
Simulation training for crises during venoarterial extracorporeal membrane oxygenation
Introduction
With advancement in medical technology, the use of extracorporeal membrane oxygenation (ECMO) for patients with refractory respiratory and cardiac failure has experienced a resurgence in the last decade. In particular, the global caseload and indications for the use of venoarterial (VA) ECMO is rapidly expanding. The spectrum of disease conditions suitable for VA ECMO ranges from cardiogenic shock due to myocardial infarction, fulminant myocarditis, and refractory ventricular arrhythmia, to the use of ECMO during resuscitation of patients with refractory cardiac arrest, i.e., “ECMO-cardiopulmonary resuscitation” (E-CPR) (1).
Despite frequent efforts to ensure the appropriateness and safety of ECMO delivery, it remains a high-risk clinical activity due to its intrinsic complexity and low volume nature (2). As a result, continuing education is essential to ensure the quality, efficiency, sustainability, and outcomes of an ECMO program (3).
Traditional ECMO education curricula and teaching modalities include reading materials, didactic lectures, water drills, and animal laboratory practice (4). These methods often focus on cognitive and technical knowledge, with little emphasis on behavioural skills. Simulation training in ECMO has gained popularity as a supplement to current training modalities by providing a standardized, controlled, safe, and confidential learning environment, and is particularly aligned to cover stressful clinical scenarios and complex topics.
In this article, we will describe the pre-requisites of an ECMO simulation program, followed by an in-depth discussion of simulation training for crises in VA ECMO.
Setup of a high-fidelity ECMO simulation program
A common misconception of simulation training is that it is a casual exercise where learners perform actions in a simulated medical environment followed by an informal discussion or a question and answer session. In reality, well-structured simulation training is stringently designed and backed by human learning theories. The most important learning theory is Kolb’s theory of experiential learning, which describes learning as a cyclic process of “concrete experience”, “reflection”, “abstract conceptualization”, and active experimentation (5). Learning starts off with experiencing an event (concrete experience), followed by self-reflection or reflection assisted by facilitator (reflection), after which a new insight of the experience is developed (abstract conceptualization). Finally, this new insight is applied to another situation (active experimentation) and another learning cycle begins.
There are several key components in simulation training. Firstly, the learning environment is set up to provide an immersive experience and to create contextual reality. Secondly, details in simulation scenarios are purposefully designed according to clearly pre-defined learning goals and objectives. Thirdly, debriefing, the post experience analytic process, should be facilitated by trained and experienced debriefers to achieve effective learning.
Simulation environment and equipment
The first step in ECMO simulation is to provide a contextual reality for the simulation activity. Standard simulation centres can usually stage the clinical settings where ECMO is commonly used, e.g., intensive care unit (ICU), operating theatre, and emergency room. Occasionally, special settings such as the cardiac catheterization laboratory may be more suited to achieve certain learning objectives in VA ECMO scenarios. In these situations, special arrangement and support from the relevant stakeholders or even the hospital administration may be necessary.
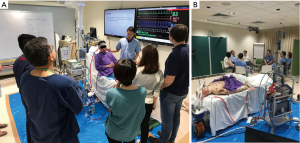
Equipment that is universal for ECMO simulation include an intubated manikin connected to a mechanical ventilator. Arterial lines, drug infusion devices, Foley catheters, and resuscitation equipment may be added as necessary. Essential physiological parameters, e.g., arterial blood pressure, pulse rate, ECG rhythm, oxygen saturation, and central venous pressure should be clearly displayed (Figure 1) and controlled remotely by a compatible computer program (e.g., Laerdal SimMan®). Additional clinical information such as laboratory results, chest radiographs, and echocardiography findings should be readily available upon request by the participants.
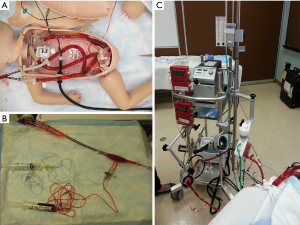
During ECMO simulation training, learners are expected to react to and work on the ECMO console in response to simulated clinical events. A commonly-used method to integrate an ECMO circuit to the manikin involves the connection of the access and return cannulae to a “bladder reservoir” hidden inside the manikin (Figure 2A). The presence of access ports on this volume reservoir (Figure 2B) allows injection or withdrawal of volume, and hence manipulation of pressure and volume status within the ECMO circuit. For example, access insufficiency is simulated by withdrawal of fluid, causing collapse of the reservoir, decreased ECMO flow, and negative access pressure. Circuit air entrainment may be simulated by the controlled introduction of air into the circuit. Depending on the specifications of the ECMO machine used, additional pressure transducers may be necessary to display the pressure measurements at different sites along the ECMO circuit (Figure 2C). This setup is simple and highly mobile, and allows simulation activities to be run even in institutions without dedicated simulation facilities.
However, there are both cost and technical considerations in using this model. In terms of budgetary estimation, expenses for the maintenance of ECMO machines and replacement of consumables (blood pump and membrane oxygenator) should be factored in. This poses economical concerns, especially for newly developed ECMO centers, or recurring simulation activities. The advancement of 3-D printing technologies for the construct of simulated oxygenators holds promise to curtail these costs (6).
Certain technical barriers limit the realism of this simulation model. First, it is difficult to demonstrate the difference in color of oxygenated and deoxygenated blood, which is an important visual cue in scenarios like oxygen supply failure. Other technical challenges include simulating blood clots in the blood pump and oxygenator. There is ongoing research to explore new possibilities, such as the use of thermochromic fluid to manipulate the ‘blood’ color in different parts of the circuit (6).
Scenario design
Scenario design is the “soul” of simulation training. Scenarios are designed with specific learning goals and objectives. The goal refers to the overall educational mission of the scenario, whereas objectives refer to the specific cognitive, psychomotor, behavioural, or affective skills the learners are expected to acquire after the training (7).
It is worthwhile to mention an important vision that the Extracorporeal Life Support Organization (ELSO) has about ECMO simulation training. All learners are trained to become ECMO specialists and hence are expected to adapt and take up the role of the ECMO specialist during simulation learning, regardless of their existing job positions as senior consultants, junior doctors, nurses, or perfusionists. For instance, nurses are encouraged to adjust the settings on the ECMO console independently as clinically appropriate, and doctors are expected to be “hands-on” in activities such as changing the ECMO circuit to the hand crank. Although contrary to routine role divisions, this is to ensure basic competency in troubleshooting and responding to ECMO emergencies. This training concept also reflects the reality that many ECMO centers nowadays adopt a “mixed ECMO care” model, with the ECMO team consisting of physicians, nurses, perfusionists, and respiratory therapists (8,9).
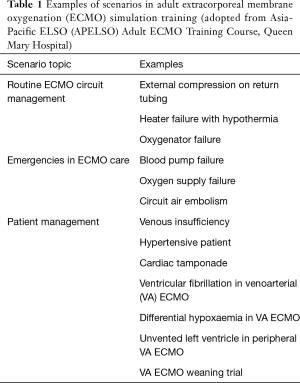
An important principle in scenario design is to take into account the background and experience of the learners. The same scenario can be modified according to the competency of the participants, and the goals and objectives should be clearly specified. For instance, in a scenario of ECMO blood pump failure, the goal for bedside nurses may be “to switch to a standby machine in emergency setting”, with objectives including “recognize the manifestation of blood pump failure and its related physiological changes” (cognitive), “acquire the technical skill of using hand crank or backup blood pump” (psychomotor) and “call for help immediately after problem identified” (behavioural). On the contrary, the goal for a group of experienced learners would be “demonstration of teamwork in managing blood pump failure crisis”, achieved through the objective of “exercising effective communication and leadership skills” (behavioural). Table 1 lists examples of basic scenarios used in an Asia-Pacific ELSO (APELSO) Adult ECMO Training Course.
Full table
Facilitators and debriefers
Apart from hardware considerations, well-trained simulation facilitators are instrumental to the success of a simulation program. ECMO simulation facilitators have to fulfill multiple roles. Firstly, they have to ensure the smooth running of simulation scenarios, provide necessary cues and information to the participants, and react appropriately to the learners actions. A thorough understanding of ECMO physiology and ECMO-patient interaction is a prerequisite for accurate and timely manipulation of the ECMO and physiological parameters. For example, in the scenario of hypovolemia in VA ECMO, facilitators have to withdraw volume from the reservoir to decrease the ECMO circuit flow, and simultaneously change the physiological parameters by dropping the SpO2, SvO2, mean arterial pressure and creating tachycardia. Normal parameters should be reinstated after the learners demonstrate appropriate response. The acquisition of these skills would imply additional training and resources at the starting phase of an ECMO simulation program, in the form of training the trainers, such as by attending advanced training programs provided by ELSO.
During the running of simulation activities, facilitators have to denote key actions and behaviours for discussion in the subsequent debriefing session. Special skills are required to conduct an effective debriefing. Debriefers should stimulate a conversation amongst learners and to guide them in discovering the “frame” behind their actions—the assumptions, knowledge, and feelings that drive their actions. Only when participants gain insight of their own frames would a simulation exercise lead to behavioural change (10).
Detailed discussion on the techniques in debriefing is beyond the scope of this article. The principles of confidentiality and mutual respect have to be strictly observed in order to create a safe environment for free communication, especially after difficult, stressful, or poorly-performed scenarios (11). There are established frameworks for the debriefing process. The most widely used tools include the three-step model (reaction, understanding, and summary) created by the Center for Medical Simulation at Harvard Medical School, and the “gather, analyze, and summarize” (GAS) model advocated by the Winter Institute for Simulation Education and Research (WISER) of University of Pittsburgh. Debriefers should familiarize themselves with different tools and adopt a systematic approach during debriefing.
Simulation training for crises in VA ECMO
A crisis is a time of intense difficulty or danger. Several characteristics intrinsic to the provision of VA ECMO continuously expose the service providers to such challenges.
- VA ECMO is often deployed under emergency and unplanned situations.
- The time to ECMO initiation is directly related to patient outcome (12).
- Providers often have to multi-task, especially in the initiation phase of VA ECMO—taking care of equally important issues such as airway management, emergency medications, and diagnostic workup.
- Patients supported by VA ECMO are usually critically ill and ECMO dependent, any complications related to equipment failure or human error have significant adverse effects on patient outcome.
- Many etiologies of circulatory failure require timely intervention by liaising with specialists not in the ECMO team, e.g., emergency percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG) (13).
- Robust data or guidelines on the use of VA ECMO in cardiac failure is lacking, which renders decision making dynamic. Many a time, critical decisions have to be made expeditiously, e.g., ECMO initiation for a borderline E-CPR candidate.
As a result of all these factors, VA ECMO providers are required to organize ECMO support, make clinical decisions, troubleshoot, demonstrate leadership, and communicate efficiently with healthcare professionals under high tension and time-pressured situations. Such situation may be made even more stressful and complex when the ECMO providers have to perform ECMO cannulation simultaneously. Simulation-based training with the goal of addressing interprofessional education (IPE) and crisis resources management (CRM) is especially suited to improve team performance, prevent error, and enhance patient safety.
The World Health Organisation (WHO) defines IPE as “when students from two or more professions learn about, from, and with each other to enable effective collaboration and improve health outcomes (14). Four major domains described as core interprofessional competencies are as follows (15):
- Values/ethics for interprofessional practice - healthcare professions are expected to work with other professions to maintain a climate of mutual respect and shared values;
- Roles/responsibilities—able to use the knowledge of own and other professions to address healthcare needs;
- Interprofessional communication—responsive and responsible communication to support team approach to treatment; and
- Teams and teamwork.
CRM is the articulation of principles of individual and crew behaviour in ordinary and crisis situations that focus on the skills of dynamic decision making, interpersonal behaviour and team management, in order to make use of all available resources to deliver safe and quality care (16).
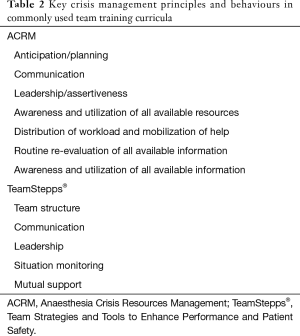
It was first introduced in 1970s in aviation industry (flight-simulator-based curriculum named crew resources management) and subsequently adopted by David Gaba in 1980s into the field of anaesthetic care [Anaesthesia Crisis Resources Management (ACRM)] (17). Since then, the concept of CRM has been incorporated into training curricula in high risk clinical areas (obstetrics, emergency medicine, critical care etc.) and various medical disciplines (18,19). While multiple standardized teamwork training curricula other than ACRM have since been developed, they all share a common focus on non-technical skills of the individual and team (Table 2).
Full table
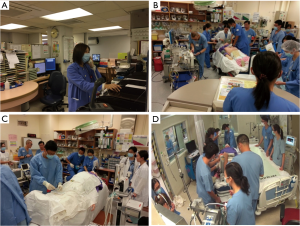
The principles of IPE and CRM are of paramount importance in ECMO emergencies. In these situations, healthcare professions with different background including ECMO specialists, perfusionists, paramedics, doctors from various specialities (e.g., emergency physicians, cardiologists, intensivists and cardiothoracic surgeons), nurses, paramedics, and social workers are required to work cohesively to handle the emergency (Figure 3). Table 3 illustrates some of the scenarios designed to address crisis management in an ECMO simulation training program.

Full table
Current status and the future of simulation in ECMO education
The importance of simulation training in ECMO education curriculum is increasing. Surveys conducted in the United States reported that 46% of the ECMO centres have an ECMO simulation program and 73% of the centres have adopted simulation as part of the institutional ECMO credentialing program (21,22). In 2017, ELSO included high-fidelity simulation into the training and continuing education guideline for ECMO physicians. In particular, the guideline highlighted the role of simulation in evaluating the knowledge and competency of the ECMO physician in managing ECMO related interventions in routine and emergency situations. It also recognized simulation training as an effective tool to train teamwork and communication skills (4).
There is ongoing research to investigate the impact of simulation training on ECMO outcomes. Studies have shown an improvement in confidence and performance in managing ECMO patient after simulation training. Allan et al. reported a shorter cannulation time in paediatric ECPR performed by cardiac surgical trainees. Su et al. reported a faster ECPR initiation time and Whitmore et al. reported a shorter time to achieve a full ECPR support simulation scenario after simulation training (23-25). Recently, Zakhary et al. published the first randomized controlled trial in ECMO simulation, comparing simulation training with water drill. The simulation group had a superior performance, gauged by achieving a higher scenario score and a shorter time to critical action. Notably, the superior performance was sustained at a 1-year evaluation (26).
At this juncture, the main criticism of simulation training is the lack of evidence that it translates to better patient outcomes. Only a multicentre trial with a standardized training curriculum and evaluated over an extended period will provide the answer. However, considering the long history and successful outcome of simulation training in the aviation industry, where running a randomized controlled trial is impossible, simulation training is very likely the most efficient and appropriate training tool for crises management in provision of ECMO care (27).
Conclusions
ECMO is a complex, high risk yet low volume clinical activity. VA ECMO, in particular, often a multidisciplinary collaboration in a stressful, dynamic and time-pressured environment, has imposed extra challenges to ECMO providers in terms of teamwork and interprofessional communication. In this aspect, simulation training is rapidly evolving as a probably superior training modality than traditional ECMO education methodologies. Further research is required to establish the effect of ECMO simulation training on patient outcomes.
Acknowledgments
The authors would like to acknowledge the support of the ECMO team members of the Department of Adult Intensive Care, Queen Mary Hospital.
Footnote
Conflicts of Interest: SW Sin and PC Lai are the education co-chairs of the Asia-Pacific Chapter of Extracorporeal Life Support Organization at the time of manuscript submission. The other authors have no conflicts of interest to declare.
References
- Abrams D, Garan AR, Abdelbary A, et al. Position paper for the organization of ECMO programs for cardiac failure in adults. Intensive Care Med 2018;44:717-29. [Crossref] [PubMed]
- Guerguerian AM, Ogino MT, Dalton HJ, et al. Setup and maintenance of extracorporeal life support programs. Pediatr Crit Care Med 2013;14:S84-93. [Crossref] [PubMed]
- Combes A, Brodie D, Bartlett R, et al. Position paper for the organization of extracorporeal membrane oxygenation programs for acute respiratory failure in adult patients. Am J Respir Crit Care Med 2014;190:488-96. [Crossref] [PubMed]
- ELSO Guidelines for Training and Continuing Education of ECMO Specialists. 2010. Available online: . Accessed 19 April 2018.http://www.elso.org/portals/0/igd/archive/filemanager/97000963d6cusersshyerdocumentselsoguidelinesfortrainingandcontinuingeducationofecmospecialists.pdf
- Kolb DA. Experiential Learning: Experience as the Source of Learning and Development. Upper Saddle River, New Jersey: Prentice Hall; 1984.
- Al Disi M, Alsalemi A, Alhomsi Y, et al. Revolutionizing ECMO simulation with affordable yet high-Fidelity technology. Am J Emerg Med 2018;36:1310-2. [Crossref] [PubMed]
- Johnston L, Williams SB, Ades A. Education for ECMO providers: Using education science to bridge the gap between clinical and educational expertise. Semin Perinatol 2018;42:138-46. [Crossref] [PubMed]
- Cavarocchi NC, Wallace S, Hong EY, et al. A cost-reducing extracorporeal membrane oxygenation (ECMO) program model: A single institution experience. Perfusion 2015;30:148-53. [Crossref] [PubMed]
- Daly KJ, Camporota L, Barrett NA. An international survey: the role of specialist nurses in adult respiratory extracorporeal membrane oxygenation. Nurs Crit Care 2017;22:305-11. [Crossref] [PubMed]
- Rudolph JW, Simon R, Raemer DB, et al. Debriefing as formative assessment: closing performance gaps in medical education. Acad Emerg Med 2008;15:1010-6. [Crossref] [PubMed]
- Gardner R. Introduction to debriefing. Semin Perinatol 2013;37:166-74. [Crossref] [PubMed]
- Chen YS, Lin JW, Yu HY, et al. Cardiopulmonary resuscitation with assisted extracorporeal life-support versus conventional cardiopulmonary resuscitation in adults with in-hospital cardiac arrest: an observational study and propensity analysis. Lancet 2008;372:554-61. [Crossref] [PubMed]
- Atkinson TM, Ohman EM, O'Neill WW, et al. A Practical Approach to Mechanical Circulatory Support in Patients Undergoing Percutaneous Coronary Intervention: An Interventional Perspective. JACC Cardiovasc Interv 2016;9:871-83. [Crossref] [PubMed]
- Framework for Action on Interprofessional Education & Collaborative Practice. 2010. Available online: . Accessed 19 April 2018.http://apps.who.int/iris/bitstream/handle/10665/70185/WHO_HRH_HPN_10.3_eng.pdf;jsessionid=D35AE4E68B396D44286ECBF4BBF4FFEF?sequence=1
- Paige JT, Garbee DD, Brown KM, et al. Using Simulation in Interprofessional Education. Surg Clin North Am 2015;95:751-66. [Crossref] [PubMed]
- Fanning RM, Goldhaber-Fiebert SN, Udani AD, et al. Crisis Resource Management. The Comprehensive Textbook of Healthcare Simulation. New York: Springer, 95-109.
- Howard SK, Gaba DM, Fish KJ, et al. Anesthesia crisis resource management training: teaching anesthesiologists to handle critical incidents. Aviat Space Environ Med 1992;63:763-70. [PubMed]
- Reznek M, Smith-Coggins R, Howard S, et al. Emergency medicine crisis resource management (EMCRM): pilot study of a simulation-based crisis management course for emergency medicine. Acad Emerg Med 2003;10:386-9. [Crossref] [PubMed]
- Nielsen PE, Goldman MB, Mann S, et al. Effects of teamwork training on adverse outcomes and process of care in labor and delivery: a randomized controlled trial. Obstet Gynecol 2007;109:48-55. [Crossref] [PubMed]
- ECMO Queen Mary Hospital AVALON cannulation model. 2017. Available online: . Accessed 28 March 2019.https://youtu.be/dr02RAMRk1A
- Weems MF, Friedlich PS, Nelson LP, et al. The Role of Extracorporeal Membrane Oxygenation Simulation Training at Extracorporeal Life Support Organization Centers in the United States. Simul Healthc 2017;12:233-9. [Crossref] [PubMed]
- Muratore S, Beilman G, John R, et al. Extracorporeal membrane oxygenation credentialing: where do we stand? Am J Surg 2015;210:655-60.e2. [Crossref] [PubMed]
- Allan CK, Pigula F, Bacha EA, et al. An extracorporeal membrane oxygenation cannulation curriculum featuring a novel integrated skills trainer leads to improved performance among pediatric cardiac surgery trainees. Simul Healthc 2013;8:221-8. [Crossref] [PubMed]
- Su L, Spaeder MC, Jones MB, et al. Implementation of an extracorporeal cardiopulmonary resuscitation simulation program reduces extracorporeal cardiopulmonary resuscitation times in real patients. Pediatr Crit Care Med 2014;15:856-60. [Crossref] [PubMed]
- Whitmore SP, Gunnerson KJ, Haft JW, et al. Simulation training enables emergency medicine providers to rapidly and safely initiate extracorporeal cardiopulmonary resuscitation (ECPR) in a simulated cardiac arrest scenario. Resuscitation 2019;138:68-73. [Crossref] [PubMed]
- Zakhary BM, Kam LM, Kaufman BS, et al. The Utility of High-Fidelity Simulation for Training Critical Care Fellows in the Management of Extracorporeal Membrane Oxygenation Emergencies: A Randomized Controlled Trial. Crit Care Med 2017;45:1367-73. [Crossref] [PubMed]
- Gaba DM. Crisis resource management and teamwork training in anaesthesia. Br J Anaesth 2010;105:3-6. [Crossref] [PubMed]


