
The pattern of use and survival outcomes of a dedicated adult Home Ventilation and Respiratory Support Service in Singapore: a 7-year retrospective observational cohort study
Introduction
Home mechanical ventilation (HMV) is widely used in conditions associated with chronic ventilatory insufficiency such as amyotrophic lateral sclerosis (ALS), congenital muscular dystrophy and spinal cord injury (SCI) (1-4). It has been demonstrated to improve sleep-related symptoms, morbidity and mortality of the ventilator-assisted individuals (VAIs) (2,5,6).
The reported prevalence (per 100,000 population) of HMV use varies depending on countries and ranges from 6.6 in Europe to 12.9 in Canada (1,4,7,8). In South East Asia (SEA), the pattern of use is likely to differ according to available resource and local advocacy. The prevalence of HMV is not known but there is likely a growing demand for HMV support. A recent single-centre cohort study in Malaysia showed an increased use of HMV in children over the past decade (9).
In Singapore, the Home Ventilation and Respiratory Support Service (HVRSS) at Tan Tock Seng Hospital (TTSH) was set-up in 2009. The initial aim was to provide home care and support for individuals with cervical SCI who require long-term ventilation and would otherwise have remained in hospital. The service was later expanded to include care for individuals with advanced neuromuscular weakness and other causes of hypercapnic ventilatory failure. The multidisciplinary HVRSS comprises of doctors with special interest in HMV (anaesthetist, respiratory and family physicians), nurse clinicians, respiratory therapist and medical social workers.
HMV poses significant care and financial burden to affected individuals, family and the health system. There is increasing need to demonstrate the demand for such support, the clinical efficacy and outcomes to health authorities for appropriate allocation of resources and continuous funding support. To date, there has not been any prior publication on the use of similar service and survival outcomes in Singapore or in the SEA. We aim to describe the pattern of use of our service, examine the survival outcomes and identify important prognostic factors of our cohort.
Methods
The HVRSS recruitment criteria and service
The HVRSS is the only national adult multidisciplinary service in Singapore. We receive referrals from within the institution or externally. We assess all individuals whom the primary physician (usually neurologist or intensivist) think may benefit from HMV. The primary criteria for recruitment into the HVRSS include hypercapnic respiratory failure or progressive neuromuscular disease with respiratory or sleep-related symptoms. Other criteria include preserved ability to interact or communicate and patient’s consent. In addition, favourable social circumstances such as having at least a full-time carer and a discharge destination (preferably home) are essential as there are very limited facilities for long term institutionalised care in Singapore. Primary uncomplicated sleep disordered breathing (SDB) cases are excluded due to resource constraint and are looked after by individual doctors interested in sleep medicine.
The HVRSS receives pilot funding from the Ministry of Health and all VAIs are subjected to means testing to determine the eligibility and proportion of funding assistance for equipment purchase. Routinely, ambulatory VAIs are followed up every 3–6 monthly at the outpatient clinic. Non-ambulatory VAIs or those receiving invasive mechanical ventilation (IMV) are reviewed every 2 months (and have tracheostomy changed at home). Phone consult service is available during office hours and ad hoc home visits can be arranged where necessary. Where appropriate, the HVRSS prescribes and titrates mechanical ventilation and mechanical insufflation-exsufflation (MIE) devices and provides caregiver training (including basic ventilator troubleshoot, emergency tracheostomy care, feeding instruction etc.) to facilitate transition to home. HVRSS also provides care coordination with various other allied health services including physiotherapy, occupational therapy and nutritionist. In addition, all referrals receive emotional support by our medical social workers and the service collaborates closely with palliative care services to provide end-of-life support.
Study design
We conducted a retrospective observational cohort study. All individuals who were referred for consideration of HMV over a 7-year period from 1/1/2009 to 31/12/2015 were identified. The individuals who required and accepted long term HMV were included for analysis. HMV was defined as mechanical ventilation, administered non-invasively or invasively (via tracheostomy), at home or in long term residential care.
Data collection
Electronic medical record review was carried out. We collected baseline demographics and social data such as age, gender, ethnicity, type and distance of residence to our centre, marital status, per capita household income and number and type of carer(s). The primary indications for HMV, smoking status, important comorbidities (diabetes mellitus, hypertension, hyperlipidaemia, congestive cardiac failure, ischaemic heart disease, malignant disease, stroke and airway diseases) and baseline physiology including spirometry and blood gas results were also recorded. In addition, we obtained data on HMV prescription details (e.g., interface, setting and adherence), use of supplemental oxygen and percutaneous gastroenterostomy nutrition.
Survival was determined from the date of HMV initiation to the date of death or 1/09/2017, whichever occurred earlier. The date and cause of death were determined from hospital-maintained records.
Disease categories
For descriptive analysis, the cohort was divided into 4 clinical categories based on expected natural progression of illness and care requirement: (I) ALS; (II) other neuromuscular and chest wall diseases (NMCW); (III) SCI; and (IV) complex intensive care unit (ICU). Complex ICU group is a subset of VAIs that were mainly receiving prolonged mechanical ventilation or failure-to-wean with no prospect of leaving the monitored care area.
For the analysis of prognostic factors, due to different trajectory of illness and to improve statistical power, we considered ALS and all non-ALS VAIs separately.
Statistical analysis
Continuous data was described using median [interquartile range (IQR)] or mean (standard deviation) where appropriate. Categorical data was described using proportion or percentage. Survival estimates were displayed using Kaplan-Meier survival curves and compared by log-rank test. To study the factors influencing survival, demographic, physical and ventilator setting variables were dichotomised when possible using clinically meaningful cut offs. Cox proportional analysis was used to determine hazard ratio (HR) and 95% confidence interval (CI) of these factors. Predictive factors with P values of <0.10 on univariate analysis (along with age and gender) were further examined in a forward stepwise analysis with removal and entry P values of 0.10 and 0.05 and significant predictors with P values <0.05 were reported. Statistical analysis was performed using STATA 14.2 software (StataCorp, Texas, USA). Statistical significance was taken at P value <0.05.
Ethics
Ethical approval was granted by the National Healthcare Group Domain Specific Review Board (reference no 2017/00471).
Results
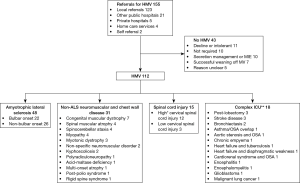
The referrals for HMV increased exponentially year-on-year since the service started (Figure 1). A total of 155 individuals were referred; most of these were local referrals from the TTSH ICU and adjacent National Neuroscience Institute. A smaller proportion were referrals from other institutions, private hospitals or self-referrals.

There were 112 individuals who proceeded to HMV; most (68%) VAIs were decided for HMV during an acute hospital admission and two thirds of these were recruited in the ICU. Main diagnoses were ALS, congenital myopathy and SCI. The study flow and detailed diagnoses of the VAIs are illustrated in Figure 2.
Baseline demographics and physical characteristics
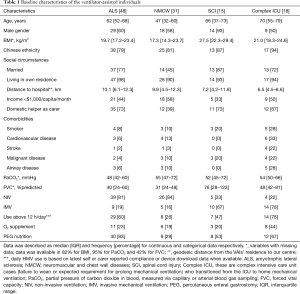
The median age of the VAIs ranged from 47–70 years and body mass index ranged from 17.3–27.5 kg/m2 across the groups. There was male gender predominance (50–93%). Among all the VAIs, almost all (95%) lived within 15 km from our centre and in their own home. The VAIs had at least one full-time carer [70% were hired foreign domestic helpers (FDH) from nearby countries] and were mostly ethnic Chinese (83%) and married (69%). Just under half (47% VAIs) had monthly per capita household income of <$1,000/month (an entry criterion for financial assistance in our centre).
Co-morbidities such as cardiovascular disease, malignant disease, stroke and airway diseases were common, especially in the complex ICU group. At the initiation of HMV, the VAIs had moderately severe ventilatory impairment. Median (IQR) FVC was 38 [24–65] %predicted and partial pressure of carbon dioxide (PaCO2) was 52 [45–66] mmHg for all VAIs.
Therapy prescription and usage
Seventy-four (66%) individuals were prescribed non-invasive ventilation (NIV). Fifteen VAIs subsequently transitioned to IMV. These VAIs were mainly suffering from ALS (n=9) and all were relatively young (<70 years of age). The transition from NIV to IMV was performed electively following extensive counselling of the potential complications including lock-in state. For the ALS VAIs on IMV at the outset, all were tracheostomised in the ICU prior to our involvement.
Most (67%) VAIs were supported with pressure-cycled ventilation; median (IQR) applied inspiratory, expiratory pressures and set-rate were 15 [12–18], 5 [4–6] cmH2O and 15 [12–16] breaths per minute respectively. Half of the VAIs reported daily HMV use of >12 hours. Twenty-eight (25%) VAIs received additional supplemental oxygen during HMV. Nutrition via gastrostomy was common (63% of VAIs). For the ALS group, 31 of the 48 VAIs were also prescribed MIE device for secretion management.
The baseline demographics, physiological characteristics, co-morbidities and therapy details of the VAIs are described in Table 1.
Full table
Follow up and survival outcomes
There were 64 deaths over a median (IQR) follow-up period of 2.56 (1.86–3.69) years. No cases were lost to follow-up. The median (95% CI) survival (in ascending order) were 1.8 (0.6–5.7), 2.6 (0.8–4.8), 4.2 (2.1–7.6) and 6.7 (4.5–10.7) years for ALS, complex ICU, SCI and NMCW groups respectively (Figure 3).
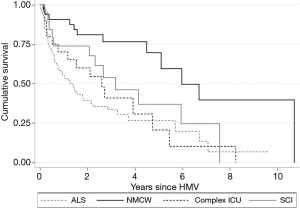
The three most common reported causes of death were death from primary disease (n=22), pneumonia (n=15) and sudden death (n=10) (data was available in 83% VAIs). Following further review of the unexpected deaths: 2 were presumed cardiac in nature (ventricular arrhythmias), 2 were likely due to aspiration, 1 was due to a fall and 5 were unknown, of which there was 1 case of possible ventilator malfunction.
Prognostic factors
In ALS group, Chinese ethnicity, NIV-transitioned-to-IMV and FVC >50%predicted were favourable prognostic factors with HR (95% CI) of 0.41 (0.18–0.95), 0.23 (0.07–0.78) and 0.24 (0.06–1.00) respectively. Poor prognostic factors were use of NIV interface only (HR 2.33, 95% CI: 1.06–5.11) and increased time between symptom onset and HMV initiation (HR 1.01, 95% CI: 1.00–1.02). Daily use of above 12 hours was associated with a trend towards worse survival (HR 1.94, 95% CI: 0.90–4.18). In multivariate analysis, NIV-transitioned-to-IMV (HR 0.24, 95% CI: 0.07–0.81) was the only independent factor associated with better survival (Table 2). Riluzole and enteral nutrition use were not significant prognostic factors.
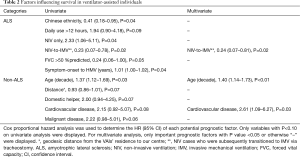
Full table
In non-ALS VAIs, older age (HR 1.37, 95% CI: 1.12–1.69 per decade increment) was associated with reduced survival. Factors that showed trend towards increased hazard of death were domestic helper as primary carer (HR 2.00, 95% CI: 0.94–4.25), co-morbid cardiovascular disease (HR 2.15, 95% CI: 0.92–5.07) and cancer diagnosis (HR 2.22, 95% CI: 0.98–5.01). Living distance further from hospital (HR 0.93, 95% CI: 0.86–1.01) was possibly associated with better survival outcome. In a multivariate model, older age (HR 1.40, 95% CI: 1.14–1.73) and cardiovascular disease (HR 2.61, 95% CI: 1.09–6.27) remained important negative prognostic factors (Table 2).
Subgroup without HMV
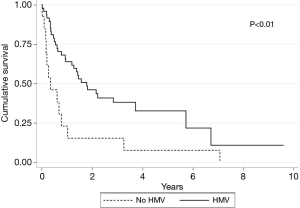
Forty-three individuals did not proceed to long term HMV. The reasons for no HMV are listed in Figure 2. Most of the individuals who declined or were not tolerant of NIV were ALS (n=9). Many individuals with spinal cord injuries were either successfully weaned off ventilator (n=7) or only required MIE (n=5). Comparing survival by log-rank analysis, in ALS, individuals who had a trial of NIV but decided not for HMV had significantly poorer survival (P<0.01) (Figure 4).
Discussion
To our knowledge, this is the first multi-ethnic Asian study on the use and survival outcome of HMV. We demonstrated that there is an increasing demand for a multidisciplinary home ventilation service to support VAIs with severe functional and physiological impairment. The baseline characteristics and survival varied according to disease categories. The worst survival was among the ALS group while the NMCW VAIs had the best survival. In ALS, transition from NIV to IMV were independently associated with better survival. Among the non-ALS VAIs, older age and those with cardiovascular disease had less favourable outcome.
The referrals to HVRSS had increased over the years. We think that this is due to increased awareness of HMV and the perceived better care by a dedicated service, which allows for pooling of expertise and resources. The NMCW group were the longest HMV users whereas many in the SCI group referred were eventually weaned from ventilatory support and did not require long term HMV. Our VAIs were generally middle-aged and older except for the NMCW group, similar to findings in other cohorts (10,11).
Almost half of the families were from lower income groups. There was heavy reliance on hired FDH for nursing care and support at home (in part due to limited access to professional skilled carers), this has contributed to additional financial burden. It is known that chronic illness is associated with poverty (12). Although selected by the VAIs (who would have considered language issue), FDH represent a challenge for caregiver training due to communication barrier and turnover where caregiver training needs to be repeated.
The survival of VAIs in our cohort is comparable to published studies (10,11,13). The poor survival in the ALS cohort was expected given the progressive nature of the illness. In our study, we demonstrated that the individuals who received HMV survived longer than those who did not, consistent with the trial result by Bourke et al. (14). However, the actual cohort of ALS without HMV is not fully captured as some individuals may have declined to see us. The median survival of SCI VAIs appears to be shorted when compared to study by Watt et al. (15). This may be explained by the relatively older age at injury in our cohort, which is factor associated with strong hazard of death (15).
The complex ICU group had very similar survival to ALS group, which reflects that these individuals had severely reduced physiologic reserve and multiple co-morbidities (including malignant disease). While some of these individuals may not be typically considered for HMV, in Singapore, societal view on filial piety along with complex healthcare financing (16) with government subsidy but also often a sizeable out-of-pocket cash and/or insurance pay out often negate a paternalistic approach. Ethically, we find it difficult to withdraw ventilator support in individuals who remain lucid (albeit minimally communicative in some) and expressed wish to continue living. Therefore, HMV became the only alternative to ICU stay; our involvement allowed selected individuals to spend time in their own home, provided they accepted the risks and took responsibility for their own care. Many chose to do so because of the perceived increased autonomy and quality of life (authors’ experience).
Approximately a third of the deaths in our study were certified due to primary disease, similar to a study from North America (4). This group is likely due to progressive ventilatory failure and with ‘expected’ deterioration and death occurred at home. Of note, sudden or unexpected death was common, this is an interesting finding and we opined that the VAIs and family should be counselled of this risk.
In ALS, Chinese ethnicity was associated with reduced hazard of death. Genetic polymorphism and different mutation may account for observed ethnicity difference in outcome (17). Chinese ethnicity had been shown to be associated with milder disease and may explain the difference in outcome when compared with other ethnicity groups (18,19). However, the effect was not seen on multivariate analysis. We did not see poor prognostic factors such as older age at presentation and lower BMI described previously (10,13,18). The effect of age on survival was probably confounded by the increased proportion of conversion of NIV to IMV among younger VAIs, which was an independent positive prognostic factor in our cohort and previously demonstrated in a large observational study in Denmark (13).
The ALS VAIs who had better lung function were associated with better outcomes, similar to previous study findings (10,20). On the other hand, delay between symptom onset and HMV initiation and higher dependence on HMV appeared to be associated with poorer survival on univariate analysis. Majority of the ALS VAIs had bulbar phenotype when they presented to our service, which suggested that HMV may have been initiated later than previous studies and may explain the lack of prognostic consequence of this phenotype (21).
In non-ALS cases, the reliance on domestic helper may be a marker of increased severity of illness and care need. The effect of age on survival is probably due to increased survival among young congenital muscular dystrophy and relatively increased co-morbidities in older individuals with more severe illnesses. This finding is consistent with previous studies (10,11). Cardiovascular diseases were associated with older age and were negative prognostic factors.
Limitations
Due to the retrospective nature of the study, there were missing data in few variables, especially in FVC. Spirometry is routinely ordered for all HVRSS new cases, but in our experience, many patients were unable to achieve acceptable and repeatable spirometry and in some cases, spirometry was impossible due to tracheostomy. Another limitation is that compliance data was self- or carer-reported as device download data was very limited and therefore prone to reporting bias. We also recognised that concomitant SDB is common among the VAIs, as demonstrated in published cohort (10). Although sleep-related symptom is one of the recruitment criteria, we do not routinely performed polysomnography due to lack of capacity to manage VAIs with complex care need in the laboratory and long wait time.
Nationally, HVRSS is the only adult service available for HMV support and therefore our study is reasonably representative for Singapore. However, our sample size is relatively small when compared to other published cohorts; important prognostic factors with smaller effect may not be apparent on multivariate analysis.
A further limitation of this study is that we did not collect data on patient and caregiver satisfaction. Quality of life appeared to be reasonable for the VAIs who suffer from relatively slow progressive neuromuscular disease based on a recent survey by co-authors (22) but this may not be generalisable to rapidly progressive disease such as ALS.
In conclusion, the HVRSS supports a heterogenous group of VAIs with varying baseline demographics, social set-up, physiological characteristics and choice of therapy. There is an exponential increase in utilisation of our service since its inception. Despite being a relatively new service, comparable survival outcomes can be achieved by our model of care. ALS had the worst survival whereas NMCW had the best outcomes with Complex ICU and SCI groups in between. The result of this study is important for healthcare resource planning and when counselling for HMV. Future direction would be to create a national registry for HMV use to allow for interval monitoring of service delivery and regular survey on patient experience.
Acknowledgements
The authors would like to express gratitude towards the Centre of Research and Innovation Office at TTSH for rendering advice on study design and statistical analysis, HVRSS team members (including but not exclusive to) Ms Janet Chua Pei Lu, Ms Anura Tamar Peters and Ms Tao Sun for their tireless service and Associate Professor John Arputhan Abisheganaden (Respiratory and Critical Care Medicine, Head of Department) and Associate Professor Thomas Lew Wing Kit (TTSH Chairman Medical Board) for the continuous support and success of the programme.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: Ethical approval was granted by the National Healthcare Group Domain Specific Review Board (reference no 2017/00471).
References
- Simonds AK. Home mechanical ventilation: An overview. Ann Am Thorac Soc 2016;13:2035-44. [Crossref] [PubMed]
- Bach JR, Ishikawa Y, Kim H. Prevention of pulmonary morbidity for patients with Duchenne muscular dystrophy. Chest 1997;112:1024-8. [Crossref] [PubMed]
- Martí S, Pallero M, Ferrer J, et al. Predictors of mortality in chest wall disease treated with noninvasive home mechanical ventilation. Respir Med 2010;104:1843-9. [Crossref] [PubMed]
- King AC. Long-Term Home Mechanical Ventilation in the United States. Respir Care 2012;57:921-30. [Crossref] [PubMed]
- Ellis ER, Grunstein RR, Chan S, et al. Noninvasive ventilatory support during sleep improves respiratory failure in kyphoscoliosis. Chest 1988;94:811-5. [Crossref] [PubMed]
- Berlowitz DJ, Howard ME, Fiore JF, et al. Identifying who will benefit from non-invasive ventilation in amyotrophic lateral sclerosis/motor neurone disease in a clinical Cohort. J Neurol Neurosurg Psychiatry 2016;87:280-6. [Crossref] [PubMed]
- Lloyd-Owen SJ, Donaldson GC, Ambrosino N, et al. Patterns of home mechanical ventilation use in Europe: results from the Eurovent survey. Eur Respir J 2005;25:1025-31. [Crossref] [PubMed]
- Chatwin M, Tan HL, Bush A, et al. Long Term Non-Invasive Ventilation in Children: Impact on Survival and Transition to Adult Care. PLoS One 2015;10:e0125839. [Crossref] [PubMed]
- Nathan AM, Loo HY, de Bruyne JA, et al. Thirteen years of invasive and noninvasive home ventilation for children in a developing country: A retrospective study. Pediatr Pulmonol 2017;52:500-7. [Crossref] [PubMed]
- Tan GP, McArdle N, Dhaliwal SS, et al. Patterns of use, survival and prognostic factors in patients receiving home mechanical ventilation in Western Australia: A single centre historical cohort study. Chron Respir Dis 2018;15:356-64. [Crossref] [PubMed]
- Laub M, Midgren B. Survival of patients on home mechanical ventilation: A nationwide prospective study. Respir Med 2007;101:1074-8. [Crossref] [PubMed]
- Walker C. Chronic illness and consumer inequality : the impact of health costs on people with chronic illnesses in rural and regional Australia. Aust Health Rev 2007;31:203-10. [Crossref] [PubMed]
- Dreyer P, Lorenzen CK, Schou L, et al. Survival in ALS with home mechanical ventilation non-invasively and invasively: A 15-year cohort study in west Denmark. Amyotroph Lateral Scler Frontotemporal Degener 2014;15:62-7. [Crossref] [PubMed]
- Bourke SC, Tomlinson M, Williams TL, et al. Effects of non-invasive ventilation on survival and quality of life in patients with amyotrophic lateral sclerosis: a randomised controlled trial. Lancet Neurol 2006;5:140-7. [Crossref] [PubMed]
- Watt JW, Wiredu E, Silva P, et al. Survival after short- or long-term ventilation after acute spinal cord injury: a single-centre 25-year retrospective study. Spinal Cord 2011;49:404-10. [Crossref] [PubMed]
- Ministry of Health. Singapore’s healthcare financing system [Internet]. Singapore: Ministry of Health. Available online: https://www.moh.gov.sg/docs/librariesprovider5/resources-statistics/educational-resources/3menglish_final.PDF
- Marangi G, Traynor BJ. Genetic causes of amyotrophic lateral sclerosis: New genetic analysis methodologies entailing new opportunities and challenges. Brain Res 2015;1607:75-93. [Crossref] [PubMed]
- Chen L, Zhang B, Chen R, et al. Natural history and clinical features of sporadic amyotrophic lateral sclerosis in China. J Neurol Neurosurg Psychiatry 2015;86:1075-81. [Crossref] [PubMed]
- Liu X, Yang L, Tang L, et al. DCTN1 gene analysis in Chinese patients with sporadic amyotrophic lateral sclerosis. PLoS One 2017;12:e0182572. [Crossref] [PubMed]
- Fallat RJ, Jewitt B, Bass M, et al. Spirometry in amyotrophic lateral sclerosis. Arch Neurol 1979;36:74-80. [Crossref] [PubMed]
- Calvo A, Moglia C, Lunetta C, et al. Factors predicting survival in ALS: a multicenter Italian study. J Neurol 2017;264:54-63. [Crossref] [PubMed]
- Wong WM, Tan AK, Koh GC. Health-related Quality of Life of Home Ventilated Patients (HoMe V) from a Tertiary Hospital in Singapore. Ann Acad Med Singapore 2017;46:399-403. [PubMed]


