Upper-esophageal inflammatory pseudotumor associated with middle-esophageal diverticulum: a case report
Introduction
Both esophageal inflammatory pseudotumor (IPT) and mid-esophageal diverticulum are rare benign diseases (1,2). Surgery is recommended for the symptomatic patients with esophageal IPT or mid-esophageal diverticulum (3). The goal of the present study is to report an extremely uncommon case, discuss the clinical and pathological aspects, and the surgical methods.
Case presentation
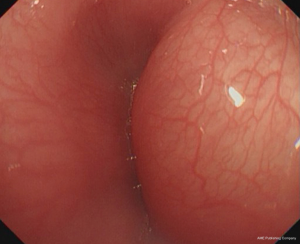
A 51-year-old male patient presented with a 7-day history of dysphagia. He had not suffered regurgitation, chest pain, substernal burning, weight loss or cough. Chest computed tomography revealed a soft tissue mass in the wall of the upper-thoracic esophagus that was projecting into the lumen as well as a diverticulum located in the right wall of the middle segment of the esophagus (Figure 1). Flexible esophagoscopy showed a submucosal swelling on the upper esophagus (Figure 2).

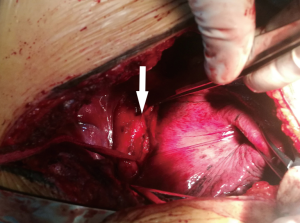
The preoperative diagnosis was esophageal leiomyoma and diverticulum, and exploration was undertaken through a right posterolateral fifth intercostal incision. During the intraoperative period, an ill-defined mass was discovered between the upper-thoracic esophagus and the trachea, with esophageal muscularis and mucosa involvement. Radical resection was nearly impossible due to the mass being very close to the tracheal membrane. After the frozen section of the mass revealed a benign lesion, about 2/3 of the tumor was resected to relieve symptom. The diverticulum was found in the middle segment of the esophagus. The diameter of neck was approximately 2.5 cm (Figure 3), and diverticulectomy was performed with a linear cut stapler.
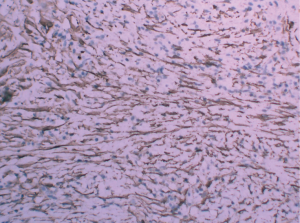
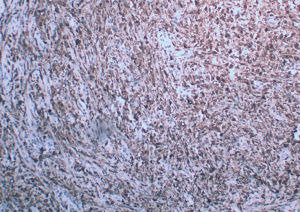
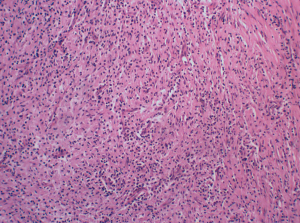
The final histopathology revealed that the tumor was composed of a spindle cell lesion with chronic inflammatory cells (Figure 4). Immunohistochemical analysis revealed that the tumor was positive for SMA (Figure 5), CD-68 (Figure 6), CD-138, and CD-43 and negative for Alk, CK, and desmin.
The patient fasted before the esophagogram with gastrografin, which had revealed that there was no leakage on the 5th day post-operation. He was discharged on the 8th day post-operation. The patient did not present with recurrent dysphagia or regurgitation at the 6-month follow up.
Discussion
IPT is a rare benign lesion that is composed of inflammatory cells and myofibroblastic spindle cells (1). The etiology of IPT remains unknown. IPT most commonly involves the lungs and the orbit, but it may also occur in the gastrointestinal tract (4). IPTs in the esophagus are extremely rare and originate in the esophageal submucosa. It was reported that esophageal IPTs were seen in the mid-or distal-esophagus, and they are frequently associated with mucosal ulceration (5). In this case, the IPT occurred in the upper esophagus without a mucosal ulceration. The appearance of gastrointestinal IPTs is usually as nodules or circumscribed masses that can be either sessile or polypoid, with the majority being solitary lesions that are rarely pedunculated. Clinical presentations of esophageal IPT include dysphagia, reflux, weight loss, melena or upper gastrointestinal bleeding. Radical surgery is suggested to patients with these symptoms (6). The treatment method for IPTs includes endoscopic removal, surgical excision, esophagectomy and thoracoscopic enucleation. A small IPT without muscularis propria involvement could be removed by endoscope, and esophagectomy should be a better procedure for large and obstructing esophageal IPTs. The IPT in this patient was sclerosus and close to the tracheal membrane, and performing radical surgery was nearly impossible; therefore, we performed surgical debulking to relieve the symptoms.
A mid-esophageal diverticulum is also a rare benign disease that occurs in the esophagus 5 cm above or below the carina (2). Mid-esophageal diverticula commonly occurs in developing countries where they result from mediastinal granulomatous inflammation secondary to tuberculosis, histoplasmosis or scarring (7,8). Most patients with mid-esophageal diverticula usually are asymptomatic. When patients are symptomatic, symptoms include dysphagia, regurgitation, halitosis, unintentional weight loss, substernal burning, chest pain, aspiration, cough, and choking (5). Surgical therapy is only indicated for patients with symptoms, including a large diverticulum, bleeding, inflammation, fistula, or with evidence of aspiration or carcinoma (9).
We suspect that mediastinal inflammation might be the cause in this case. Also, we thought the dysphagia resulted from the IPT. Surgery is unnecessary if the patient suffers from esophageal diverticulum without IPT. Because the two lesions were on the right side of the patient’s chest cavity, we chose the right thoracotomy incision. We also thought that a correct preoperative diagnosis was essential for the surgery.
Conclusions
In conclusion, both esophageal IPT and epiphrenic diverticula are rare. Their simultaneous occurrence in the same patient is extremely rare. Dysphagia is the most common associated syndrome, and surgery is recommended for symptomatic patients. Complete resection is preferred over surgical debulking. Whether or not a diverticulectomy is superior to the traditional treatment method cannot be concluded based on this case alone.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Sy K, Parfitt J, Marginean C, et al. Inflammatory pseudotumours of the oesophagus--histological and immunohistochemical findings. Histopathology 2015;66:1003-9. [Crossref] [PubMed]
- Thomas ML, Anthony AA, Fosh BG, et al. Oesophageal diverticula. Br J Surg 2001;88:629-42. [Crossref] [PubMed]
- Nehra D, Lord RV, DeMeester TR, et al. Physiologic basis for the treatment of epiphrenic diverticulum. Ann Surg 2002;235:346-54. [Crossref] [PubMed]
- Johnstone JM, Morson BC. Inflammatory fibroid polyp of the gastrointestinal tract. Histopathology 1978;2:349-61. [Crossref] [PubMed]
- LiVolsi VA. Perzin KH. Inflammatory pseudotumors (inflammatory fibrous polyps) of the esophagus. A clinicopathologic study. Am J Dig Dis 1975;20:475-81. [Crossref]
- Saklani AP, Pramesh CS, Heroor AA, et al. Inflammatory pseudotumor of the esophagus. Dis Esophagus 2001;14:274-7. [Crossref] [PubMed]
- Michael H, Fisher RS. Treatment of Epiphrenic and Mid-esophageal Diverticula. Curr Treat Options Gastroenterol 2004;7:41-52. [Crossref] [PubMed]
- Ferraro P, Duranceau A. Esophageal diverticula. Chest Surg Clin N Am 1994;4:741-67. [PubMed]
- Nastos D, Chen LQ, Ferraro P, et al. Long myotomy with antireflux repair for esophageal spastic disorders. J Gastrointest Surg 2002;6:713-22. [Crossref] [PubMed]
(English Language Editor: Jeremy Dean Chapnick, AME Publishing Company)