
Hybrid coronary revascularization versus off-pump coronary artery bypass grafting and percutaneous coronary intervention for the treatment of two-vessel coronary artery disease with proximal left anterior descending artery stenosis
Introduction
Hybrid coronary revascularization (HCR) was first reported by Angelini in 1996 (1), which combined the durability and survival advantage of left internal mammary artery (LIMA) to left anterior descending artery (LAD) grafting with less invasive percutaneous coronary intervention (PCI) to treat non-LAD lesions. HCR balanced the conflict between surgical trauma and long-term outcome. The transfusion rate, the hospital length of stay (LOS) and the intensive care unit (ICU) LOS of HCR were significantly lower than those of coronary artery bypass grafting (CABG) (2). Gasior et al. (3) reported that there was no difference in the incidence of death, myocardial infarction, and target vessel revascularization (TVR) 1 year after HCR and CABG. When compared to PCI, HCR demonstrated a lower incidence of main adverse cardiovascular and cerebrovascular events (MACCE) and cardiac adverse events, such as acute myocardial infarction (MI) and TVR (4). It can be seen that HCR can accelerate the recovery of patients after surgery, and the mid-term effect of HCR is not inferior to CABG and superior to PCI.
Compared with conventional CABG, off-pump coronary artery bypass grafting (OPCAB) can avoid systemic inflammation and ischemia-reperfusion injury caused by cardiopulmonary bypass (CPB) (5). In recent years, it has been widely used, especially in Asia. In the 5-year follow-up results of CORONARY study, the rates of death, stroke, MI, renal failure, and TVR in OPCAB and conventional CABG patients were comparable (6). In addition, HCRs are mostly performed with off-pump techniques, so it is reasonable to use OPCAB for comparison with HCR.
The treatment of two-vessel coronary artery disease (CAD) including proximal LAD stenosis is still controversial. According to the guidelines, both CABG and PCI are class I recommendations (7). For patients in this border area, HCR that incorporates surgical and interventional techniques may be a more reasonable option. This study sought to compare mid-term clinical outcomes of HCR with OPCAB and PCI for the treatment of two-vessel CAD including proximal LAD stenosis.
Methods
Study design
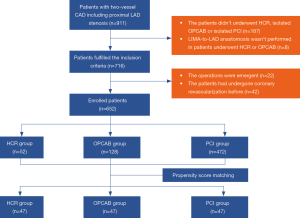
This study was a three-group, single-center, retrospective cohort study. The local Research Ethics Board of Rui Jin Hospital approved this retrospective cohort study. Data was collected from the local database of Rui Jin Hospital. The patients between January 2009 and December 2016 were selected for analysis. The inclusion criteria were as follows: (I) the patient underwent HCR, isolated OPCAB or isolated PCI; (II) the patient had two-vessel CAD including proximal LAD stenosis; (III) LIMA-to-LAD anastomosis was performed in patients underwent HCR or OPCAB; (IV) the stents used in HCR or PCI were drug eluting stents (DES). The exclusion criteria were as follows: (I) the operation was emergent; (II) the patient had undergone coronary revascularization before.
The patients were divided into the HCR group, the OPCAB group and the PCI group. Figure 1 shows the detailed flow of this study. All patients received aspirin 100 mg and clopidogrel 75 mg daily in the first year after surgery. Then, aspirin 100mg was continued for life.
Data collection
Patient demographics including gender, age, body mass index (BMI), family history and histories of hypertension, diabetes mellitus (DM), hyperlipoidemia, MI, stroke, chronic obstructive pulmonary disease (COPD), peripheral vessel disease (PVD) and smoking were obtained for all patients from the local database of Rui Jin Hospital. The preoperative ejection fraction (EF) was also obtained. EuroSCORE II was calculated on the basis of the original methodology (8). Coronary angiograms were analyzed by experienced technicians and scored according to the SYNTAX score algorithm (9).
Outcome measures
The primary endpoints of this study were mid-term main adverse cardiovascular and cerebrovascular events (MACCE), defined as the composite of death, MI, stroke or TVR. We measured the clinical outcomes, including perioperative and mid-term clinical outcomes.
“Perioperative” was defined as within 30 days after surgery. The perioperative clinical outcomes were as follow: (I) death; (II) MI, defined as MI type 5 according to Third Universal Definition of Myocardial Infarction (10); (III) stroke; (IV) TVR; (V) MACCE; (VI) the ICU LOS and the hospital LOS of the HCR group and the OPCAB group.
The mid-term clinical outcomes were as follows: (I) death; (II) MI; (III) stroke; (IV) TVR; (V) MACCE.
Follow-up
Hospital databases were checked annually to identify and review any routine follow-up information. In addition, all participants in the present study were contacted by telephone again by the research staff using standard procedures and forms.
Propensity score matching (PSM)
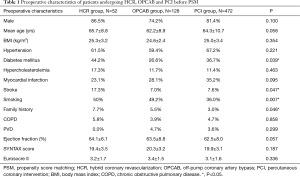
There were 52, 128 and 472 patients in the HCR, OPCAB and PCI group fulfilling the inclusion and exclusion criteria. In order to adjust for significant unbalanced individual characteristics among 3 groups, we used propensity scores (PSs) to reduce imbalance. A multivariate logistic regression model was employed to estimate PSs. All prespecified covariates are listed in Table 1. We chose caliper matching without a replacement for this study. The patients in the HCR group were matched with those in the OPCAB and PCI cohorts, with calipers of width 0.2 standard deviations of the logit of the PS. Covariate balance was measured using the t-test or χ2 analysis, in case of numerical or categorical variables, respectively.
Full table
Statistical analysis
Continuous data were summarized as mean (± standard deviation) or median (the 25th percentile, the 75th percentile), and categorical variables were summarized as frequencies or percentages. Continuous variables of the three groups were compared using ANOVA or Kruskal-Wallis test. After PSM, for perioperative outcomes, continuous variables of two groups were compared using paired t-tests or Wilcoxon signed-rank test. In the other situations, continuous variables of two groups were compared using Student’s t-test or Wilcoxon’s rank-sum test. After PSM, for perioperative outcomes, categorical variables of the three groups were compared using Bowker’s test and categorical variables of two groups were compared using McNemar’s test. In the other situations, categorical variables were compared using the χ2 test or Fisher exact test. The time to the first occurrence of each mid-term adverse event was described with the use of Kaplan-Meier curves (K-M curves), and the comparisons were performed with the stratified log-rank test. All analysis was performed with SPSS (IBM Corp. Released 2013. IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp) and R version 3.4.3. P<0.05 was considered statistically significant. A Dunn-Bonferroni test was used for post-hoc comparisons.
Results
Baseline characteristics of patients
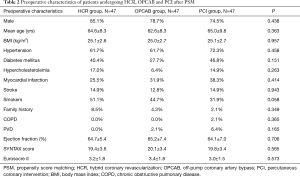
A total of 52 patients in the HCR group, 128 patients in the OPCAB group and 472 patients in the PCI group fulfilled the inclusion and exclusion criteria. There were 47 patients in each group after PSM. Tables 1 and 2 displays the preoperative patient characteristics before and after PSM. Before PSM, the distributions of gender, age, BMI, histories of hypertension, hyperlipoidemia, MI, COPD and PVD, preoperative EF, SYNTAX score and Euroscore II were comparable among 3 groups (P>0.05). There were significant differences in family history (P=0.046) and histories of DM (P=0.039), stroke (P=0.047) and smoking (P=0.007). After PSM, all the preoperative characteristics were comparable among 3 groups.
Full table
Perioperative outcomes
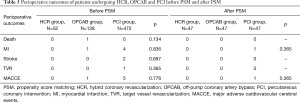
Table 3 shows the perioperative outcomes of 3 groups. The incidence of death, MI, stroke, TVR and MACCE were comparable among 3 groups before and after PSM (P>0.05).
Full table
But the ICU LOS was shorter in the HCR group than in the OPCAB group after PSM (21.8±5.3 vs. 27.8±6.4 hours, P<0.001), so was the hospital LOS (15.3±4.5 vs. 17.6±5.4 days, P=0.027).
Mid-term outcomes
The mean follow-up time was 59 months (interquartile range, 42 to 79 months). The follow-up rates of the HCR, OPCAB and PCI group were 93.6%, 95.7% and 95.7% respectively. The incidences of death, MI and stroke were comparable among 3 groups (P>0.05). HCR incurred MACCE rate and TVR rate lower than those with PCI (MACCE: 11.4% vs. 35.6%, P=0.007; TVR: 4.5% vs. 22.2%, P=0.015), but similar to those with OPCAB (MACCE: 11.4% vs. 13.3%, P=0.778; TVR: 4.5% vs. 2.2%, P=0.616) (Table 4).

Full table
The estimated 8-year freedom from MACCE in the HCR group (84.0%) was significantly higher than that in the PCI group (54.0%; P=0.008), but similar to that in the OPCAB group (64.5%; P=0.893) (Figure 2).

Discussion
In recent years, HCR has received more and more attention in the treatment of coronary heart disease. A meta-analysis showed that HCR had advantages in reducing in-hospital hemorrhage, shortening hospitalization and recovery time (11). The intubation time and ICU LOS in patients after HCR were significantly lower than those after conventional CABG (12,13). The potential beneficiaries for HCR include patients who cannot undergo sternotomy, patients with estimated poor recovery and patients with diabetes, COPD, recent MI or stroke (14), poor left ventricular function (EF <40%) and severe PVD (15). The American College of Cardiology Foundation /American Heart Association gave a class IIa recommendation for HCR in patients with one or more of the followings (16): (I) limitations to traditional CABG, such as heavily calcified proximal aorta or poor target vessels for CABG (but amenable to PCI); (II) lack of suitable graft conduits; (III) unfavorable LAD artery for PCI (i.e., excessive vessel tortuosity or chronic total occlusion). In patients with two-vessel CAD including proximal LAD stenosis, CABG and PCI are both class I recommendations, but there was no recommendation for HCR in these patients (7). CABG using LIMA is suitable for dealing with the lesions in important sites such as the left main coronary artery and LAD, while PCI is suitable for patients with low SYNTAX score. Patients with two-vessel CAD including proximal LAD stenosis are at the border of the two technologies. HCR that incorporates surgical and interventional techniques may be a more reasonable option for these patients.
In patients undergo HCR, LIMA-LAD grafts are performed via a left-sided thoracotomy between the 4th/5th interspace with special retractors suited for smaller incisions (4–5 cm). Although the LIMA is under direct visualization, doing this surgery through a smaller incision with a beating heart is technically challenging. This approach also requires single lung ventilation, which increase the difficulty of anesthesia. But the postoperative mortality and rates of MI, stroke, TVR and MACCE of HCR were comparable with those of OPCAB or PCI group in our center. This demonstrated that although HCR had a high requirement for surgical and anesthesia techniques, it did not increase postoperative risk in experienced cardiac centers and was safe and reliable in selected patients.
Although PSM has been performed in this study, the bias is still existing since the retrospective nature of this study. The attending physicians probably selected patients at a low clinical risk to undergo this procedure. This can be observed by the low rates of acute complications observed in this group in Table 3.
In this study, the ICU LOS and the hospital LOS of HCR were shorter than those of OPCAB. It seemed that the lesser invasiveness of HCR speeded up the recovery of patients. Meanwhile, according to the previous studies, the smaller incision of HCR reduces postoperative discomfort, risk of infection and transfusion, compared with CABG (17-19). And the quality of life 6 weeks after discharge is better in patients undergoing HCR (11). All of the above has given HCR a big advantage over OPCAB.
LIMA-LAD graft is one of the gold standards of coronary revascularization. Previous studies have concluded that the improved survival of CABG is derived from the excellent long-term patency rate of the LIMA-LAD graft (20). The LIMA graft has a better anti-atherogenic function than the vein graft, and meanwhile, its endothelium can secrete powerful vasodilators to protect downstream target vessels. Compared with bare-metal stents, DES significantly reduced the restenosis rate, which was similar to or lower than the failure rate of vein grafts (21). HCR retains the LIMA-LAD graft and replaces vein graft with DES. This strategy keeps the survival advantage of LIMA-LAD graft and has no negative effect on non-LAD lesions. Our mid-term results showed that the HCR group did not differ significantly from the OPCAB group in the incidence of MACCE, death, MI, stroke and TVR, which was consistent with the short-term results of previous studies (22).
For patients with high operative risk, PCI is a feasible revascularization strategy, due to the minimal invasiveness. Considering the superior long-term outcomes derived from the favorable patency of LIMA-LAD graft, especially in the patients with DM, renal sufficiency, advanced age (23-25), HCR seems to be a feasible alternative option. In our study, HCR offered relatively lower mid-term MACCE (the primary outcome) and TVR rates than PCI in patients with two-vessel CAD including proximal LAD stenosis.
Limitations
Firstly, this is a nonrandomized comparison. Although PSM has been used in this study, the potential limitation is there still may be residual confounders, as well as differences between groups due to nonblinding of both the patients and physicians. Secondly, the sample size of this study is very limited. The follow-up of the patients enrolled into this study will be continued and more patients will be enrolled in the future.
Conclusions
In this study, HCR is a safe and feasible procedure in an experienced cardiac center. It speeds up the recovery of patients and provides favorable mid-term outcomes for patients with two-vessel CAD including proximal LAD stenosis. It seems to be a promising treatment of CAD patients.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The local Research Ethics Board of Rui Jin Hospital approved this retrospective cohort study.
References
- Angelini GD, Wilde P, Salerno TA, et al. Integrated left small thoracotomy and angioplasty for multivessel coronary artery revascularisation. Lancet 1996;347:757-8. [Crossref] [PubMed]
- Bachinsky WB, Abdelsalam M, Boga G, et al. Comparative study of same sitting hybrid coronary artery revascularization versus off-pump coronary artery bypass in multivessel coronary artery disease. J Interv Cardiol 2012;25:460-8. [Crossref] [PubMed]
- Gąsior M, Zembala MO, Tajstra M, et al. Hybrid revascularization for multivessel coronary artery disease. JACC Cardiovasc Interv 2014;7:1277-83. [Crossref] [PubMed]
- Repossini A, Di Bacco L, Rosati F, et al. Hybrid coronary revascularization versus percutaneous strategies in left main stenosis: a propensity match study. J Cardiovasc Med (Hagerstown) 2018;19:253-60. [Crossref] [PubMed]
- Edmunds LH, Jr. Inflammatory response to cardiopulmonary bypass. Ann Thorac Surg 1998;66:S12-6; discussion S25-8.
- Lamy A, Devereaux PJ, Prabhakaran D, et al. Five-Year Outcomes after Off-Pump or On-Pump Coronary-Artery Bypass Grafting. N Engl J Med 2016;375:2359-68. [Crossref] [PubMed]
- Kolh P, Windecker S, Alfonso F, et al. 2014 ESC/EACTS Guidelines on myocardial revascularization: the Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). Developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI). Eur J Cardiothorac Surg 2014;46:517-92. [Crossref] [PubMed]
- Nashef SA, Roques F, Sharples LD, et al. EuroSCORE II. Eur J Cardiothorac Surg 2012;41:734-44; discussion 744-5. [Crossref] [PubMed]
- Sianos G, Morel MA, Kappetein AP, et al. The SYNTAX Score: an angiographic tool grading the complexity of coronary artery disease. EuroIntervention 2005;1:219-27. [PubMed]
- Thygesen K, Alpert JS, Jaffe AS, et al. Third universal definition of myocardial infarction. J Am Coll Cardiol 2012;60:1581-98. [Crossref] [PubMed]
- Harskamp RE, Bagai A, Halkos ME, et al. Clinical outcomes after hybrid coronary revascularization versus coronary artery bypass surgery: a meta-analysis of 1,190 patients. Am Heart J 2014;167:585-92. [Crossref] [PubMed]
- Hu FB, Cui LQ. Short-term clinical outcomes after hybrid coronary revascularization versus off-pump coronary artery bypass for the treatment of multivessel or left main coronary artery disease: a meta-analysis. Coron Artery Dis 2015;26:526-34. [Crossref] [PubMed]
- Zhu P, Zhou P, Sun Y, et al. Hybrid coronary revascularization versus coronary artery bypass grafting for multivessel coronary artery disease: systematic review and meta-analysis. J Cardiothorac Surg 2015;10:63. [Crossref] [PubMed]
- Holzhey DM, Jacobs S, Mochalski M, et al. Minimally invasive hybrid coronary artery revascularization. Ann Thorac Surg 2008;86:1856-60. [Crossref] [PubMed]
- Umakanthan R, Leacche M, Zhao DX, et al. Hybrid options for treating cardiac disease. Semin Thorac Cardiovasc Surg 2011;23:274-80. [Crossref] [PubMed]
- Hillis LD, Smith PK, Anderson JL, et al. 2011 ACCF/AHA guideline for coronary artery bypass graft surgery: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Thorac Cardiovasc Surg 2012;143:4-34. [Crossref] [PubMed]
- Aubin H, Akhyari P, Lichtenberg A, et al. Additional right-sided upper "Half-Mini-Thoracotomy" for aortocoronary bypass grafting during minimally invasive multivessel revascularization. J Cardiothorac Surg 2015;10:130. [Crossref] [PubMed]
- Kon ZN, Brown EN, Tran R, et al. Simultaneous hybrid coronary revascularization reduces postoperative morbidity compared with results from conventional off-pump coronary artery bypass. J Thorac Cardiovasc Surg 2008;135:367-75. [Crossref] [PubMed]
- Hu S, Li Q, Gao P, et al. Simultaneous hybrid revascularization versus off-pump coronary artery bypass for multivessel coronary artery disease. Ann Thorac Surg 2011;91:432-8. [Crossref] [PubMed]
- Avgerinos DV, Charitakis K. Hybrid coronary revascularization: present and future. Hellenic J Cardiol 2015;56:193-6. [PubMed]
- Carrié D, Berland J, Verheye S, et al. A multicenter randomized trial comparing amphilimus- with paclitaxel-eluting stents in de novo native coronary artery lesions. J Am Coll Cardiol 2012;59:1371-6. [Crossref] [PubMed]
- Shen L, Hu S, Wang H, et al. One-stop hybrid coronary revascularization versus coronary artery bypass grafting and percutaneous coronary intervention for the treatment of multivessel coronary artery disease: 3-year follow-up results from a single institution. J Am Coll Cardiol 2013;61:2525-33. [Crossref] [PubMed]
- Investigators B. The final 10-year follow-up results from the BARI randomized trial. J Am Coll Cardiol 2007;49:1600-6. [Crossref] [PubMed]
- Cameron A, Davis KB, Green G, et al. Coronary bypass surgery with internal-thoracic-artery grafts--effects on survival over a 15-year period. N Engl J Med 1996;334:216-9. [Crossref] [PubMed]
- Hemmelgarn BR, Southern D, Culleton BF, et al. Survival after coronary revascularization among patients with kidney disease. Circulation 2004;110:1890-5. [Crossref] [PubMed]


