From open surgery to uniportal VATS: asturias experience
Introduction
Single port major pulmonary resections are very popular worldwide and interest is growing in many thoracic surgery departments. It probably represents a less invasive approach to operate non-small cell lung cancer.
It has been proven to be a feasible and safe procedure when performed by surgeons experienced with double-port technique and anterior thoracotomy (1,2) but there is no evidence whether it is possible to perform a direct transition from posterolateral thoracotomy to the single port with as satisfactory postoperative results as with the transition from multiport technique.
In January 2012 a uniportal video-assisted thoracic surgery (VATS) program for major pulmonary resections was started at the Asturias University Central Hospital. This article presents the results of our learning curve period for uniportal VATS anatomical resections in a direct transition from open surgery to single-port. The focus of this study was to analyze and compare the results of our initial experience in direct transition from open surgery to uniportal VATS with the reference data from the results of the published best initial experience in the transition from multiport technique to uniportal VATS (3) in order to identify the feasibility and safety of this transition.
Patients and methods
We retrospectively reviewed the files of patients on whom anatomical pulmonary resection via uniportal VATS was attempted between January 2012 and January 2014 in the Department of Thoracic Surgery of Asturias University Central Hospital by the unique surgeon with VATS experience in the department, assisted by residents of thoracic surgery (4). The approval for this study was provided by the institutional ethical review board of the said hospital, and all patients provided written informed consent before operation.
Variables
We recorded: demographic data of patients, smoking habits, chronic obstructive pulmonary disease (COPD), presence of cardiopulmonary comorbidities, general characteristics of pulmonary lesions, preoperative FEV1, intraoperative findings, operative time, postoperative-drain-time, hospital-stay-time, successfully completed or converted to thoracotomy, intraoperative and postoperative complications and 30-day mortality.
The preoperative assessment according to the protocol of the tumor board routinely included: blood test, bronchoscopy, thoracic computed tomography (CT), and pulmonary function performed by spirometry or additional functional test in high-risk patients. PET-CT was made in cases of N2 suggested by CT. We made two groups of patients for analysis: A—patients operated on in the first year of experience (January 2012 to December 2012), and B—patients operated on in the second part of experience (January 2013 to January 2014).
As reference data, we select the results published in the largest case-series in uniportal VATS major resection (3).
Selection criteria
The indication criteria for uniportal VATS approach were the same as for open surgery except for lesions affecting chest wall or impossibility to extract without rib spreading.
Surgical technique
The patients were positioned in lateral decubitus as for posterolateral thoracotomy. The lung blockade was obtained using a double lumen tube and continuous suction is applied to the non ventilated bronchus. A 4-5 cm incision was made in the 5th intercostal space. Rib retractor was not used in any case. A wound protector is used in some particular patients. A 10 mm/30° camera was used for vision. Some specific Scanlan instruments (ref 9009-738SC, 9009-828, 9009-240, 9909-225, 9909-227, 9909-920, 9909-203) was used in combination with standard VATS instruments.
Following specific technical recommendations for uniportal VATS, the hilar vessels and bronchus were dissected and transected in a particular order using stapler devices (ECHELON FLEX™) and clips (Hem-o-lok®). Fissureless technique was applied if absent or uncompleted fissures were found. No section of pulmonary ligament was made in any case. A special bag was used for the extraction of the resected lobe. Mediastinal lymph nodes were dissected completely. The intercostal spaces were infiltrated with bupivacaine in all cases. A 24F chest tube was positioned through the incision in the upper part of the pleural space.
Statistical analysis
All the data are reported as mean, median or frequencies, with associated interquartile ranges (IQR), 95% confidence intervals (CI), and P values calculated. Categorical data, both nominal and ordinal, were compared between groups using Fisher’s χ2 (exact) test. A probability value of less than 0.05 was considered to be statistically significant. SPSS, version 20.0 (IBM Corp) was used for the statistical analysis.
Results
From January 2012 to January 2014, 82 uniportal VATS anatomical pulmonary resections were attempted in the department of thoracic surgery by a single surgeon. In the first part of the experience (January 2012-Dec 2012) 40 resections were attempted, of them 36 (90%) were completed by uniportal VATS. In the second part of experience (January 2013-January 2014) 42 resections were attempted and 40 (95.2%) were completed. Therefore, of the 82 resections attempted, 74 (90.2%) were completely carried out including: left upper lobectomy in 21 patients, left lower lobectomy in 18 patients, right upper lobectomy in 18 patients, middle lobectomy in 2 patients, right lower lobectomy in 12 patients, lingulectomy in 1 patient, middle & lower bilobectomy in 1 patient, and pneumonectomy in 1 patient.
The general characteristics in two groups were similar: the mean age was 61±14 for group A and 62±12 for group B. Mean FEV1 was 87±19 for group A and 85±19 for group B.
Of 82 patients, 76 (92.6%) were selected for resection because of a diagnosis of non-small lung cancer.
One third of patients could be considered to be relatively complex case for an initial program of VATS because of: strong pleural adhesion in 25 (30.4%) cases, silicoanthracotic adherent lymph nodes in 26 (31.7%) cases, incomplete or fused fissures in 26 (31.7%) cases, pneumoconiosis in 16 (19.5%) cases, tumor size larger than ≥5 cm in 10 (12.1%) cases, preoperative global FEV1 less than 50% in 4 (4.8%) cases.
The mean surgical time during the learning curve was 211 min for group A and 150 min for group B (Table 1).
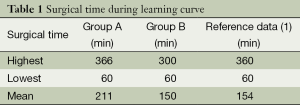
Full table
The median drain-time and hospital-stay-time were 3 and 4 days for the first year of experience, 2 and 3 days for the second year of experience respectively. In the multivariable analysis we identify pneumoconiosis and level of training as significant factors for higher operative and postoperative time.
Comparisons between multiple variables with drain-time and hospital-stay-time are described in Table 2.
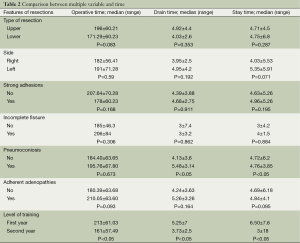
Full table
The most frequent intraoperative complication was bleeding in 10 (12.1%) patients (Table 3) but only 2 patients of group B had this complication. Conversion was required in 6 patients of group A and 2 patients of group B. Of the 82 patients 23 (28%) had some minor postoperative complication. Of these, chest tube reinsertion was the most frequently observed in ten patients of group A but only two patients of group B because a decreased incidence of postoperative residual pleural effusion (Table 4). There were 3 (3.65%) major complications, all of them in group B. In this group there were two perioperative deaths: (I) a right upper bilobectomy for a 5 cm long tumor in a 76-year-old man with preoperative FEV1 of 42% because of a pneumoconiosis with massive pulmonary fibrosis (the poorest pulmonary function in this study population) who died of respiratory failure on the 12th postoperative day. This patient was one of the four conversions to thoracotomy because of technical difficulties. (II) a left upper lobectomy in a 76-year-old man with high cardiovascular risk because of a triple coronary bypass, and previous right upper lobectomy with simultaneous left upper lobe wedge resection with adjuvant chemotherapy and radiotherapy treatment for synchronous lung cancer, with limited pulmonary function (preoperative FEV1: 70%) who died the day he was discharged from hospital after an optimal recovery because of a neurologic cause on the 8th postoperative day.
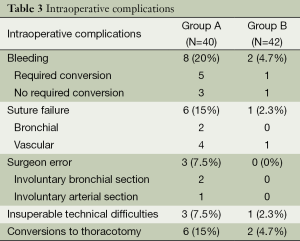
Full table
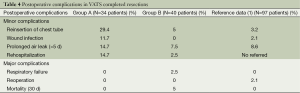
Full table
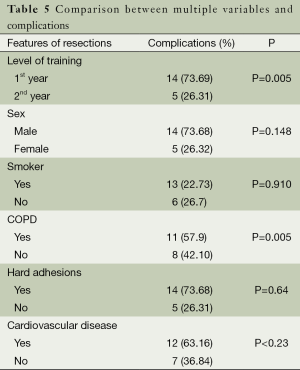
Relations between multiple variables with complications are outlined in Table 5.
Full table
Discussion
Single-port major pulmonary resections are very popular worldwide and interest is growing in many thoracic surgery departments. It probably represents a less invasive approach to operate on non-small cell lung cancer.
This technique has been proved to be a feasible and safe procedure when performed by surgeons experienced with double-port technique and anterior thoracotomy (1-3) but probably that particular experience is not really necessary to start a uniportal VATS program. We have hypothesized that a uniportal VATS program for major resections could be started with similar recommendations published by Petersen for a multiport VATS program (5,6): 1—large experience in open lobectomy; 2—experience in performing more than 100 minor VATS procedures; 3—attendance at formal courses in VATS lobectomy; 4—selection of the patients; 5—introduction of the element of resection step-by-step; and 6—making a prospective data collection.
A uniportal VATS program was implemented at Asturias University Central Hospital, in a direct transition from posterolateral thoracotomy by a single surgeon very experienced in posterolateral but not in anterior approach for open lung resections.
The analysis of data shows several differences between group A and B in terms of surgical time, postoperative drain time, hospital-stay-time, minor and major complications. Indeed, mean surgical time was reduced after the 40 first cases (group B) by 61 min. In a similar way, the median of postoperative drain time and hospital stay time was reduced by 1 day. Therefore, group B had similar postoperative outcomes to patients in the reference studies in those particular items. Minor complications in group B were also similar to the reference study except for a small increase rate in patients requiring reinsertion of chest tube (5%/3.2%). Major complications were found in 3.6% of patients but only in group B including two cases of 30 d-mortality in this group. In our study we included a considerable amount of relatively complex cases for initial VATS program. We found this reason responsible for increased rates of complications in both groups. Additionally, in the multivariable analysis, we found COPD and the level of training as the only significant factors for complications (P=0.05).
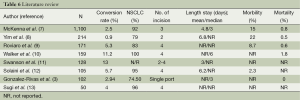
The results of the second part of our experience are in concordance to results of others authors and reference data except for 30 d-mortality (Table 6). However we found these deaths associated with an inadequate selection decision more than with a technique-related cause, because of an overestimation of the benefits of the technique in these patients. As a result, we consider that patient selection is crucial to prevent complications.
Full table
From the results of group B of patients we may consider that our learning curve from open surgery to uniportal VATS has required 40 resections. This is very similar to that reported for multiport technique (5,6). In this period of time we had no major complications and a very assumable rate of minor complications, so we found this transition feasible, safe and concordant with the transition from open surgery to multiport technique if patients are properly selected.
Our study has several limitations. Indeed, this is a small, retrospective and descriptive study of a single-surgeon’s practice. Reference data used for comparison include the global results of the two first years of experience. This can lead to underestimate the particular results of the second year of experience in comparison with our group B of patients.
Conclusions
Direct transition from open surgery to uniportal VATS for major pulmonary resections has been in our experience feasible and safe with good results. We founded this approach may be closer to conventional operation technique as compared to traditional thoracoscopic technique. It is probably important that the surgeon has to be very experienced in open resections and has completed more than 100 minor VATS procedures. Specific training courses with experts and proper patient selection process are also necessary. The number of procedures necessary to obtain appropriate experience may be similar to those reported for transition from open surgery to multiport technique. It is recommendable to be conscious that conversion to thoracotomy at the correct time during learning curve indicates prudence not failure. Until there are other similar experiences, our results should be interpreted with caution.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Gonzalez-Rivas D, Fernandez R, de la Torre M, et al. Thoracoscopic lobectomy through a single incision. Multimed Man Cardiothorac Surg 2012;2012:mms007.
- Gonzalez-Rivas D, Paradela M, Fieira E, et al. Single-incision video-assisted thoracoscopic lobectomy: initial results. J Thorac Cardiovasc Surg 2012;143:745-7. [PubMed]
- Gonzalez-Rivas D, Paradela M, Fernandez R, et al. Uniportal video-assisted thoracoscopic lobectomy: two years of experience. Ann Thorac Surg 2013;95:426-32. [PubMed]
- Aragón J, Pérez Méndez I. First Case Report of Single Port Video-Assisted Thoracoscopic Middle Lobectomy for the Treatment of Pulmonary Aspergilloma in a Pediatric Patient. European J Pediatr Surg Rep 2013;01:012-014.
- Petersen RH, Hansen HJ. Learning curve associated with VATS lobectomy. Ann Cardiothorac Surg 2012;1:47-50. [PubMed]
- Petersen RH, Hansen HJ. Learning thoracoscopic lobectomy. Eur J Cardiothorac Surg 2010;37:516-20. [PubMed]
- McKenna RJ Jr, Houck W, Fuller CB. Video-assisted thoracic surgery lobectomy: experience with 1,100 cases. Ann Thorac Surg 2006;81:421-5; discussion 425-6. [PubMed]
- Yim AP, Liu HP. Thoracoscopic major lung resection--indications, technique, and early results: experience from two centers in Asia. Surg Laparosc Endosc 1997;7:241-4. [PubMed]
- Roviaro G, Rebuffat C, Varoli F, et al. Videoendoscopic pulmonary lobectomy for cancer. Surg Laparosc Endosc 1992;2:244-7. [PubMed]
- Walker WS, Codispoti M, Soon SY, et al. Long-term outcomes following VATS lobectomy for non-small cell bronchogenic carcinoma. Eur J Cardiothorac Surg 2003;23:397-402. [PubMed]
- Swanson SJ, Herndon J, D’Amico A, et al. Results of CALGB 39802: feasibility of video-assisted thoracic surgery (VATS) lobectomy for early stage lung cancer. Proc ASCO 2002;21:290a.
- Solaini L, Prusciano F, Bagioni P, et al. Video-assisted thoracic surgery major pulmonary resections. Present experience. Eur J Cardiothorac Surg 2001;20:437-42. [PubMed]
- Sugi K, Kaneda Y, Esato K. Video-assisted thoracoscopic lobectomy achieves a satisfactory long-term prognosis in patients with clinical stage IA lung cancer. World J Surg 2000;24:27-30; discussion 30-1. [PubMed]


