
A comparative study of thoracoscopic sympathectomy for the treatment of hand sweating
Introduction
Primary hyperhidrosis (PH) is a disease with the primary symptoms being excessive sweating in the palms as well as in the armpits and pedals that are not secondary to metabolic disease (such as hyperthyroidism and hypermetabolism) or other systemic disease. It can have a severe negative impact on patients’ work and daily life (1). In recent years, with the development of thoracoscopic minimally invasive surgery (2), thoracoscopic bilateral sympathectomy has been proven to be a safe and effective treatment (3). However, some patients suffer a common complication after surgery, namely compensatory hyperhidrosis (CH). It has been found that the occurrence of CH has a close relationship with the plane of sympathectomy. Specifically, the lower the plane is, the less likely CH is to occur (4-6). Currently, there is extensive clinical research exploring the treatment of PH to minimize postoperative complications and improve patients’ satisfaction. Here, we report a comparative study of thoracoscopic T3 and T4 sympathectomy for the treatment of hand sweating, where 192 patients from December 2010 to October 2014 underwent thoracoscopic bilateral sympathectomy and achieved satisfactory results.
Methods
Clinical data
A total of 192 consecutive patients with PH in our hospital were involved in this study. The patients included 88 males and 104 females, and the age range was 15 to 42 years old at the time of surgery, with 75% of them being between 16 to 30 years old. Patients’ primary symptoms were excessive sweating in the palms, armpits, and the pedals. In some severe cases, the patients have flushing hands and dripping sweat. The inclusion criteria for patients were as follows: (I) aged from 14 to 45 years old; (II) severe sweating symptoms causing considerably negative impact on patient’s work and daily life; (III) suffering from PH for a long time, and having poor response to drug therapy. Patients whose sweating was caused by metabolic diseases such as hyperthyroidism or hypermetabolism, tuberculosis, and other systemic diseases, were excluded from the study. According to the PH classification proposed by Lai et al. (7,8), the distribution of the patients was as follows: Grade I (mild, palm skin moist), 0 cases; Grade II (moderate, obvious palm skin sweating which can wet a layer of handkerchief), 100 cases; Grade III (severe, sweat dripping on both hands), 92 cases. Among the patients, 53 had armpit sweating, and 145 had pedal sweating. The duration of disease ranged from 5 to 20 years (an average of 13 years) (9). Patients all had preoperational examinations such as a chest X-ray, electrocardiogram and so on, and underwent the double-lumen intubation during thoracoscopic bilateral sympathectomy. There were no statistically significant differences in gender, age, degree of hand sweating, and postoperative follow-up between these two groups. Details are shown in Table 1.

Full table
Surgical methods
The double-lumen endotracheal intubation was used for general anesthesia, and patients’ heart rate, blood pressure, and oxygen saturation were monitored during surgery. The position of patients was 30°–45° half sitting, with 90° arm outreach, and a thermometer placed in the palm to measure the temperature before and after surgery. Two small incisions of about 0.5 cm were made, one in the 3rd intercostal space of the anterior axillary line and the other in the 5th intercostal space of the midaxillary line, and a 30°, 5-mm needle-type thoracoscopy was decided upon for the exploration of the thoracic cavity. The upper rib (the 2nd rib) is typically used as a marker point to find the T3-T4 sympathetic chain. Eighty-eight cases in the T3 group underwent T3 sympathetic chain + Kuntz fiber (bypass fiber) neurotomy, and 104 cases in the T4 group underwent T4 sympathetic chain + Kuntz fiber (bypass fiber) neurotomy. In order to entirely remove the traffic nerve bundle (Kuntz bundle), tissues of small size along the ribs (about 1.5 to 2.0 cm) were thermally ablated in both groups. After the surgery, the catheter was inserted and then pulled out after complete re-expansion of the lung, followed by a suturing of the incisions. The same procedure was performed on the other side. A chest X-ray was performed the first day after surgery to exclude the possibility of hemorrhage or pulmonary atelectasis.
Post operation follow-up
All cases were to be followed up by telephone after operation for more than 12 months. In total, 180 cases were followed up, and the follow-up rate was 93.8%. The content of the follow-up was as follows: (I) controlling of sweating after operation; (II) time and extent of post-operative sweating; (III) time, extent, and locations of compensatory hyperhidrosis.
Statistical processing
The χ2 test was used to compare the two groups (T3 versus T4) with SPSS 13.0 statistical software.
Results
Improvement of hand sweating and the occurrence of CH
The surgical success rate of both groups was 100%, and sweating was improved qualitatively after the surgery in all patients. There was no occurrence of severe complications during or after the surgery. Compensatory hyperhidrosis (CH) was the main non-severe postoperative complication.
The incidence rate of CH in the T3 group at 1 month, 6 months, and 12 months after surgery was 45.5%, 43.2%, and 34.1%, respectively. The rate in the T4 group was 46.2%, 38.5%, and 24.0%, respectively. While the incidence rates of CH in these two groups were comparable at 1 month and 6 months, the rate at 12 months was significantly lower in the T4 group than that in the T3 group (P<0.05). Hyperhidrosis can be classified into three categories based on severity (mild, moderate, severe), with varying negative impact on the patients’ life. Mild hyperhidrosis had a negligible impact on patients’ normal activities and daily life. Moderate hyperhidrosis reduced patients’ satisfaction of the surgery and had a noticeably negative impact on the patients’ daily life and emotional well-being. Severe hyperhidrosis posed a substantially negative impact on the patients’ life. There was no statistically significant difference between these two groups in the proportion of patients with mild and severe CH, while the proportion of patients with moderate CH was significantly lower in the T4 group compared to the T3 group (P<0.05). Details are shown in Table 2.
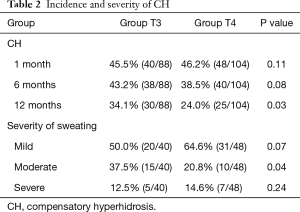
Full table
In addition to CH, non-severe pneumothorax was observed after the surgery in a small portion of the patients, and it could be managed with either thoracentesis or conservative treatment. Specifically, 5 patients developed unilateral pneumothorax as indicated by postoperative chest X-ray, and the pneumothorax was resolved with thoracentesis. Moreover, 2 patients developed a mild bilateral pneumothorax, which was resolved with conservative treatment (10).
Patients’ satisfaction and quality of life
In terms of postoperative satisfaction, the satisfaction rate in the T4 group was significantly higher than that in the T3 group (either very satisfied or satisfied, P<0.05). The incidence of palm dryness in the T4 group was also significantly lower than that in the T3 group (P<0.05). Patients in the T4 group had a significantly higher rate of armpit sweating than those in the T3 group (P<0.05). There was no statistically significant difference in the improvement of pedal sweating between these two groups (P>0.05). Details are shown in Table 3.
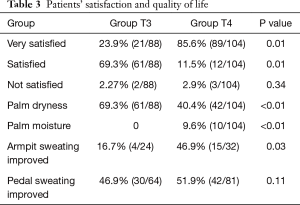
Full table
Discussion
Primary hyperhidrosis is characterized by abnormal hyperactivity of the sympathetic nervous system that controls the sweating glands in the hands. Such abnormal hyperactivity leads to the hypersecretion from the sweating glands, which usually becomes more severe when the patient is excited; however, its specific pathogenesis is still unclear (11). Although hand sweating has no significant impact on patients’ health, it poses a negative social impact on patients’ daily life, work, educational activities, and social interaction, which will severely impair the patients' emotional wellness. Therefore, there has been a strong desire to develop an effective and safe treatment for patients of the disease.
For many years, traditional conservative treatments like botulinum injections have been proven ineffective and have significant side effects. Endoscopic thoracic sympathectomy now is considered the only effective treatment for PH. It has been proven to be stable and persistent and has achieved very good curative effects and social benefits (12).
Current studies are mainly focused on the different cutting planes of T2-T4 of sympathetic nerve chains, all of which can effectively treat PH. However, the probability and extent of CH and the impact on patients’ life varies with the cutting plane. Traditional T2 sympathectomy may result in severe CH and palm dryness, so the numbers of patients who undergo such surgery are decreasing gradually (13).
In this study, we compared the effectiveness and safety of thoracoscopic sympathectomy with different cutting planes (T3 and T4) for the treatment of hand sweating. T3 or T4 sympathectomy was performed on patients who were divided into two groups, with one group receiving T3 and the other group receiving T4 sympathectomy. The success rates of surgery in both groups (T3 and T4) were 100%, and the sweating symptoms were qualitatively improved in all patients. There were no severe complications during or after the surgery, while the main non-severe postoperative complication was compensatory hyperhidrosis (CH). Currently, the mechanism of CH after video-assisted thoracic surgery (VATS) is still unclear, but the occurrence of compensatory sweating is closely related to the sympathetic chain cutting, which has an impact on the sympathetic nervous system (14). Some studies have shown that the sweating in other parts of the body after surgery is caused by the damage of the reflex arc between the sympathetic nerve and the hypothalamus during the surgery, which can result in sweating control disorder. The key to avoiding this is to retain as much tension in the sympathetic nerves of the head as possible. This is a convincing theoretical hypothesis for compensatory sweating, which has been confirmed by many clinical research studies (15).
Some studies have found that lowering the sympathetic cutting plane can reduce the incidence of compensatory hyperhidrosis. The study here shows that there was no statistically significant difference in the incidence of compensatory hyperhidrosis between these two groups at 1 month and 6 months, but the incidence rate in the T4 group was significantly lower than that in the T3 group at 1 year. Also, while there was no statistically significant difference in the incidence of mild or severe compensatory hyperhidrosis between these two groups, the incidence of moderate compensatory hyperhidrosis in the T4 group was lower compared to that in the T3 group. This indicates that while lowering the sympathetic cutting plane cannot reduce the incidence of short-term compensatory hyperhidrosis, it can reduce long-term CH.
The results also demonstrate that in these two groups, the remission rate of armpit sweating in the T4 group was higher than that in the T3 group, which indicates that the T4 sympathectomy is preferred for patients with armpit sweating. There was a statistically significant difference in the incidence of palmar moisture between these two groups, with a higher incidence in the T4 group than in the T3 group. Therefore, we would recommend T3 sympathetic chain cutting for the patients with severe hand sweating in order to reduce the incidence of palm moisture and to ensure treatment results.
In conclusion, thoracoscopic T3 and T4 sympathectomy are safe and effective methods for treating PH. Lowering the sympathetic chain cutting plane can reduce the incidence of long-term compensatory hyperhidrosis. For patients with excessive sweating, T4 sympathectomy is recommended, while for patients with severe hand sweating, T3 sympathectomy is recommended to ensure positive results of treatment.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The Ethics Committee of Hangzhou First People’s Hospital approved this study (NO.105-01 Ethics).
References
- Raposio E, Caruana G. Video-assisted Thoracic Sympathicotomy for the Treatment of Palmar and Axillary Hyperhidrosis: A 17-Year Experience. Surg Laparosc Endosc Percutan Tech 2015;25:417-9. [Crossref] [PubMed]
- Raposio E, Filippi F, Nordström RE, et al. Endoscopic transthoracic dorsal sympathectomy for the treatment of upper extremity hyperhidrosis: a new minimally invasive approach. Plast Reconstr Surg 1998;102:1629-32. [Crossref] [PubMed]
- Günal N, Ozpolat B, Dere Günal Y, et al. Single port thoracoscopic sympathectomy for primary palmar hyperhidrosis in adolescence. Turk J Med Sci 2014;44:79-83. [Crossref] [PubMed]
- Panhofer P, Ringhofer C, Gleiss A, et al. Quality of life after sympathetic surgery at the T4 ganglion for primary hyperhidrosis: clip application versus diathermic cut. Int J Surg 2014;12:1478-83. [Crossref] [PubMed]
- Liu Y, Yang J, Liu J, et al. Surgical treatment of primary palmar hyperhidrosis: a prospective randomized study comparing T3 and T4 sympathicotomy. Eur J Cardiothorac Surg 2009;35:398-402. [Crossref] [PubMed]
- Turkyilmaz A, Karapolat S, Seyis KN, et al. Comparison of T2 and T3 sympathectomy for compensatory sweating on palmar hyperhidrosis. Medicine (Baltimore) 2017;96:e6697. [Crossref] [PubMed]
- Li X, Tu YR, Lin M, et al. Endoscopic thoracic sympathectomy for palmar hyperhidrosis: a randomized control trial comparing T3 and T2-4 ablation. Ann Thorac Surg 2008;85:1747-51. [Crossref] [PubMed]
- Zhang W, Wei Y, Jiang H, et al. R3 versus R4 Thoracoscopic Sympathectomy for Severe Palmar Hyperhidrosis. Thorac Cardiovasc Surg 2017;65:491-6. [Crossref] [PubMed]
- Cameron AE. Selecting the Right Patient for Surgical Treatment of Hyperhidrosis. Thorac Surg Clin 2016;26:403-6. [Crossref] [PubMed]
- Silva SLD. Sobrinho, Fiorelli RKA, Morard MRS. Evaluation of the quality of life of patients with primary hyperhidrosis submitted to videothoracoscopic sympathectomy. Rev Col Bras Cir 2017;44:323-7. [PubMed]
- Wolosker N, Teivelis MP, Krutman M, et al. Long-Term Efficacy of Oxybutynin for Palmar and Plantar Hyperhidrosis in Children Younger than 14 Years. Pediatr Dermatol 2015;32:663-7. [Crossref] [PubMed]
- Panhofer P, Ringhofer C, Gleiss A, et al. Quality of life after sympathetic surgery at the T4 ganglion for primary hyperhidrosis: clip application versus diathermic cut. Int J Surg 2014;12:1478-83. [Crossref] [PubMed]
- Cheng A, Johnsen H, Chang MY. Patient Satisfaction after Thoracoscopic Sympathectomy for Palmar Hyperhidrosis: Do Method and Level Matter? Perm J. 2015;19:29-31. [PubMed]
- Cai S, Huang S, An J, et al. Effect of lowering or restricting sympathectomy levels on compensatory sweating. Clin Auton Res 2014;24:143-9. [Crossref] [PubMed]
- Thorlacius L, Gyldenløve M, Zachariae C, et al. Distinguishing hyperhidrosis and normal physiological sweat production: new data and review of hyperhidrosis data for 1980-2013. Int J Dermatol 2015;54:e409-15. [Crossref] [PubMed]


