. reported in 2017 about 24 patients who had completely resected pM0 pulmonary pleomorphic carcinoma with 5-YSR of 54.7% and 5-year progression free survival 52.4%. They revealed vascular invasion and LN metastasis to be independent risk factors for overall survival (24). The survival data of our series is relatively favorable which is similar with those reported by Okuda et al., and which is relatively higher than previous studies. These relatively better survival outcomes may be attributable to excluding patients with a history of other malignancy and only including completely resected pM0 patients. There were only five patients (13.5%) who were diagnosed as pT1, which might be due to the aggressive behavior of the tumor. Our data also revealed 45.9% (17/35) of recurrence and most of the recurrence was distant recurrence (15/17, 94.6%) with 41.2% (7/17) recurring within 0.5 years, which is similar with the report from Yuki et al. and Park et al. (16,23). There has been controversy regarding prognostic factors─some studies reported tumor size, some studies reported complete resection, and some studies reported LN metastasis (14,16,17,21,24,25). However, data from our series revealed no significant relationship between prognosis and tumor size, pT stage, tumor composition (pure or mixed sarcomatoid), LN metastasis. Adjuvant chemotherapy had no prognostic significance on survival from our series, similar to reports from Lin et al. and Raveglia et al. (14,15).
Regarding the NLR, activated neutrophils can release matrix metalloproteinases (MMPs), especially MMP-9, which activates potent angiogenic factors (VEGF, fibroblast growth factor-2). On the other hand, lymphocytes act as a suppressor of cancer progression. Cytotoxic lymphocytes can kill tumor cells and are applicable for cancer immunotherapy (12). Tsubata et al. reported that VEGF expression was present in many cases of pulmonary pleomorphic carcinoma and a higher score of angiogenesis was significantly related to a poorer prognosis (26). The NLR is a readily available, inexpensive, and can be easily calculated and obtained from the database compared to other molecular markers. Earlier reports about NLR mostly focused on the significance of the initial (pretreatment) NLR. Khunger and colleagues reported the clinical significance of post-treatment NLR in 109 patients with NSCLC treated with nivolumab, which revealed that higher post-treatment NLR was related with poorer survival and non-respondence to the treatment (27). However, some of the recent papers are more focusing on the clinical significance of the change in NLR. Dan et al. reported the postoperative NLR change was an independent prognostic factor for patients undergoing radiofrequency ablation for small-sized hepatocellular carcinoma (28). Min et al. and Li et al. reported similar results for gastric cancer and colon cancer, respectively (12,29). Our data also revealed similar results, with ΔNLR being the independent prognostic factor for the overall survival and disease-free survival. We carefully suspect that more dynamically increased NLR after the surgery reflects higher neutrophil activity over lymphocyte activity after the surgery, which resulted in poorer survival. We measured postoperative NLR from immediate postoperative laboratory data to minimize the effect of postoperative infection or physical invasiveness from the surgery.
This study is a retrospective study with a small number of patients which can be the limitation. Further multicenter prospective study with a larger number of patients should be needed.
In conclusion, ΔNLR was significantly associated with poorer overall survival and disease-free survival in the patients with completely resected primary PSC and had better statistical significance than the initial preoperative NLR. The prognosis was poor in patients with higher ΔNLR, with the 5-year survival rate of 10.0% and the 5-year disease-free survival rate of 10.0%. More careful follow-up plan might be considered for patients with higher ΔNLR.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This study was approved by the Institutional Review Board of our institution (IRB Number: B-1809-495-111, Seoul National University Bundang Hospital).
References
- Mantovani A, Allavena P, Sica A, et al. Cancer-related inflammation. Nature 2008;454:436-44. [Crossref] [PubMed]
- Tazzyman S, Lewis CE, Murdoch C. Neutrophils: key mediators of tumour angiogenesis. Int J Exp Pathol 2009;90:222-31. [Crossref] [PubMed]
- An X, Ding PR, Li YH, et al. Elevated neutrophil to lymphocyte ratio predicts survival in advanced pancreatic cancer. Biomarkers 2010;15:516-22. [Crossref] [PubMed]
- Shimada H, Takiguchi N, Kainuma O, et al. High preoperative neutrophil-lymphocyte ratio predicts poor survival in patients with gastric cancer. Gastric Cancer 2010;13:170-6. [Crossref] [PubMed]
- Azab B, Bhatt VR, Phookan J, et al. Usefulness of the neutrophil-to-lymphocyte ratio in predicting short- and long-term mortality in breast cancer patients. Ann Surg Oncol 2012;19:217-24. [Crossref] [PubMed]
- Ohno Y, Nakashima J, Ohori M, et al. Followup of neutrophil-to-lymphocyte ratio and recurrence of clear cell renal cell carcinoma. J Urol 2012;187:411-7. [Crossref] [PubMed]
- Jin H, Zhang G, Liu X, et al. Blood neutrophil-lymphocyte ratio predicts survival for stages III-IV gastric cancer treated with neoadjuvant chemotherapy. World J Surg Oncol 2013;11:112. [Crossref] [PubMed]
- Zhao QT, Yang Y, Xu S, et al. Prognostic role of neutrophil to lymphocyte ratio in lung cancers: a meta-analysis including 7,054 patients. Onco Targets Ther 2015;8:2731-8. [PubMed]
- Jin F, Han A, Shi F, et al. The postoperative neutrophil-to-lymphocyte ratio and changes in this ratio predict survival after the complete resection of stage I non-small cell lung cancer. Onco Targets Ther 2016;9:6529-37. [Crossref] [PubMed]
- Kang M, Jeong CW, Kwak C, et al. The Prognostic Significance of the Early Postoperative Neutrophil-to-Lymphocyte Ratio in Patients with Urothelial Carcinoma of the Bladder Undergoing Radical Cystectomy. Ann Surg Oncol 2016;23:335-42. [Crossref] [PubMed]
- Lino-Silva LS, Salcedo-Hernandez RA, Garcia-Perez L, et al. Basal neutrophil-to-lymphocyte ratio is associated with overall survival in melanoma. Melanoma Res 2017;27:140-4. [Crossref] [PubMed]
- Min KW, Kwon MJ, Kim DH, et al. Persistent elevation of postoperative neutrophil-to-lymphocyte ratio: A better predictor of survival in gastric cancer than elevated preoperative neutrophil-to-lymphocyte ratio. Sci Rep 2017;7:13967. [Crossref] [PubMed]
- Ma J, Kuzman J, Ray A, et al. Neutrophil-to-lymphocyte Ratio (NLR) as a predictor for recurrence in patients with stage III melanoma. Sci Rep 2018;8:4044. [Crossref] [PubMed]
- Lin Y, Yang H, Cai Q, et al. Characteristics and Prognostic Analysis of 69 Patients With Pulmonary Sarcomatoid Carcinoma. Am J Clin Oncol 2016;39:215-22. [Crossref] [PubMed]
- Raveglia F, Mezzetti M, Panigalli T, et al. Personal experience in surgical management of pulmonary pleomorphic carcinoma. Ann Thorac Surg 2004;78:1742-7. [Crossref] [PubMed]
- Yuki T, Sakuma T, Ohbayashi C, et al. Pleomorphic carcinoma of the lung: a surgical outcome. J Thorac Cardiovasc Surg 2007;134:399-404. [Crossref] [PubMed]
- Avila Martinez RJ, Marron Fernandez C, Hermoso Alarza F, et al. Primary pulmonary sarcomatoid carcinomas. Arch Bronconeumol 2013;49:405-7. [PubMed]
- Huang SY, Shen SJ, Li XY. Pulmonary sarcomatoid carcinoma: a clinicopathologic study and prognostic analysis of 51 cases. World J Surg Oncol 2013;11:252. [Crossref] [PubMed]
- Rajdev K, Siddiqui AH, Ibrahim U, et al. Sarcomatoid Carcinoma of the Lung Presenting as Localized Bronchiectasis: A Case Report and Review of Literature. Respir Med Case Rep 2018;24:143-6. [Crossref] [PubMed]
- Boulesteix AL. Maximally selected chi-square statistics for ordinal variables. Biom J 2006;48:451-62. [Crossref] [PubMed]
- Fishback NF, Travis WD, Moran CA, et al. Pleomorphic (spindle/giant cell) carcinoma of the lung. A clinicopathologic correlation of 78 cases. Cancer 1994;73:2936-45. [Crossref] [PubMed]
- Chang YL, Lee YC, Shih JY, et al. Pulmonary pleomorphic (spindle) cell carcinoma: peculiar clinicopathologic manifestations different from ordinary non-small cell carcinoma. Lung Cancer 2001;34:91-7. [Crossref] [PubMed]
- Park JS, Lee Y, Han J, et al. Clinicopathologic outcomes of curative resection for sarcomatoid carcinoma of the lung. Oncology 2011;81:206-13. [Crossref] [PubMed]
- Okuda K, Oda R, Suzuki A, et al. Clinicopathological factors influenced the prognosis of surgically resected pulmonary pleomorphic carcinoma. J Thorac Dis 2017;9:1295-302. [Crossref] [PubMed]
- Yamamoto S, Hamatake D, Ueno T, et al. Clinicopathological investigation of pulmonary pleomorphic carcinoma. Eur J Cardiothorac Surg 2007;32:873-6. [Crossref] [PubMed]
- Tsubata Y, Sutani A, Okimoto T, et al. Tumor angiogenesis in 75 cases of pleomorphic carcinoma of the lung. Anticancer Res 2012;32:3331-7. [PubMed]
- Khunger M, Patil PD, Khunger A, et al. Post-treatment changes in hematological parameters predict response to nivolumab monotherapy in non-small cell lung cancer patients. PLoS One 2018;13:e0197743. [Crossref] [PubMed]
- Dan J, Zhang Y, Peng Z, et al. Postoperative neutrophil-to-lymphocyte ratio change predicts survival of patients with small hepatocellular carcinoma undergoing radiofrequency ablation. PLoS One 2013;8:e58184. [Crossref] [PubMed]
- Li Z, Zhao R, Cui Y, et al. The dynamic change of neutrophil to lymphocyte ratio can predict clinical outcome in stage I-III colon cancer. Sci Rep 2018;8:9453. [Crossref] [PubMed]


