
Paramedic-initiated helivac to tertiary hospital for primary percutaneous coronary intervention: a strategy for improving treatment delivery times
Introduction
Primary percutaneous coronary intervention (PPCI) is well established as the optimal reperfusion strategy for patients presenting with ST-elevation myocardial infarction (STEMI), provided the time from patient symptom onset is <12 hours and first medical contact-to-balloon (FMCTB) time can be achieved within 120 minutes (1,2). However, outside the main metropolitan centres in New Zealand, access to onsite cardiac catheterisation laboratory (CCL) facilities do not exist. Therefore, regional STEMI patients are often subjected to prolonged transport delays before receiving PPCI if it is the chosen reperfusion strategy.
To address this location and time-to-treatment imperative for PPCI, various expedited regional patient transfer systems have been developed internationally, employing road-based emergency medical services (EMS) (3,4). In some countries this concept has extended to the use of rotor wing air ambulance services for distances to the nearest CCL that preclude road transport. However, these select helivac pathways have produced mixed results in achieving mandated balloon inflation times, and for a variety of reasons (5,6).
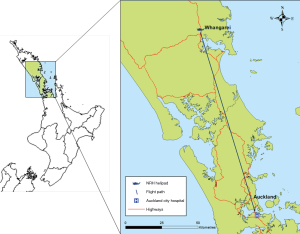
From a New Zealand perspective, in June 2010, Whangarei Base Hospital Emergency Department (WBH-ED) in regional Northland, commenced a helivac programme for STEMI patients to Auckland City Hospital Cardiac Intervention Unit (ACH-CIU) for PPCI. The distance is 155km, with an average flight time of 30 minutes. The programme had a target balloon-inflation time of <120 minutes from patient presentation at WBH-ED (the non-interventional centre) and utilised an established air ambulance service, the Northland Rescue Helicopter Trust (NRHT), operating 24/7 with Sikorsky-S76 airframes and based within a minute’s flying time of the hospital.
Despite its favourable features, this 3-year programme failed to consistently achieve its target treatment-delivery time. Only 24/57 patients (42.1%) received PPCI within 120 minutes, although the median time was close at 122 minutes (IQR 24) (7). The greatest contributor to delay was patient time spent in WBH-ED prior to transfer (median time 52 minutes, IQR 23), and this delay contributed 44% of the total time until PPCI was achieved. Of note, 32/57 patients (56%) were delivered to WBH-ED via ambulance, and the attending paramedics had already accurately determined the diagnosis of acute STEMI, prior to arriving at hospital.
It was this situation that prompted our investigation, a 48-month clinical trial of paramedic-initiated helivac of STEMI patients directly from the field in the Whangarei City area to ACH-CIU for PPCI. In contrast to the previous inter-hospital transfer programme, ambulance patients who met specific protocol criteria were transported directly to the NRHT helipad, bypassing WBH-ED. At the helipad, the duty flight intensive care paramedic (ICP) reassessed the patient before phoning the on-call interventional cardiologist at ACH-CIU, to have the patient accepted for transfer. Upon acceptance, the patient was flown directly to Auckland. The aim of our study was to trial this new paramedic-initiated helivac procedure, and to compare it with the previous physician-lead inter-hospital helicopter transfer programme. The primary outcome measures were: FMCTB time and accuracy of paramedic diagnosis. Secondary outcome measures were mortality at 30 days and six months, and hospital length of stay (LOS).
Methods
Design and setting
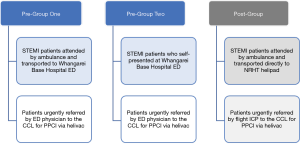
We utilised a prospective analysis of differences study design to compare three groups of STEMI patients, all of whom received PPCI but following two different models of patient identification and referral to the CCL. The first two groups, Pre-Group One and Pre-Group Two, were both historic control cohorts in the trial’s pre-implementation phase. Both groups were firstly assessed at WBH-ED before undergoing helivac to the ACH-CIU, following emergency physician referral. Pre-Group One consisted of STEMI patients initially attended and diagnosed by paramedics in the field, prior to being transported to WBH-ED, while Pre-Group Two consisted of STEMI patients who self-presented. The third group, Post-Group, was the prospective experimental cohort in the trial’s post-implementation phase, who underwent helivac to ACH-CIU following identification and direct referral from the field by independent attending flight ICPs. This process bypassed WBH-ED and occurred without physician oversight. For all three groups, the patients came from Whangarei City and all were transported to the same PCI centre via helicopter. The primary difference between both Pre-Groups combined and the Post-Group was the intervention – the implementation of a paramedic CCL activation protocol that permitted the paramedic-initiated referral process. In addition, the main comparison for this study was between the two ambulance cohorts, i.e., Pre-Group One and the Post-Group. Figure 1 provides a visual presentation and description of the three groups.
This trial was conducted within Whangarei, the main metropolitan centre for the region of Northland, New Zealand. The city has a population of 56,400 and is serviced by a single 246-bed, secondary-level public hospital. The city’s ambulance service has one centrally located station operating three double-crewed emergency ambulances 24/7. The NRHT aircraft hangars are located directly adjacent to the ambulance station. Crew configuration for the helicopters is two pilots and one flight ICP. Figure 2 illustrates the helicopter flight path used for the trial. Twenty-five intermediate and advanced life support level paramedics were enrolled in the study, consisting of eight flight ICPs and 17 road-based staff.
The trial’s receiving hospital, Auckland City Hospital (ACH), is a 1000-plus-bed, quaternary-level public hospital and the largest in New Zealand. Staff of the ACH-CIU are in-house from 8 am to 5 pm during weekdays, and outside this timeframe are expected to be on site within 30 minutes of laboratory activation. During the 2016 calendar year, the unit performed approximately 988 PCI procedures, of which 349 (35%) were acute primary.
Study population
The Pre-Groups included all patients from the previous hospital-based programme who were urgently referred and transported by air ambulance from WBH-ED to ACH-CIU with a diagnosis of STEMI. This period was June 2010 to June 2013. The Post-Group included all patients attended by paramedics in the Whangarei City area with a diagnosis of STEMI and who underwent helivac directly from the NRHT helipad to ACH-CIU following independent paramedic referral. This period was from June 2013 to June 2016. In addition, patients transported by road-based paramedics to the NRHT helipad during the post-implementation phase of the trial, but who were deemed ineligible for helivac by the duty flight ICP, were also investigated.
Sample size
To measure the primary outcomes of time-to-treatment and of accuracy of paramedic diagnosis, 60 patients (30 per group) were required for the trial’s main comparison, between ambulance cohorts, i.e., Pre-Group One and the Post-Group (8). This was based on a previous autonomous paramedic PPCI referral study involving 175 patients (9), and an a priori power analysis using their data. This was assuming a sensitivity of 70%, an accuracy measure of ±10% and an alpha level of 0.05, denoting a 95% confidence interval.
Measures
Patient characteristics
Key demographic data was collected to describe the patient sample population. Clinical characteristics on presentation were collected, plus patient cardiovascular disease risk factors. The time interval from symptom onset to receipt of 111 emergency call was calculated.
Time-to-treatment
Mandated treatment-related target time intervals were measured, per Cardiac Society of Australia and New Zealand (CSANZ) Guidelines (10) and compared between groups. These included:
- EMS patient contact to arrival at the CCL (ETD);
- EMS patient contact to balloon inflation (ETB);
- Patient arrival at the referral centre to balloon inflation (either WBH-ED in the trial’s pre-implementation phase, or the NRHT helipad in the trial’s post-implementation phase);
- First medical contact to balloon inflation (FMCTB);
- First diagnostic STEMI ECG to balloon inflation;
- Patient arrival at the interventional hospital to balloon inflation (DTB);
- Patient symptom onset to balloon inflation (total ischaemic time).
For those patients with a FMCTB time >120 minutes, a review of each case was conducted to determine the cause/s contributing to treatment delay.
Accuracy of paramedic diagnosis
Sensitivity and specificity, positive predictive value and negative predictive value of the accuracy of the flight intensive care paramedics’ clinical diagnoses were determined. This was possible only in the post-implementation phase of the study. Three independent cardiology consultants reviewed all cases after the fact, to determine accuracy of diagnosis and protocol application.
Patient clinical management and outcomes
The following data was collected for all three observed groups and analysed to determine patient outcomes:
- Clinical complications prior to undergoing PPCI, i.e., cardiogenic shock, compromising arrhythmia (not including those patients in cardiac arrest) and cardiac arrest;
- Inappropriate CCL activation;
- PCI procedural complications;
- Thirty-day and 6-month mortality;
- Hospital LOS.
Hospital LOS (measured in bed days) is an indicator of public health system costs. It can also indicate that other in-hospital interventions were necessary.
Intervention
Paramedic-initiated CCL activation protocol
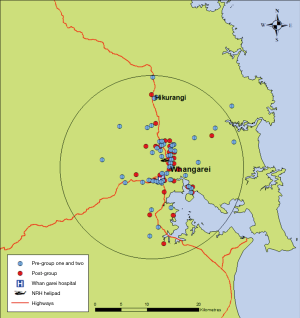
The paramedic protocol for PPCI referral (inclusion/exclusion criteria) applied in the post-implementation phase had several differences from those detailed within the CSANZ Guidelines (10) and used by emergency physicians in the trial’s pre-implementation phase. Firstly, an automated interpretation of STEMI was added as an additional inclusion criterion to mitigate the risk of erroneous ECG interpretation. Secondly, a new or presumed new left bundle branch block was not considered a STEMI equivalent and added as an exclusion from referral. In addition, to ensure key target time intervals were achieved, a catchment area was established. This was dictated primarily by the average ambulance transport time to the helipad, with outer boundaries within a 20-minute road travel timeframe (see Figure 3). Beyond this perimeter, STEMI patients were excluded from the helivac pathway and instead were assessed as to their suitability to receive prehospital fibrinolysis.
Data analysis
All analyses were performed using the Statistical Package for the Social Sciences software programme version 24. Initial analysis of data was primarily descriptive, producing frequencies, means and standard deviations, or medians and interquartile ranges where relevant, and testing for normal distributions of continuous measures. The observed groups were initially compared using where relevant: chi-square tests for independence, one-way analysis of variance or independent-sample t-tests. Comparisons of medians were made using Mann-Whitney U tests and Kruskal-Wallis tests. To examine the accuracy of paramedic decision making, the rates of “True Positive” and “True Negative” along with “False Positive” and “False Negative” cases were identified, and the sensitivity, specificity, positive predictive value and negative predictive value of paramedic diagnosis and protocol application were then calculated.
Results
Patient characteristics
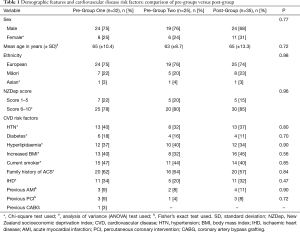
A total of 92 patients were included in the study: 32 patients in Pre-Group One, 25 in Pre-Group Two and 35 in the Post-Group. Table 1 reports on patient demographics and cardiovascular disease risk factors. These were similar overall between the three observed groups. Most patients were male (combined average age of 64 years, SD ± 10.3), of European ethnicity and residing in more socioeconomically deprived areas (as measured by the New Zealand Deprivation Index). Smoking, increased body mass index and a family history of acute coronary syndrome were the most prominent risk factors identified.
Full table
A map showing the spatial distribution of geo-coded residential addresses for patients within all three groups is presented in Figure 3, and relative to the designated catchment area in the trial’s post-implementation phase. All bar one patient from the pre-implementation phase are clustered within this boundary. Clinical characteristics of patients on initial presentation were similar between the three groups (Table 2).

Full table
No significant difference was identified between groups in terms of the time lapse between patient symptom onset and phoning 111 for ambulance assistance or self-presenting at hospital (P=0.36). The combined median time for this subinterval was 72 minutes (95% CI: 67−121 minutes). Sixty-eight percent of all patients presented during normal working hours, i.e., between 9 am and 5 pm.
Time-to-treatment
Table 3 provides a comparison of key treatment time intervals between all three groups. Note that balloon inflation times and the total ischaemic time exclude one patient in the Pre-Group One and two patients in the Post-Group. This was due to no device being inserted because of anatomy which precluded stent placement. For all measures, a significant improvement in time was demonstrated in favour of the Post-Group, except for ‘from arrival at interventional hospital to balloon inflation’, where no difference between groups was observed.
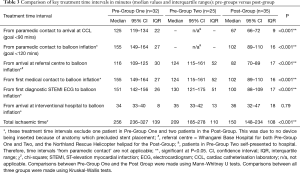
Full table
Note that for Pre-Group Two (self-presentation), the FMCTB time is equivalent to the sub-interval known as ‘door-to-device’, that is, from patient presentation at the referral hospital to balloon inflation. The median time shown exceeds the CSANZ benchmark standard of <120 minutes, with only 6/25 patients (24%) receiving treatment within this time-period.
Among those patients who received PPCI with a FMCTB time >120 minutes (n=53), prolonged emergency department assessment was the most common cause for delay, evident in more than three-quarters of all cases (77%), followed by the CCL being already occupied upon patient arrival (9% of cases). Among the 56 patients in total who received PPCI within the hospital-based referral system (i.e., both Pre-Groups), 50/56 (89.3%) had a FMCTB time >120 minutes. Emergency department assessment time contributed to 82% of these delays.
The flight times for all three groups were similar (P=0.71). Combined average flight time was 31 minutes (SD ±2). There was no difference between time-to-treatment (commencing from patient arrival at the referral centre) during normal working hours (8 am to 5 pm) versus outside of normal working hours (5 pm to 8 am) (P=0.48).
Accuracy of paramedic diagnosis
During the post-implementation phase, 57 patients were transported by ambulance paramedics to the NRHT helipad for reassessment by the duty flight ICP as to their suitability for helivac. Thirty-five of these patients (61%) were deemed eligible and subsequently flown to ACH-CIU; the remaining 22/57 patients (39%) were deemed ineligible and redirected to WBH-ED. Following audit review, none of the 35 helivac cases were deemed as inappropriate CCL activations. However, among the 22 patients excluded, one was misdiagnosed and did meet criteria for helivac. The accuracy of flight ICP diagnosis showed a sensitivity of 97% (95% CI: 85–99%), a specificity of 100% (95% CI: 84–100%), a positive predictive value of 100% (95% CI: 85–100%), and negative predictive value of 95% (95% CI: 84–99%). The single patient who was misdiagnosed received fibrinolysis in WBH-ED.
Among the 22 excluded cases, most patients presented with a STEMI-mimic on 12-lead ECG. The most common STEMI-mimic was left-ventricular hypertrophy (11/21), followed by left bundle branch block (5/21). Eighty-six percent of these false positive cases (18/21) occurred within the trial’s first 12 months.
During the post-implementation phase, an additional 13 STEMI patients eligible for helivac were transported by ambulance directly to WBH-ED due to aircraft unavailability. Of these 13 patients, four were later flown to ACH-CIU for PPCI while the other nine received prehospital fibrinolysis. Eight of these nine patients were then later flown to ACH-CIU for rescue PCI.
Patient clinical management and outcomes
Table 4 summarises key treatment features and outcomes for all patients. No significant differences between groups were identified, including clinical complications prior. Among all patients combined (n=92), no deaths occurred during helicopter transfer and only one patient required resuscitation in flight.
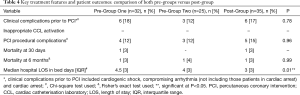
Full table
There were no significant differences in either 30-day or 6-month mortality between the three groups, but numbers were too small to be definitive. However, patients in the Post-Group experienced a significantly shorter hospital LOS compared to those in both the Pre-Groups.
Discussion
This study is the first to compare two distinct models of CCL activation and referral of STEMI patients for PPCI via helivac. Authorisation of this activation and referral process was the main distinction between the two models, and despite modest numbers, this study has demonstrated a significant time-saving, a 34-minute reduction in median FMCTB time in favour of the paramedic-initiated model. Moreover, significantly more patients received treatment within CSANZ benchmark timeframes.
The ETB time goal of <120 minutes was achieved among only 3% of relevant pre-implementation cases versus 91% of post-implementation cases, a 30-fold improvement. The total ischaemic time goal of <180 minutes was achieved in only 16–18% of pre-implementation cases versus 60% of post-implementation cases, a more than three-fold improvement.
These results compare favourably with similar aeromedical transfer pathways reported in the literature, including those that were physician-led, and/or inter-hospital based (5,6,11). They were also associated with a significant reduction in patient hospital LOS in favour of our paramedic-initiated model. Of note, there were no significant differences in demographic features, cardiovascular disease risk factors or clinical presentations between groups that would account for these differences in treatment times. Despite significant reductions in both treatment delivery times and hospital LOS, the study was underpowered to show either morbidity or mortality benefit.
Many studies have shown that failure to meet evidence-based treatment times may diminish the relative benefits of PPCI and its superiority over on-site fibrinolysis (12). Among proposed strategies to remedy this, internationally, paramedic-initiated referral and direct patient transport from the field to the CCL has yielded the most promising results. This more streamlined approach has shown markedly improved PCI delivery times compared to both physician-assisted paramedic models and improved in-hospital strategies (9,13,14). Our study has reaffirmed this in the New Zealand context and across a greater transport distance (155 km) than reported in similar trials (3,11,15,16).
For our four-year 57-case trial we experienced no inappropriate CCL activations, which can be costly and inconvenient, particularly outside of normal working hours when staff are on-call. Within the literature, acceptable rates of inappropriate activation by autonomous paramedics’ range between 5–20% (14,17). However, without our protocol of patient reassessment by the flight ICPs, as many as 20 patients may have been referred inappropriately by road paramedics. Our autonomous flight ICPs demonstrated highly accurate STEMI diagnosis and clinical decision making, and this, in part, serves to validate the study’s paramedic protocol, which included additional inclusion/exclusion criteria designed to mitigate the risk of misdiagnosis.
One potential limitation of our new protocol was the exclusion of more complex ECG criteria for STEMI, namely, the new or presumed new left bundle branch block. These can be difficult to determine in the out-of-hospital setting where there is often little or no access to patient medical records. In addition, the left bundle branch block criteria have been shown to be less sensitive and specific for the diagnosis (18,19). However, this study has demonstrated that New Zealand paramedics can determine patient eligibility for urgent PPCI referral (including ECG interpretation) with a high degree of accuracy. This provides support for broadening the ECG criteria for STEMI within New Zealand paramedic treatment protocols, something which has indeed occurred within the latest national ambulance Clinical Procedures and Guidelines (20). Notably, however, of the 57 patients assessed in the Post-Implementation phase of the trial, none presented with ECG evidence of either a new or presumed new left bundle branch block.
Among the 57 patients assessed in the post-implementation phase, 36 (63.1%) subsequently showed evidence of a culprit lesion on angiography. Thirty-five of these patients were referred to the CCL by the duty flight ICP but one was misdiagnosed—receiving fibrinolysis in WBH-ED. The remaining 21/57 patients were all STEMI-mimics. In part, this false positive number reflects the fact that road paramedics were encouraged to transport patients to the helipad (for reassessment by the flight ICP) if they were unsure of the diagnosis and if an automated ECG interpretation of STEMI was present. Most of these false positive cases (18/21) presented within the first 12 months of the trial. This suggests that as time progressed, road paramedic selection of patients improved substantially, likely attributable to greater familiarity with the new protocol plus regular staff feedback as part of the trial’s quality assurance process.
The median time delay between symptom onset and the patient seeking medical assistance (i.e., calling an ambulance or self-presenting at hospital) was 72 minutes (95% CI: 67–121 minutes, n=92, all groups combined). In the New Zealand context, these findings represent a moderate improvement to previous reports (21). However, continued public awareness and education is needed to reduce this delay and improve times to reperfusion.
Among patients in the trial’s post-implementation phase, a significantly shorter hospital LOS was observed. This is likely attributable to the time-saving advantage gained by our paramedic-initiated referral pathway, as the benefits of PPCI are directly proportional to total ischaemic time (22,23). This suggests there may be an economic benefit to our new paramedic-initiated pathway; however, our study’s sample size is too small to be definitive.
The primary deficiency of the inter-hospital helivac programme in the trial’s pre-implementation phase was the excessive time that patients spent in the emergency department prior to transfer: median time 52 minutes (95% CI: 50–67 minutes). The international benchmark for this sub-interval of ‘door in-door out’ is <30 minutes (17). Among the 56 patients who received PPCI within this hospital-based referral system, 50 (89.3%) had a FMCTB time >120 minutes. By excluding transport to the emergency department and activating the CCL team from the first point of care, our paramedic-initiated referral pathway achieved significantly shorter times to treatment. Moreover, this proved to be safe and feasible with no additional risk to the patient. The average flight time of 30 minutes provided adequate time for CCL staff to assemble and prepare for patient arrival, including outside of normal working hours.
Numerous randomised controlled trials comparing fibrinolysis with PPCI in the management of STEMI have produced unequivocal results in favour of PPCI as the superior reperfusion strategy in terms of infarct artery patency rates, morbidity and mortality (24-26). This superiority has also been consistent when inter-hospital transfer of patients to a PCI facility has occurred (11,16,27,28). However, the rates of those patients who receive PCI, and within optimal timeframes, is poor in New Zealand (29). This has been attributed to several factors, including: lack of adequate funding; patient location in relation to a PCI facility; time of day; and in particular, delays within emergency healthcare systems (29,30). The paramedic-based model of care presented in our study offers a viable strategy to address many of these issues.
Limitations
This study was not randomised and there were several differences in the PPCI referral protocols (inclusion/exclusion criteria) between the Pre-Groups and the Post-Group. However, all groups were demographically similar with similar clinical characteristics on initial presentation, so were considered comparable. The sample size for this study was small and it was underpowered to show morbidity or mortality benefit. Despite this, a significant improvement in time-to-treatment was able to be observed in favour of our experimental cohort. A cost efficacy analysis was beyond the remit of this study, but it would certainly be of interest to compare ultimate costs of the two models of referral. The study took place in just one New Zealand region (Northland) and may not be generalisable to other New Zealand regions, or other countries. However, other services may be able to utilise the study’s key concepts and develop similar pathways tailored to their own local setting.
Conclusions
This study has demonstrated that paramedic-initiated patient referral and helivac from the field to the CCL for PPCI is a safe and feasible strategy for the treatment of STEMI, a process that bypasses the emergency department and occurs without physician oversight. This approach provides a significant time-saving advantage for treatment delivery compared to an inter-hospital helicopter transfer model with physician referral, resulting in a significant reduction in hospital LOS. No difference in 30-day or 6-month mortality was observed, likely due to the small sample size. Paramedics demonstrated highly accurate clinical decision making with no inappropriate CCL activations occurring. Continued public education campaigns which encourage ACS patients to call for ambulance assistance immediately after symptom onset are required, to help reduce reperfusion times to within guideline targets.
Acknowledgments
We would like to thank Dr. Ryan Howard of WBH-ED and Dr Peter Ruygrok of ACH-CIU for their assistance in helping develop the paramedic pathway. We would also like to thank the New Zealand St John Ambulance Service, the NRHT and the paramedic participants for their commitment and contribution to this project.
Funding: This work was partially supported by the New Zealand Health Research Council (grant number 15/441) and St John Ambulance Service awarded to Dr Paul Davis PhD.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study protocol was approved by the New Zealand Health and Disabilities Ethics Committee - Northern A (14/NTA221) and the Auckland University of Technology Ethics Committee (15/04). Informed patient consent was not required, given this research was in the nature of an ‘industry audit’, which sort to determine that an expanded treatment referral protocol was being implemented effectively and producing the desired outcomes.
References
- O'Gara PT, Kushner FG, Ascheim DD, et al. 2013 ACCF/AHA Guideline for the management of ST-Elevation Myocardial Infarction. J Am Coll Cardiol 2013;61:e78-140. [Crossref] [PubMed]
- Ibanez B, James S, Agewall S, Antunes MJ, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J 2018;39:119-77. [Crossref] [PubMed]
- Widimský P, Budešínský T, Voráč D, et al. Long distance transport for primary angioplasty vs immediate thrombolysis in acute myocardial infarction. Final results of the randomized national multicentre trial--PRAGUE-2. Eur Heart J 2003;24:94-104. [Crossref] [PubMed]
- Nielsen PH, Maeng M, Busk M, et al. Primary angioplasty versus fibrinolysis in acute myocardial infarction. Circulation 2010;121:1484-91. [Crossref] [PubMed]
- McMullan JT, Hinckley W, Bentley J, et al. Reperfusion is delayed beyond guideline recommendations in patients requiring interhospital helicopter transfer for treatment of ST-segment elevation myocardial infarction. Ann Emerg Med 2011;57:213-20.e1. [Crossref] [PubMed]
- Sigmundsson TS, Gannarsson B, Benediktsson S, et al. Management of patients with STEMI transported with air-ambulance to Landspitali University Hospital in Reykjavik. Laeknabladid 2010;96:159-65. [PubMed]
- White JM, Howard R, Goldsmith R, et al. Safety and feasibility of patient transfer by helicopter for primary percutaneous coronary intervention. N Z Med J 2012;125:47-59. [PubMed]
- Faul F, Erdfelder E, Lang A, Buchner A. G. *Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods 2007;39:175-91. [Crossref] [PubMed]
- Cheskes S, Turner L, Foggett R, et al. Paramedic contact to balloon in less than 90 minutes: A successful strategy for ST-segment elevation myocardial infarction bypass to primary percutaneous coronary intervention in a Canadian emergency medical System. Prehosp Emerg Care 2011;15:490-8. [Crossref] [PubMed]
- ST-Elevation Myocardial Infarction Guidelines Group; New Zealand Branch of Cardiac Society of Australia and New Zealand. ST-elevation myocardial infarction: New Zealand Management Guidelines, 2013. N Z Med J 2013;126:127-64. [PubMed]
- Grines CL, Westerhausen DR, Grines LL, et al. A randomized trial of transfer for primary angioplasty versus on-site thrombolysis in patients with high-risk myocardial infarction: The air primary angioplasty in myocardial infarction study. J Am Coll Cardiol 2002;39:1713-9. [Crossref] [PubMed]
- Pinto DS, Kirtane AJ, Nallamothu BK, et al. Hospital delays in reperfusion for ST-elevation myocardial infarction: Implications when selecting a reperfusion strategy. Circulation 2006;114:2019-25. [Crossref] [PubMed]
- Clark CL, Berman AD, McHugh A, et al. Hospital process intervals, not EMS time intervals, are the most important predictors of rapid reperfusion in EMS patients with ST-segment elevation myocardial infarction. Prehosp Emerg Care 2012;16:115-20. [Crossref] [PubMed]
- Garvey JL, Monk L, Granger CB, et al. Rates of cardiac catheterization cancelation for ST-segment elevation myocardial infarction after activation by Emergency Medical Services or emergency physicians: Results from the North Carolina Catheterization Laboratory Activation Registry. Circulation 2012;125:308-13. [Crossref] [PubMed]
- De Luca G, Biondi-Zoccai G, Marino P. Transferring patients with ST-segment elevation myocardial infarction for mechanical reperfusion: A meta-regression analysis of randomized trials. Ann Emerg Med 2008;52:665-76. [Crossref] [PubMed]
- Widimský P, Groch L, Zelízko M, et al. Multicentre randomized trial comparing transport to primary angioplasty vs immediate thrombolysis vs combined strategy for patients with acute myocardial infarction presenting to a community hospital without a catheterization laboratory. The PRAGUE Study. Eur Heart J 2000;21:823-31. [Crossref] [PubMed]
- Moyer P, Ornato JP, Brady WJ, et al. Development of systems of care for ST-elevation myocardial infarction patients: The Emergency Medical Services and emergency department perspective. Circulation 2007;116:e43-8. [Crossref] [PubMed]
- Jain S, Ting HT, Bell M, et al. Utility of left bundle branch block as a diagnostic criterion for acute myocardial infarction. Am J Cardiol 2011;107:1111-6. [Crossref] [PubMed]
- Kontos MC, Aziz HA, Chau VQ, et al. Outcomes in patients with chronicity of left bundle-branch block with possible acute myocardial infarction. Am Heart J 2011;161:698-704. [Crossref] [PubMed]
- St John New Zealand. Clinical Procedures and Guidelines: Comprehensive edition 2016-2018. Auckland, New Zealand: St John, 2016.
- Tanner H, Larsen P, Lever N, et al. Early recognition and early access for acute coronary syndromes in New Zealand: key links in the chain of survival. N Z Med J 2006;119:U1927. [PubMed]
- McNamara RL, Wang Y, Herrin J, et al. Effect of door-to-balloon time on mortality in patients with ST-segment elevation myocardial infarction. J Am Coll Cardiol 2006;47:2180-6. [Crossref] [PubMed]
- Steg PG, Bonnefoy E, Chabaud S, et al. Impact of time to treatment on mortality after prehospital fibrinolysis or primary angioplasty. Circulation 2003;108:2851-6. [Crossref] [PubMed]
- Andersen HR, Nielsen TT, Rasmussen K, et al. A comparison of coronary angioplasty with fibrinolytic therapy in acute myocardial infarction. N Engl J Med 2003;349:733-42. [Crossref] [PubMed]
- Keeley EC, Boura JA, Grines CL. Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review of 23 randomised trials. Lancet 2003;361:13-20. [Crossref] [PubMed]
- Weaver WD, Simes RJ, Betriu A, et al. Comparison of primary coronary angioplasty and intravenous thrombolytic therapy for acute myocardial infarction. JAMA 1997;278:2093-8. [Crossref] [PubMed]
- Aversano T, Aversano LT, Passamani E, et al. Thrombolytic therapy vs primary percutaneous coronary intervention for myocardial infarction in patients presenting to hospitals without on-site ardiac surgery. JAMA 2002;287:1943-51. [Crossref] [PubMed]
- Zijlstra F. Angioplasty vs thrombolysis for acute myocardial infarction: a quantitative overview of the effects of interhospital transportation. Eur Heart J 2003;24:21-3. [Crossref] [PubMed]
- Ellis C, Devlin G, Matsis P, et al. Acute Coronary Syndrome patients in New Zealand receive less invasive management when admitted to hospitals without invasive facilities. N Z Med J 2004;117:U954. [PubMed]
- Williams M. Percutaneous coronary intervention in New Zealand. N Z Med J 2007;120:U2398. [PubMed]


