
Necessity of thoracotomy in pulmonary metastasis of osteosarcoma
Introduction
In recent years, with the advances of comprehensive treatment, the survival rate for osteosarcoma patients with pulmonary metastasis has increased from 0% in 1970 (1) to 17–34% recently (2). Many studies have suggested that the prognosis of patients with pulmonary metastasis of osteosarcoma is closely related to the rate of tumor necrosis after chemotherapy, disease-free interval before recurrence, number of metastases and unilateral or bilateral metastases (3-6). Importantly, the most critical prognostic factor is whether the metastases can be completely removed (7,8). Therefore, surgical management is the primary choice for patients with pulmonary metastasis of osteosarcoma.
Additionally, with the rapid development of minimal invasive surgery technology, video-assisted thoracoscopic surgery (VATS) has been widely used in the resection of pulmonary tumor due to its advantages for the patient of mild postoperative pain and shorter hospital stays (9,10). However, the application of minimal invasive surgery in patients with pulmonary metastasis of osteosarcoma is limited because of the inability of direct vision or palpation to find and locate the metastasis. Despite of some new methods, such as intraoperative ultrasonic thoracoscope, preoperative lesion marker and metal filament localization, have been developed to try to deal with these problems (11). Relaying on preoperative computer tomography (CT) examination still affects the thoroughness of minimal invasive surgery for removal of pulmonary metastatic tumors.
Nearly 35% of all patients who underwent pulmonary metastasis surgery for osteosarcoma, according to one study, were underdiagnosed by preoperative CT in accessing the number of pulmonary lesions relative to the number of pathologically determined metastases after surgery (12). This study analyzed surgeries for patients with pulmonary metastasis of osteosarcoma carried out in our hospital over 10 years. Through subgroup analysis of CT scan thickness, the era of operation, and the number of nodules detected by preoperative CT, we explored the necessity of thoracotomy for patients with pulmonary metastasis of osteosarcoma.
Methods
Inclusion and exclusion criteria
All patients had osteosarcoma and underwent radical orthopedic surgical resection of primary lesions, and were then transferred to oncology department for comprehensive systemic chemotherapy. All patients were assessed by oncology physicians and thoracic surgeons together. Here it was confirmed that there were no extra-pulmonary metastasis and ideal treatment had been carried out. The possibility of complete resection of metastases was high and the perioperative risk was low. After that, the patients were transferred to thoracic surgery for resection of pulmonary metastases.
We collected a total of 106 records of surgical operations for pulmonary metastases of osteosarcoma, in our hospital, from January 2008 to July 2018. Among which four operations were excluded for thoracoscopic palliative resection or an involvement of hilar lymph node, mediastinum, parietal pleura or chest wall. Considering the interplay between nodules, patients with diffused pulmonary lesions (>25 nodules), either on preoperative CT scan or found intraoperatively, were also excluded. In addition, those patients having six operations without available preoperative CT images were removed. In total, 96 thoracic surgeries which were performed on 69 patients were finally included. This study was approved by ethics of committee of Shanghai Sixth People’s Hospital and the approval number is 2019-ky-005.
Radiological analysis
All patients were routinely followed up for CT scans with a layer thickness of 5 or 7 mm (either German Siemens Sonatom Sensation Cardiac64 or American GE LightSpeed VCT64). Two radiologists, with more than 10 years of experience, who did not participate in the surgical operation and did not know the postoperative pathological results of resected nodules, counted the number of pulmonary nodules separately on the operation side according to the latest CT images before surgery. When there were different numbers of the nodules in the same patient diagnosed by two radiologists, a third radiologist was asked to confirm and review the results together. If the number of nodules counted on preoperative CT scan was not less than the number of pathologically confirmed metastases, the CT examination was a predictive one for the detection of metastases. Otherwise, it would be considered as an underestimated one. When CT overestimated the number of metastases, only the number of pulmonary nodules resected increased, which did not affect the tumor prognosis. The situation was different when CT underestimated the number of metastases which led to missed resection.
Surgical method
All operations were performed by the same team of thoracic surgeons led by an attending surgeon with more than 10 years of working experience. Double-lumen endotracheal intubation, conventional posterolateral incision, 5th or 6th intercostal approach to the chest were used in the operation. During thoracotomy, each surgeon involved in the operation systematically palpated the whole lung in turns, and all the nodules touched were wedge resected regardless of size, texture and location. After the pleural cavity was washed with warm water, each surgeon palpated the whole lung twice again in order to make sure that no suspicious nodules were missed. All included patients had highly suspected metastatic tumors on preoperative CT examination. Unless suspected nodules existed on the opposite side of preoperative CT simultaneously, contralateral thoracotomy was not routinely performed.
Pathologic analysis
All pulmonary specimens resected during surgery were examined under a microscope separately by two pathologists with more than 15 years of working experience. If a wedge resected specimen contained multiple metastases, the pathological diagnosis would be counted separately. But if the nodules were fused together and needed additional incisions to separate them, the pathological diagnosis was considered as one metastatic lesion. Our pathological report did not give feedback either on the necrosis rate or the tumor activity of the metastases, but we recorded the nature and number of non-osteosarcoma metastatic nodules.
Statistical analysis
For data with a non-normal distribution, such as the number of nodules on CT examination, the number of nodules resected during thoracotomy and the number of lesions pathologically confirmed as metastases after surgery, were described by median, range and quartiles of each distribution. The age, number of nodules on CT, size of nodules, and intervals between CT examination and surgery were analyzed across subgroups by Wilcoxon signed rank test. The Spearman correlation coefficient between the number of nodules on CT before surgery and the number of lesions pathologically confirmed as metastases were also calculated. All statistical analyses were completed using SPSS 20.0.0 and statistical significance was set at P<0.05.
Results
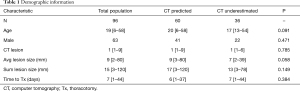
There are 69 patients totally included in this study, of which 45 are males (as presented in text). But the 69 patients had underwent 96 thoracic surgeries (some patients had more than one thoracic operation). Among the 96 thoracic surgeries, 63 were performed on males (as showed in Table 1). There was no significant difference in gender between the patients of CT predicted group and patients of CT underestimated group (P=0.471). The median number of thoracotomies per patient was 1 (range 1–4), the median age of patients was 19 (range, 6–58). The age of patients in CT predicted group (median 20 years; range, 6–58) and patients in CT underestimated group (median 17 years; range, 13–54) had no statistical difference (P=0.091). A total of 178 pulmonary lesions were found in preoperative CT examination (median 1 per CT; range, 1–9). There was no statistically significant difference in the amounts of nodules on preoperative CT between the patients in CT predicted group (median 1; range, 1–9) and the patients in CT underestimated group (median 1; range, 1–6) (P=0.785). The median mean diameter of nodules was 9 mm (range, 2–80 mm) and the median sum of nodule diameter was 15 mm (range, 3–120 mm). Finally, the median intervals between CT examination and operation was 7 days (range, 1–44 days). There was no statistically significant difference, in diameter and interval, between the two groups (P=0.058, P=0.149, P=0.384).
Full table
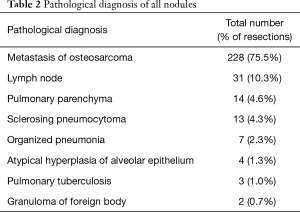
In 96 thoracotomies, there were only 178 nodules detected on CT scanning before surgery, but 302 nodules were found and removed by palpation during operations, of which 228 (75.5%) were confirmed metastatic lesions by pathological examination. In addition, 50 (40.3%) of the 124 nodules, omitted by CT scanning while detected by palpation were metastatic lesions. The pathological diagnosis of all nodules resected intraoperatively is shown in Table 2. There were more nodules resected in the patients in CT predicted group than patients in CT underestimated group, and there was a statistically significant difference between the two groups (P=0.003).
Full table
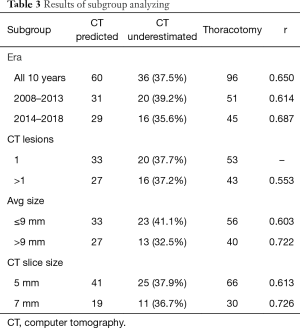
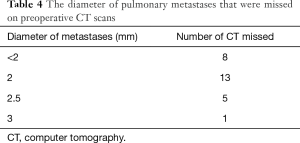
Table 3 lists the probability that preoperative CT examination underestimated the number of pulmonary metastatic nodules in patients, the correlation coefficient between the counts of nodules on CT and the number of actual pulmonary metastases, and the corresponding correlation coefficient of subgroup analyses. Subgroups were arranged according to the era of surgery, the number of nodules and the thickness of CT layer. Thirty-six preoperative CT scans in a total 96 thoracotomies (37.5%) underestimated the number of pulmonary metastases. The correlation coefficient between the number of nodules on CT and the number of pulmonary metastases confirmed pathologically was 0.65, confirming the existence of a positive correlation. Table 4 shows the diameters of pulmonary metastases that were missed on preoperative CT scans, and it is clear that the omitted nodules were small in diameter.
Full table
Full table
Discussion
Since CT examination is more sensitive than X-ray chest plain film, it is been regarded as the best method to diagnose pulmonary metastatic tumor. However, there are many studies showing that CT cannot detect the exact number of pulmonary metastases accurately (13,14). In this study, we have confirmed the inadequacy of routine CT examination in determining the number of pulmonary metastases of osteosarcoma. Despite the development of image technology and the thinner CT slice thickness in the past decade, the probability of CT scans omitting the metastases has not declined. Also, the correlation between the number of nodules on preoperative CT and the number of metastasis resected by palpation has not increased significantly.
If the minimal invasive surgery is performed in patients with pulmonary metastasis of osteosarcoma, CT images might be the only reference for the resection of the pulmonary lesions. While some small tumors can be accurately located and precisely resected with the help of preoperative or intraoperative techniques in VATS, minimal invasive surgery can only guarantee to resect all nodules detected on CT scan. Certainly could not resect any nodes not shown on CT images, which will inevitably lead to incomplete lung metastases resection. Conventional thoracotomy is not only to find and resect the nodules detected by CT scanning rapidly and accurately, but also find more lesions not detected by CT through careful palpation so as to realize the complete resection of the metastatic lesions. Some studies supported the use of minimal invasive surgery in selected patients recently (15,16), but these researches all have the disadvantages of small sample size and highly specific patients.
In view of previous studies, it has been shown that the crucial factor influencing the prognosis of patients with pulmonary metastasis of osteosarcoma is whether pulmonary metastases are completely resected (7,8). Therefore, we believe that if thoracic surgeons only perform the VATS for resection of pulmonary metastases according to the number of nodules shown by preoperative CT examination, without palpation, the goal of radical resection will certainly not be achieved.
Conclusions
This research demonstrated that nearly 37.5% preoperative CT examinations neglected the pulmonary metastases of osteosarcoma. Additionally, correlation between the number of nodules on preoperative CT and the number of resected metastases was not high. Subgroup analysis showed that these indicators have not changed significantly in the past 10 years, nor did they change with the thickness of CT slices and the number of nodules on preoperative CT. This result supports the recommendation that thoracotomies be performed using direct palpation for complete removal of pulmonary metastases secondary to osteosarcoma.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study was approved by ethics of committee of Shanghai Sixth People’s Hospital and the approval number is 2019-ky-005.
References
- Marcove RC, Miké V, Hajek JV, et al. Osteogenic sarcoma under the age of twenty-one. A review of one hundred and forty-five operative cases. J Bone Joint Surg Am 1970;52:411-23. [Crossref] [PubMed]
- Osasan S, Zhang M, Shen F, et al. Osteogenic sarcoma: a 21st century review. Anticancer Res 2016;36:4391-8. [Crossref] [PubMed]
- Meazza C, Scanagatta P. Metastatic osteosarcoma: a challenging multidisciplinary treatment. Expert Rev Anticancer Ther 2016;16:543-56. [Crossref] [PubMed]
- Harting MT, Blakely ML, Jaffe N, et al. Long-term survival after aggressive resection of pulmonary metastases among children and adolescents with osteosarcoma. J Pediatr Surg 2006;41:194-9. [Crossref] [PubMed]
- Kimura H, Suzuki M, Ando S, et al. Pulmonary metastasectomy for osteosarcomas and soft tissue sarcomas. Gan To Kagaku Ryoho 2004;31:1319-23. [PubMed]
- Rasalkar DD, Chu WC, Lee V, et al. Pulmonary metastases in children with osteosarcoma: characteristics and impact on patient survival. Pediatr Radiol 2011;41:227-36. [Crossref] [PubMed]
- Ward WG, Mikaelian K, Dorey F, et al. Pulmonary metastases of stage IIB extremity osteosarcoma and subsequent pulmonary metastases. J Clin Oncol 1994;12:1849-58. [Crossref] [PubMed]
- Goorin AM, Delorey MJ, Lack EE, et al. Prognostic significance of complete surgical resection of pulmonary metastases in patients with osteogenic sarcoma: analysis of 32 patients. J Clin Oncol 1984;2:425-31. [Crossref] [PubMed]
- Nykäinen A, Räsänen J, Salo J, et al. Thoracoscopic surgery of lung cancer. Duodecim 2014;130:145-51. [PubMed]
- Cheng AM, Wood DE. Minimally invasive resection of early lung cancers. Oncology (Williston Park) 2015;29:160-6. [PubMed]
- Keating J, Singhal S. Novel methods of intraoperative localization and margin assessment of pulmonary nodules. Semin Thorac Cardiovasc Surg 2016;28:127-36. [Crossref] [PubMed]
- Kayton ML, Huvos AG, Casher J, et al. Computed tomographic scan of the chest underestimates the number of metastatic lesions in osteosarcoma. J Pediatr Surg 2006;41:200-6; discussion 200-6. [Crossref] [PubMed]
- Ciccarese F, Bazzocchi A, Ciminari R, et al. The many faces of pulmonary metastases of osteosarcoma: retrospective study on 283 lesions submitted to surgery. Eur J Radiol 2015;84:2679-85. [Crossref] [PubMed]
- Ellis MC, Hessman CJ, Weerasinghe R, et al. Comparison of pulmonary nodule detection rates between preoperative CT imaging and intraoperative lung palpation. Am J Surg 2011;201:619-22. [Crossref] [PubMed]
- Mineo TC. Thoracoscopic approach to lung metastases. Minerva Chir 2008;63:511-6. [PubMed]
- Numan RC, Baas P, Klomp HM, et al. Optimal surgical management of pulmonary metastases: VATS versus thoracotomy. Respirology 2016;21:188-90. [Crossref] [PubMed]


