Rapid growing huge teratoma: complete surgical resection
Introduction
The most common causes of anterior mediastinal tumor include thymoma, germ cell tumor, thyroid disease, and lymphoma (1). Germ cell tumors are found in young adults and represent 15% of anterior mediastinal masses. Most common germ cell tumors are benign teratomas that grow very slowly (2). Complete surgical resection is the treatment of choice for such tumors, although this is sometimes difficult and requires careful attention in the case of larger tumors (2). We report our successful experience with complete resection of a large mediastinal teratoma showing rapid growth.
Case
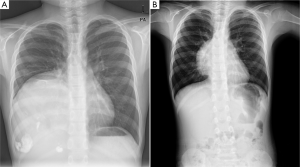
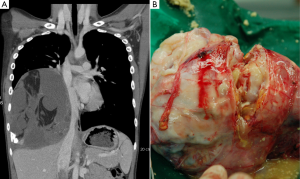
An 11-year-old male with frequent upper respiratory symptoms visited our hospital for chest computed tomography. Chest radiography performed in a local hospital revealed a large mass occupying the right thoracic cavity (Figure 1A). A chest radiograph from three years prior also demonstrated a mediastinal mass neighboring the right cardiac border (Figure 1B). However, no further work-up was performed at that time. Chest computed tomography in our hospital revealed a mediastinal mass, measuring 14 cm in largest diameter, occupying most of the right thoracic cavity (Figure 2A). The tumor showing a heterogeneous nature compressed the right lung parenchyma, but it had not become totally atelectatic. There was no prominent evidence of local invasion into neighboring organs. However, the mass compressed the right atrium and inferior vena cava (Figure 2A).
Preparation
The decision was made to remove the tumor. Left decubitus position was simulated before surgery to anticipate the mass effect on the inferior vena cava and right atrium. Fortunately, the patient had stable vital signs and did not complain of any other symptoms. A single lumen endotracheal tube with endobronchial blocker was prepared for single-lung ventilation. Forestalling the possibility of adhesions or invasions to the mediastinal organs or lungs, extracorporeal membrane oxygenation (ECMO) was utilized. A central line (6 Fr) via the internal jugular vein and two peripheral venous catheters (20 gauge) were prepared for unexpected bleeding or urgent intravenous medication. The vital signs were not changed after anesthesia, and surgery was performed with no extraordinary events.
Approach and pitfall
We selected the sixth intercostal space for our surgical approach. The mass seemed to have developed from the thymus or a thymus-neighboring organ based on comparison of the old and new chest X-rays (Figure 1A,B). Based on this finding, the fourth or fifth intercostal space would have been optimal for identifying the origin of the mass. However, the mass had occupied the end of the diaphragm and the costophrenic angle, and we could not guarantee absence of invasion or adhesion around the diaphragm space. Therefore, to anticipate dissection of the lower right thorax area, the sixth intercostal space was selected and easily widened without rib resection. There was no pleural adhesion or effusion. The mass was determined to have originated from the thymus and was attached along the side of the phrenic nerve. Phrenic nerve sparing is important to preserve lung functions, especially in young patients. Thermal instrument use was avoided and meticulous dissection with Metzenbaum scissors was performed in order to not injure the nerve. Although there was no adhesion between the parietal pleura and the mass, a fibrous band and adhesion was observed between the pericardial space and the mass. Finger palpation and blunt dissection were used because direct visualization was not possible. Tumor punctuation could have provided additional information and simplified the surgery, especially if the tumor had been cystic. However, the outer surface was not cystic and was difficult to aspirate, so tumor punctuation was not performed. After surgery, the lung was expanded to fill the space even if long term compression by the mass. The patient recovered without problems, and the chest tube was removed on postoperative day 3. The patient was discharged without complications. The pathological examination revealed a benign mature teratoma containing hair, teeth, and other sebaceous material (Figure 2B). The patient showed stable vital signs and normal chest X-ray in the outpatient clinic.
Discussion
Posterolateral thoracotomy was inevitable in this case. If the surgery had been performed when the mass was small, some minimally invasive surgical techniques including video-assisted thoracoscopic surgery or robotic surgery could have been utilized (3,4). However, by the time of presentation to our hospital, the mass had grown to a large size that prevented use of the technique. Median sternotomy with anterior thoracotomy was applied in a similar case (2). However, thoracotomy without a second incision was sufficient in this case, possibly due to the absence of tight adhesion or invasion between the mass and pleura. The flexible intercostal space of the 11-year-old boy also made this technique possible. In fact, rib resection or additional intercostal incision was not required even for extraction of the mass. Moreover, the patient did not complain of postoperative chest pain except tolerable discomfort.
Meticulous preoperative preparation might be also inevitable in such cases. Teratoma patients typically do not complain of major symptoms regardless of the size of the mass; however, the mass effect can be serious (2,5,6). In addition, surgery may be difficult in some cases (5,7). Therefore, preoperative simulation of the surgical position, application of a central catheter, and even ECMO should be considered. A meticulous surgical technique is also imperative so as to not injure a mediastinal structure such as the phrenic nerve, vagus nerve, or hilar structures. Decisive dissection with finger palpation is required because direct visualization of all entire mass is sometimes impossible, especially with large masses.
In conclusion, resection of a very large mediastinal mass occupying the right hemithorax via posterolateral thoracotomy was performed in an 11-year-old boy. Our meticulous preoperative preparation and surgical technique were effective and resulted in no postoperative complications and favorable recovery.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Duwe BV, Sterman DH, Musani AI. Tumors of the mediastinum. Chest 2005;128:2893-909. [PubMed]
- Yokoyama Y, Chen F, Date H. Surgical resection of a giant mediastinal teratoma occupying the entire left hemithorax. Gen Thorac Cardiovasc Surg 2013. [Epub ahead of print]. [PubMed]
- Melfi F, Fanucchi O, Davini F, et al. Ten-year experience of mediastinal robotic surgery in a single referral centre. Eur J Cardiothorac Surg 2012;41:847-51. [PubMed]
- Rothermel L, Gilkeson R, Markowitz AH, et al. Thoracoscopic resection of a giant teratoma compressing the right heart. Interact Cardiovasc Thorac Surg 2013;17:594-7. [PubMed]
- Zisis C, Rontogianni D, Stratakos G, et al. Teratoma occupying the left hemithorax. World J Surg Oncol 2005;3:76. [PubMed]
- Avci A, Eren S. Life-threatening giant mediastinal cystic teratoma in a 4-month-old male baby. Gen Thorac Cardiovasc Surg 2009;57:389-91. [PubMed]
- Miyazawa M, Yoshida K, Komatsu K, et al. Mediastinal mature teratoma with rupture into pleural cavity due to blunt trauma. Ann Thorac Surg 2012;93:990-2. [PubMed]