
Selective serotonin re-uptake inhibitors: risk of blood product transfusion and inotrope requirements in patients undergoing cardiac surgery
Introduction
Depression is a serious mental health disorder. The World Health Organization postulated that by 2020 depression will be the second greatest contributor to the global economic burden of diseases (1). Patients undergoing cardiac surgery exhibit a high prevalence of concomitant depression. A substantial number of these patients demonstrate worsening symptoms of depression after cardiac surgery resulting in higher rates of post-operative complications, longer hospital length of stay, and reduced return to activity (2-6).
The exact etiology of depression is not known, however, some studies have showed that polymorphisms in the serotonin transporter gene are associated with an increased incidence of depression (7,8). The first-line pharmacological treatment modality for depression includes selective serotonin re-uptake inhibitors (SSRIs) (9). Despite their efficacy, SSRIs are not without their own side-effects. A number of studies have recently reported an increase in upper gastro-intestinal bleeding events in depressed medical patients on SSRI therapy (10). Furthermore, studies in orthopedic surgical patients have also demonstrated increased perioperative blood loss and bleeding related complications owing to the platelet-inhibiting nature of serotonin (11-13).
The evidence for increased perioperative operative bleeding in cardiac patients receiving SSRI therapy is scarce. Xiong et al. demonstrated that patients on SSRIs were more likely to receive blood transfusion during coronary revascularization surgery (14). On the contrary, Andreasen et al. reported no differences in post-operative blood transfusion or 30-day mortality between patients with or without SSRIs (15). A large retrospective cohort of 530,416 patients undergoing major elective surgery (including cardiac surgery) showed that patients receiving SSRIs had higher odds of in-hospital mortality, bleeding, and readmission at 30 days (16). A more recent study by Sajan et al. found explored a smaller sample size of 767 patients and found that preoperative use of SSRIs was associated with increased exposure to allogeneic blood transfusion in surgical patients at high risk for perioperative bleeding (17).
Majority of patients undergoing cardiac surgery receive substantial doses of fentanyl during the perioperative period. Another aspect of SSRI therapy is a potential interaction with fentanyl. In a dose dependent manner fentanyl has serotoninergic properties that maybe associated with a subclinical serotoninergic syndrome resulting in hypotension and increased requirement for inotropic support, particularly in anesthetized patients (18).
We conducted a retrospective observational study to determine if preoperative SSRI therapy was associated with higher rates of perioperative blood product transfusion, higher incidence of inotropic requirements in patients undergoing elective cardiac surgery.
Methods
Population and sampling
After Institutional Research Ethics Board approval, we conducted a retrospective observational study on all patients undergoing cardiac surgery at Toronto General Hospital between January 1, 2008 and December 31, 2009. Information was analyzed from the Toronto Anesthesia Perioperative Outcomes Database, a large longitudinal database consisting of prospectively collected perioperative data. The Electronic Patient Record was used for any variables not included in the database. For patients with multiple database entries, data regarding the earliest surgery was collected in order to avoid multiple operations as confounders. Patients undergoing emergency surgery, or surgery without cardiopulmonary bypass (CPB) were excluded.
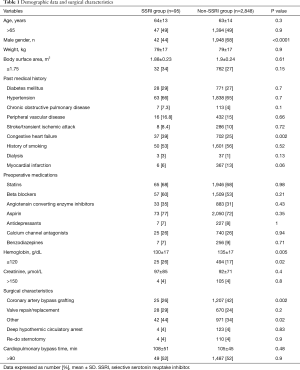
Demographic and pre-operative variables
Baseline preoperative variables collected included age, sex, body surface area, smoking history, past medical history, preoperative medications, baseline hemoglobin, creatinine, and planned surgical procedures. In addition, patients were also classed on basis of increased risk predictors such as age >65 years, body surface area ≤1.75 m2, preoperative hemoglobin ≤120 g/dL, and creatinine value >150 µmol/L. SSRI status was determined as a dichotomous variable. All patients were divided into two groups, either with (SSRI group) or without (non-SSRI group) SSRIs.
Intra-operative variables
The following intra-operative variables were collected: type of surgery (coronary artery bypass grafting, or cardiac valve replacement/repair, or others including repairs of congenital heart defects, left ventricular aneurysmectomies, re-do sternotomy procedures), CPB time, deep hypothermic circulatory arrest, the use of inotropes, and blood product transfusion.
Post-operative variables
The following post-operative variables were collected: myocardial infarction, stroke and transient ischemic attack, seizures, atrial fibrillation, ventricular arrhythmia requiring medical treatment, pacemaker insertion, low cardiac output syndrome, renal failure, inotropic requirements, transfusion of packed red blood cells, fresh frozen plasma, and platelets, chest re-exploration, mechanical ventilation time, intensive care unit and hospital length of stay, and hospital mortality.
Statistical analysis
The primary outcome included combined intraoperative and postoperative blood product transfusion. Transfusion of red blood cells, fresh frozen plasma, and platelets were analyzed separately. Secondary outcome was composite inotrope utilization during the perioperative period.
The patient cohort was divided into two groups based on the pre-operative SSRI status. Age, body surface area, hemoglobin, creatinine, and CPB times were presented as continuous as well as dichotomous variables. These included age >65 years, body surface area <1.75 kg/m2, preoperative hemoglobin <120 g/dL, preoperative creatinine >150 µmol/L, and CPB time >90 minutes. The following inotropes (milrinone, epinephrine, norepinephrine, vasopressine) were combined into the binary composite outcome.
We investigated the association between the preoperative SSRI status and primary and secondary outcomes, adjusting for potential confounders, with the use of logistic regression. A number of potential confounders were selected using prior knowledge of association with the outcome, as well as clinical judgment. Covariates with P<0.25 in the univariate analysis were chosen in conjunction with SSRI status for the multivariate models. A parsimonious model was built for the outcomes of interest (use of inotropes and blood product transfusion), having SSRI as a covariate, while the rest of the covariates were selected from an initial pool of potential confounders such as preoperative creatinine >150, hemoglobin <120, age >65 years, history of congestive heart failure, and diabetes mellitus, complex surgery (combined or re-do surgery), requirement for deep hypothermic circulatory arrest. According to the model building procedure (19) the univariate association of each one of the potential confounders with the outcome was tested (using chi-square and t-test for categorical and continuous variables respectively) and the covariates with some evidence of association (P<0.25) were kept as the initial set of covariates in the model along with the SSRI status. A subsequent stepwise variable selection procedure was followed where a model with significant covariates was identified. Finally, any variables excluded in univariate analyses were tested again in the model and kept in if they were significant. The differences between the groups were assessed using the chi-square test for nominal variables, the Mann-Whitney U test for ordinal variables and the Student’s t-test for continuous variables. A two-tailed significance level of P<0.05 was set for all univariate analyses and a Bonferroni correction was applied for multiple comparisons. A P value of less than 0.05 was considered significant. Statistical analysis was performed using STATA 12.1 (StataCorp., College Station, Texas, USA).
Results
A total of 2,943 patients were included in the study, with 95 (3.2%) patients receiving SSRI therapy. Demographic data and surgical characteristics are presented in Table 1. Univariate analysis showed that patients in SSRI group were more likely to be female, have history of congestive heart failure, preoperative anemia, and likelihood of having more complex surgery, received more inotropes and fresh frozen plasma during the perioperative period, and were more likely to have chest reopening for bleeding during the early postoperative period (Table 2). There was no difference in postoperative morbidity and mortality between the SSRI and non-SSRI groups. The intensive care unit and hospital length of stay was also similar between the two groups (Table 2).
Full table

Full table
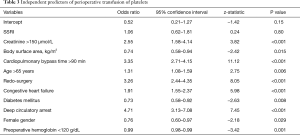
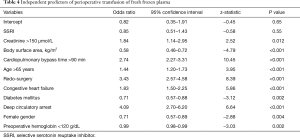
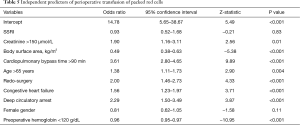
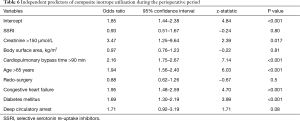
SSRI variable was not significant in any of the multivariate models, indicating the lack of evidence of association between the SSRIs and either blood product transfusion (Tables 3-5), or inotrope requirements (Table 6). Bootstrap adjusted calibration plots did not reveal severe over fitting of any of the models.
Full table
Full table
Full table
Full table
Discussion
The risk of perioperative bleeding and transfusion in surgical patients receiving SSRI therapy has been studied in general, orthopedic, gynecological, and cardiac surgical contexts, with inconsistent results. We have conducted a large retrospective review of 2,943 patients undergoing wide range of cardiac surgical procedures to determine if preoperative SSRI therapy was associated with higher rates of blood product transfusion, and increased incidence of inotropic requirements during the perioperative period. Even though univariate analysis showed that patients receiving SSRIs were more likely to require inotropic support and fresh frozen plasma transfusion, after adjusting for multiple covariates this association was no longer significant.
The current study adds to the body of evidence regarding the controversy in the literature related to SSRI therapy and increased incidence of allogeneic blood product transfusion in cardiac surgical patients. While Xiong et al., Auerbach et al., and Sajan et al. established a link between the SSRI therapy and increased bleeding and blood transfusion, Andreasen et al., Kim et al., and Tully et al. reported negative findings (14-17,20,21).
A recent meta-analysis of observational studies found a significant increase of red blood cell transfusion in patients receiving SSRI treatment but no difference in mortality when compared to patients that did not receive SSRI therapy (22). However, this meta-analysis was heavily weighted by a single study that reported that patients receiving SSRIs were more likely to receive 1–2 units of blood more than patients without SSRI therapy, but there was no association with increased blood loss or major transfusion risk between the two groups (23). These findings were also supported by a more rigorous statistical approach of propensity match of 1,417 pairs of patients based on their preoperative SSRI status. In this study, the presence of SSRI therapy was not associated with increased risk of bleeding or transfusion during cardiac surgery (24).
In the current study we assessed transfusion of red blood cells, fresh frozen plasma, and platelets in separate statistical models. Preoperative SSRI therapy was associated with a lack of increased risk of transfusion with any of the blood product components. However, all statistical models confirmed that the presence of well-known predictors of increased transfusion risk remained significant. These predictors included smaller body surface area, female gender, older age, low baseline hemoglobin levels, high creatinine, increased CPB time, presence of deep hypothermic circulatory arrest, complex cardiac surgery, history diabetes mellitus, and congestive heart failure. It is likely that the presence of these established risk factors negated the potential for increased transfusion risk associated with SSRI therapy. In addition, the use of tranexamic acid in cardiac surgery is a routine clinical practice in our institution. The dose of tranexamic acid ranged from 50 mg/kg in simple cases to 100 mg/kg in complex cardiac surgery. It is possible that the routine use of tranexamic acid further minimized the potential for increased transfusion rates in patients receiving SSRI therapy. Several mechanisms of increased risk of bleeding risk in patients receiving SSRI therapy have been proposed with most prevalent SSRI mediated platelet inhibition, and inhibition of enzymes involved in metabolism of anticoagulant medications through cytochrome P450 complex (10).
However, a lack of increased risk of bleeding with SSRI therapy was recently reported in patients receiving anticoagulation therapy for atrial fibrillation in a non-surgical setting (25).
In the current study, the SSRI treatment was not associated with increased inotrope utilization. However, older age, elevated creatinine, increased CPB time, and history of diabetes mellitus, and congestive heart failure remained significant factors in predicting higher rates of inotropic use. It is not surprising as all of these predictors identify a higher surgical risk subgroup of patients. Again, SSRI treatment in this particular setting likely plays a minor role.
The present study has a number of limitations. First, this was a retrospective review and the baseline characteristics of patients with and without SSRI therapy were different. However, our statistical approach was robust enough to adjust for most of the covariates to minimize bias. Second, we did not look at the different types of SSRIs, however, there have been no previous reports to identify that one subgroup of SSRIs would be more or less harmful than others.
The future research in this area will likely be required. Use of a prospective case-control design with abstraction of individual SSRI types, and quantification of SSRI dose or pre-operative serum serotonin or SSRI levels, may permit isolation of specific medications implicated in bleeding events, and may permit the determination of a threshold effect of SSRIs or serotonin on bleeding events, if one exists. Findings from such studies may prompt re-evaluation of treatment recommendations for patients with depression, especially those with identified cardiac risk factors that may in the future require surgical intervention. The current evidence suggests that modifying preoperative therapy pertinent to SSRI treatment is not warranted.
Acknowledgments
The authors would like to acknowledge the support of the Department of Anesthesia, the Divisions of Vascular and Cardiovascular Surgery at Toronto General Hospital, University Health Network, Toronto, Ontario, Canada.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was approved by the Institutional Research Ethics Board of Toronto General Hospital.
References
- Fleishman M. Economic grand rounds: psychopharmacosocioeconomics and the global burden of disease. Psychiatr Serv 2003;54:142-4. [Crossref] [PubMed]
- Beresnevaitė M, Benetis R, Taylor G, et al. Depression predicts perioperative outcomes following coronary artery bypass graft surgery. Scand Cardiovasc J 2010;44:289-94. [Crossref] [PubMed]
- Burg MM, Benedetto MC, Rosenberg R, et al. Presurgical depression predicts medical morbidity 6 months after coronary artery bypass graft surgery. Psychosom Med 2003;65:111-8. [Crossref] [PubMed]
- Contrada RJ, Boulifard DA, Hekler EB, et al. Psychosocial factors in heart surgery: presurgical vulnerability and postsurgical recovery. Health Psychol 2008;27:309-19. [Crossref] [PubMed]
- Copeland LA, Zeber JE, Pugh MJ, et al. Postoperative complications in the seriously mentally ill: a systematic review of the literature. Ann Surg 2008;248:31-8. [Crossref] [PubMed]
- Mallik S, Krumholz H, Lin Z, et al. Patients with depressive symptoms have lower health status benefits after coronary artery bypass surgery. Circulation 2005;111:271-7. [Crossref] [PubMed]
- Caspi A, Sugden K, Moffitt T, et al. Influence of life stress on depression: moderation by a polymorphism in the 5-HTT gene. Science 2003;301:386-9. [Crossref] [PubMed]
- Brown GW, Harris TO. Depression and the serotonin transporter 5-HTTLPR polymorphism: a review and a hypothesis concerning gene-environment interaction. J Affect Disord 2008;111:1-12. [Crossref] [PubMed]
- Khawam EA, Laurencic G, Malone DA Jr. Side effects of antidepressants: an overview. Cleve Clin J Med 2006;73:351-3. [Crossref] [PubMed]
- Andrade C, Sandarsh S, Chethan K, et al. Serotonin reuptake inhibitor antidepressants and abnormal bleeding: a review for clinicians and a reconsideration of mechanisms. J Clin Psychiatry 2010;71:1565-75. [Crossref] [PubMed]
- van Haelst IMM, Egberts TCG, Doodeman H, et al. Use of serotonergic antidepressants and bleeding risk in orthopedic patients. Anesthesiology 2010;112:631-6. [Crossref] [PubMed]
- Movig KL, Janssen MW, de Waal Malefijt J, et al. Relationship of serotonergic antidepressants and need for blood transfusion in orthopedic surgical patients. Arch Intern Med 2003;163:2354-8. [Crossref] [PubMed]
- Lip GYH, Andreotti F, Fauchier L, et al. Bleeding risk assessment and management in atrial fibrillation patients. Executive Summary of a Position Document from the European Heart Rhythm Association, endorsed by the European Society of Cardiology Working Group on Thrombosis. Thromb Haemost 2011;106:997-1011. [Crossref] [PubMed]
- Xiong GL, Jiang W, Clare RM, et al. Safety of selective serotonin reuptake inhibitor use prior to coronary artery bypass grafting. Clin Cardiol 2010;33:E94-8. [Crossref] [PubMed]
- Andreasen JJ, Riis A, Hjortdal VE, et al. Effect of Selective Serotonin Reuptake Inhibitors on Requirement for Allogeneic Red Blood Cell Transfusion Following Coronary Artery Bypass Surgery. Am J Cardiovasc Drugs 2006;6:243-50. [Crossref] [PubMed]
- Auerbach AD, Vittinghoff E, Maselli J, et al. Perioperative use of selective serotonin reuptake inhibitors and risks for adverse outcomes of surgery. JAMA Intern Med 2013;173:1075-81. [Crossref] [PubMed]
- Sajan F, Conte JV, Tamargo RJ, et al. Association of Selective Serotonin Reuptake Inhibitors with Transfusion in Surgical Patients. Anesth Analg 2016;123:21-8. [Crossref] [PubMed]
- Koury KM, Tsui B, Gulur P. Incidence of serotonin syndrome in patients treated with fentanyl on serotonergic agents. Pain Physician 2015;18:E27-30. [PubMed]
- Hosmer DW, Lemeshow S. Applied Logistic Regression, Second Edition. New York: Wiley, 2000.
- Kim DH, Daskalakis C, Whellan DJ, et al. Safety of Selective Serotonin Reuptake Inhibitor in Adults Undergoing Coronary Artery Bypass Grafting. Am J Cardiol 2009;103:1391-5. [Crossref] [PubMed]
- Tully PJ, Cardinal T, Bennetts JS, et al. Selective Serotonin Reuptake Inhibitors, Venlafaxine and Duloxetine are Associated With in Hospital Morbidity but Not Bleeding or Late Mortality After Coronary Artery Bypass Graft Surgery. Heart Lung Circ 2012;21:206-14. [Crossref] [PubMed]
- Eckersley MJ, Sepehripour AH, Casula R, et al. Do selective serotonin reuptake inhibitors increase the risk of bleeding or mortality following coronary artery bypass graft surgery? A meta-analysis of observational studies. Perfusion 2018;33:415-22. [Crossref] [PubMed]
- Gagne JJ, Polinski JM, Rassen JA, et al. Selective serotonin reuptake inhibitor use and perioperative bleeding and mortality in patients undergoing coronary artery bypass grafting: A cohort study. Drug Saf 2015;38:1075-82. [Crossref] [PubMed]
- Smith MM, Smith BB, Lahr BD, et al. Selective Serotonin Reuptake Inhibitors and Serotonin-Norepinephrine Reuptake Inhibitors Are Not Associated With Bleeding or Transfusion in Cardiac Surgical Patients. Anesth Analg 2018;126:1859-66. [Crossref] [PubMed]
- Quinn GR, Hellkamp AS, Hankey GJ, et al. Selective Serotonin Reuptake Inhibitors and Bleeding Risk in Anticoagulated Patients With Atrial Fibrillation: An Analysis From the ROCKET AF Trial. J Am Heart Assoc 2018;7:e008755. [Crossref] [PubMed]


