
Lateral decubitus chest radiography or chest ultrasound to predict pleural adhesions before medical thoracoscopy: a prospective study
Introduction
Medical thoracoscopy (MT) is a diagnostic tool and the gold-standard to investigate undiagnosed pleural exudates effusion (1,2). It can be safely performed by pulmonologist under local or general anesthesia (3,4). Thanks to a rigid optical system, it is possible to explore the entire pleural cavity, to do fluid sampling and multiple biopsies of the parietal pleura and, if necessary, to perform pleural symphysis with pulverized talc under visual control (3,5). However, the major prerequisite is an easy access to the pleural space obtained by creating an artificial pneumothorax at the beginning of the procedure. The presence of dense pleural partitions can prevent access to the pleural space (6). The detection of such pleural adhesions prior to MT is necessary to locate the best pleural access point (6). Chest ultrasonography (CUS) recently gained popularity for the management of main pleural procedures including MT (6,7). For the latest, this imaging technique decreases the complications, mainly bleeding and failed procedure, by safely allowing the creation of the artificial pneumothorax and the choice of a pertinent point of entry for the pleural trocar (8,9). However, there are countries where the CUS technique is not available so far and where the pleural approach is only based on clinical examination and chest radiography. A recent prospective study aiming to assess the diagnostic accuracy of lateral decubitus chest radiography (LDCR) on the affect side before pleural maneuvers showed a positive predictive value (PPV) and negative predictive value (NPV) for the detection of pleural adhesions of 66.1% and 50% respectively (10). Therefore, this simple imaging technique can be useful in some cases in the area without any access to CUS procedures. However, to our knowledge, there is no study comparing LDCR and CUS. Therefore, we conducted a prospective study comparing these two procedures aiming to detect pleural adhesions before MT.
Methods
Study design and data analysis
During a period of 14 months, all consecutive patients, presenting a pleural exudate and for whom a MT was indicated for a diagnosis or a pleural symphysis, underwent a LDCR and a CUS before the procedure. The study was conducted in the Department of Thoracic Oncology, Pleural Diseases and Interventional Pulmonology in Marseille (France). Data acquisition and analysis were performed after the patients provided informed consent according to local policies and the approval of the local institute review board (North Hospital, Marseille, France). Collected data included demographics (age and gender), macroscopic fluid appearance, volume of fluid, radiography findings on LDCR (complete fluid layer from the diaphragm to the apex, incomplete/segmented fluid layer), CUS and thoracoscopy findings (free cavity or adhesions).
Pleural evaluation
LDCR
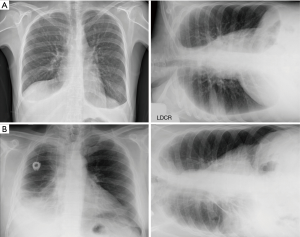
Radiographic evaluation on the affect side was performed the day before MT using a 125 kV (dose: 25 µGy/m2) Optimus 80 unit (Philips) with a 1.5 m film-focus distance for lateral decubitus views. The exposure was taken in inspiration with the central beam aimed at the lateral chest wall. The radiographic criteria were the thick density with complete (Figure 1A) or incomplete/segmented horizontal level (Figure 1B). Complete horizontal level from the diaphragm to the apex was supposed to illustrate free pleural cavity without pleural adhesion. The LDCR analysis was done by two senior physicians who did not perform the thoracoscopy procedures. In case of disagreement, a third one was asked for definitive scoring.
CUS
CUS was performed on the operating table before the MT using a general ultrasound machine (Philips) with a curvilinear probe with a frequency range of 2.5 MHz. Pleural effusion was measured checking the presence of internal echoes, septations and defining the optimal site for pleural access marked according to the operator.
MT
MT was standardized according to the current European practice as previously describe. Briefly, the procedure was done under mild sedation or general anesthesia after tracheal intubation with the patient in the lateral decubitus position on the healthy side and spontaneously breathing. An artificial pneumothorax was created on the table before the insertion of a 7-mm trocar to allow the introduction of a 0° telescope. The dedicated intercostal space for the procedure was decided according to the result of pre procedural assessment by CUS. A careful examination of the pleural cavity was done under visual control focusing on the presence of pleural adhesions, before pleural biopsies. MT was used as the gold standard for the detection of pleural adhesions.
Statistical methods
The statistical analyzes were performed using PASW Statistics version 17.0.2 (SPSS Inc., Chicago, IL, USA) and Vassar Stats statistical software. A value of P<0.05 was considered statistically significant. Comparisons were made using the chi-square test or Fisher's exact test (as appropriate) for the qualitative variables. The performance of radiographic signs (horizontal opacity with complete upper limit and regular or segmented) and ultrasound for the detection of pleural adhesions were evaluated using MT as a gold standard.
Results
Sociodemographic and clinical data
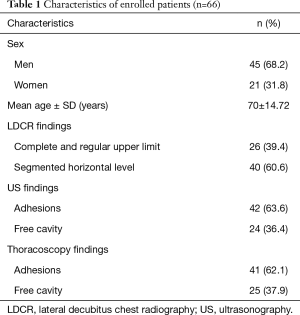
A total of 66 patients were included in the study with 45 men (68.2%) and 21 women (31.8%). The median age was 70 years (range: 29–87 years). The patients’ characteristics are collected in Table 1.
Full table
LDCR findings
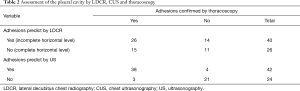
The chest radiography showed a measurable thick density with horizontal level in all patients, indicating the presence of pleural fluid. On lateral chest X-ray, opacity was horizontal with a complete and regular upper limit in 26 patients (39.4%) corresponding to a free pleural fluid effusion according to the pre-defined hypothesis. LDCR showed irregular and segmented horizontal level in 40 patients (60.6%), which we considered as multilocular pleural effusions with pleural adhesions. Table 2 summarizes these findings.
Full table
CUS findings
Ultrasound evaluation was performed using CUS showed pleural adhesions in 42 patients (63.6%). These pleural adhesions were limited in 61.9% of cases (n=26). Table 2 summarizes these findings.
MT findings
MT was performed in 59 patients (89.4%) with pleural effusion and in 7 patients (10.6%) with a hydro-pneumothorax. When the opacity was horizontal with a complete and regular upper limit on LDCR (26 patients), MT showed adhesions in 15 patients (57.7%). Among the patients with segmented horizontal level on LDCR (40 patients), the MT showed septa in 26 patients (65%). Table 2 summarizes these findings.
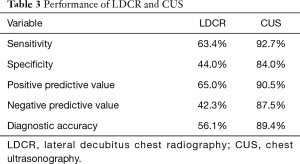
The sensitivity to predict adhesions on LDCR in case of segmented horizontal level was 63.4%, specificity 44.0%, PPV 65.0% and NPV 42.3%. The diagnostic accuracy of segmented opacity to predict pleural adhesions was 56.1%. Pleural adhesions found by MT were almost always (90.5%) previously significantly detect by CUS (P<0.001). The sensitivity of CUS to detect pleural adhesions was 92.7% (CI: 79.0–98.1%), the specificity 84.0% (CI: 63.1–94.7%), the PPV 90.5% (CI: 76.5–96.9%) and the NPV 87.5% (CI: 66.5–96.7%). The diagnostic accuracy of CUS in predicting pleural adhesions was 89.4%. Table 3 shows the performance of LDCR and CUS.
Full table
Discussion
The aim of this study was to evaluate and compare the performance of two imaging procedures (LDCR and CUS) to predict the presence of pleural adhesions with MT as a gold-standard to assess the pleural cavity taking into account that CUS is considered the best procedure to detect pleural septations in comparison to CT scan (11). Indeed, despite the increasing use of CUS for all the pleural maneuvers (11,12), there are some places where this technique is not already practice and the chest radiograph still remains the initial investigation of choice in patients with pleural disease (13). Thoracoscopy can be performed by both surgeons or interventional pulmonologist trained for this procedure. Some surgeons perform the procedure via video assisted thoracic surgery (VATS) under general anesthesia with single lung ventilation, which is not adequate for simple parietal pleural biopsies and a careful analysis of the pleural space. In this setting, uniportal VATS without intubation and MT are two techniques suitable to be performed under conscious sedation or local anesthesia. They both allow an access to the pleural cavity through a single incision during a non-intubated procedure. The main advantages of MT, using a 5 to 7 mm thoracoscope, are its safety and efficiency with an excellent diagnostic yield through a small point-of-entry. Therefore, the potential presence of pleural adhesions is crucial to predict before all diagnostic or therapeutic pleural maneuvers because of the increasing risk of chest bleeding, lung injury and sometimes the lack of access to the pleural cavity (14). The prediction of pleural adhesions is useful to choose the port site before a thoracentesis, a closed pleural biopsy or a thoracoscopy (15). To the best of our knowledge, this is the first study comparing the performance of LDCR and CUS to predict pleural adhesions.
According to our results, the accuracy of LDCR is lower than CUS evaluation of the pleural cavity. The LDCR data collected are similar to the data we found for a previous cohort including 86 patients which was the rationale of the current study (10). Again, the assumption that an incomplete/segmented horizontal level on LDCR being suggestive of pleural adhesions was not verified and the LDCR failed in this intent-to-diagnose pleural adhesion study. The MT findings regarding the presence of pleural adhesions were correlated with their detection at CUS examination (16). The segmented nature of the visible opacity on the LDCR was not associated with the presence of pleural adhesions at MT. Chest radiography was less sensitive and less specific than CUS for the diagnosis of pleural adhesions and NPV was also low. As a result, the CUS is higher than LDCR in the prediction of pleural adhesions at MT, which corroborates the literature data (17-22). Despite the limited number of patients enrolled in this study, the size of this cohort, the patients’ gender and the mean age of the patients remain representative and quite similar to other monocentric studies in particular in Korea (Seoul) (4) and Japan (23) with respectively 50 and 35 patients and a mean age of 66 years. Moreover, all patients presented a pleural effusion and this prospective study using for each patient the two preprocedural techniques to detect adhesion ruled out the need to take into account previous pleural procedures, mainly thoracenteses which therefore has no impact on the results.
Conclusions
CUS is superior to LDCR to detect pleural adhesion and consequently it is mandatory before all the pleural maneuvers. Before MT, CUS can be performed on the operating table to guide the choice of the pleural access. Lateral chest decubitus radiograph can remain in some situations an alternative to assess a pleural effusion. However, an educational program focusing the CUS practice is urgently mandatory for the teams aiming to develop a complete and safe management program for pleural diseases.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was approved by the local institute review board (North Hospital, Marseille, France) and written informed consent was obtained from all patients.
References
- Bhatnagar R, Corcoran JP, Maldonado F, et al. Advanced medical interventions in pleural disease. Eur Respir Rev 2016;25:199-213. [Crossref] [PubMed]
- Lakranbi M, Rabiou S, Ghalimi J, et al. The place of thoracoscopy in the management of thoracic pathologies: about 104 cases. Pan Afr Med J 2015;21:42. [Crossref] [PubMed]
- Schnyder JM, Tschopp JM. Thoracoscopie médicale. Rev Med Suisse 2011;7:792-4. [PubMed]
- Kim SJ, Choi SM, Lee J, et al. Medical Thoracoscopy in Pleural Disease: Experience from a One-Center Study. Tuberc Respir Dis (Seoul) 2017;80:194-200. [Crossref] [PubMed]
- Skalski JH, Astoul P, Maldonado F. Medical thoracoscopy. Semin Respir Crit Care Med 2014;35:732-43. [Crossref] [PubMed]
- Havelock T, Teoh R, Laws D, et al. Pleural procedures and thoracic ultrasound: British Thoracic Society pleural disease guideline 2010. Thorax 2010;65:ii61-76. [Crossref] [PubMed]
- Duncan DR, Morgenthaler TI, Ryu JH, et al. Reducing iatrogenic risk in thoracentesis: establishing best practice via experiential training in a zero-risk environment. Chest 2009;135:1315-20. [Crossref] [PubMed]
- Hallifax RJ, Talwar A, Wrightson JM, et al. State-of-the-art: Radiological investigation of pleural disease. Respir Med 2017;124:88-99. [Crossref] [PubMed]
- Psallidas I, Helm EJ, Maskell NA, et al. Iatrogenic injury to the intercostal artery: aetiology, diagnosis and therapeutic intervention. Thorax 2015;70:802-4. [Crossref] [PubMed]
- Thiam K, Berbis J, Laroumagne S, et al. Diagnostic Accuracy of Lateral Decubitus Chest Radiography before Pleural Maneuvers for the Management of Pleurisies in the Era of Chest Ultrasound. Respiration 2018;95:449-53. [Crossref] [PubMed]
- Wei B, Wang T, Jiang F, et al. Use of transthoracic ultrasound to predict pleural adhesions: a prospective blinded study. Thorac Cardiovasc Surg 2012;60:101-4. [Crossref] [PubMed]
- Williamson JP, Twaddell SH, Lee YC, et al. Thoracic ultrasound recognition of competence: a position paper of the Thoracic Society of Australia and New Zealand. Respirology 2017;22:405-8. [Crossref] [PubMed]
- Moffett BK, Panchabhai TS, Nakamatsu R, et al. Comparing posteroanterior with lateral and anteroposterior chest radiography in the initial detection of parapneumonic effusions. Am J Emerg Med 2016;34:2402-7. [Crossref] [PubMed]
- Ahmed M, Saka H, Ali Mohammadien H, et al. Safety and complications of Medical Thoracoscopy. Adv Med 2016;2016:3794-91. [PubMed]
- Havelock T, Tanikawa Y, Tsuboi R, et al. Masahiro Aoyama and Keiji Sugiyama. BTS guidelines. Thorax 2010;65:ii61-76. [Crossref] [PubMed]
- Sasaki M, Kawabe M, Hirai S, et al. Preoperative detection of pleural adhesions by chest ultrasonography. Ann Thorac Surg 2005;80:439-42. [Crossref] [PubMed]
- Marchetti G, Valsecchi A, Indellicati D, et al. Ultrasound-guided medical thoracoscopy in the absence of pleural effusion. Chest 2015;147:1008-12. [Crossref] [PubMed]
- Yousefifard M, Masoud B, Parisa GA, et al. Screening Performance Characteristic of Ultrasonography and Radiography in Detection of Pleural Effusion: a Meta-Analysis. Emerg (Tehran) 2016;4:1-10. [PubMed]
- Tsai TH, Yang PC. Ultrasound in the diagnosis and management of pleural disease. Curr Opin Pulm Med 2003;9:282-90. [Crossref] [PubMed]
- Qureshi NR, Rahman NM, Gleeson FV. Thoracic ultrasound in the diagnosis of malignant pleural effusion. Thorax 2009;64:139-43. [Crossref] [PubMed]
- Kiranantawat N, Sungsiri J, Geater SL. Outcome of ultrasound-guided small-bore catheter drainage in exudative pleural effusions. J Med Assoc Thai 2014;97:548-53. [PubMed]
- Corcoran JP, Tazi-Mezalek R, Maldonado F, et al. State of the art thoracic ultrasound: intervention and therapeutics. Thorax 2017;72:840-9. [PubMed]
- Miyoshi S, Sasada S, Izumo T, et al. Diagnostic Utility of Pleural Fluid Cell Block versus Pleural Biopsy Collected by Flex-Rigid Pleuroscopy for Malignant Pleural Disease: A Single Center Retrospective Analysis. PLoS One 2016;11:e0167186. [Crossref] [PubMed]


