Anxiety and depression—Important psychological comorbidities of COPD
Chronic obstructive pulmonary disease (COPD) is a chronic lung disease that has significant extrapulmonary effects that may impact the severity of symptoms in individual patients. COPD is a highly prevalent disease worldwide. The prevalence is variable between countries, but overall there is a prevalence rate of around 10% in individuals aged 40 and above (1). In developed countries, COPD is responsible for approximately 4% of all deaths and is the only major condition for which the burden of disease continues to increase, currently being 5th overall in underlying cause of death and 3rd for burden of disease (2).
Anxiety and depression are well-recognized major comorbidities in COPD (3), and consequently there has been a surge in clinical and research interest in reducing the negative impact of these important comorbidities in patients with COPD (4). This review provides an overview of the pathophysiology associated with anxiety and depression in COPD patients, the prevalence and impact of these comorbid conditions, and the strategies for their diagnosis and treatment. Areas of need for future research are also highlighted.
Prevalence of anxiety and depression as comorbidities in COPD
Like other major chronic diseases, COPD has a significant impact on psychological well-being of people affected. Patients with COPD have a higher prevalence of depression and anxiety than the general population (5) and COPD patients have relative risk of 1.69 of developing depression (6). The rates of both anxiety and depression may even be more prevalent among COPD sufferers compared with other chronic diseases (7).
The reported prevalences of each condition are quite varied, depending on the population surveyed and the tools used to assess depression and anxiety. For patients with stable COPD in primary care settings or respiratory clinics, the prevalence of depression varies widely from 10% to 57% (5,8), and for anxiety, prevalence ranges from 7% to 50% (5,9).
Risk factors for increased rates of depression include living alone (10) and gender. Females have a higher rate of both anxiety and depression (11-13), and rates of depression are more strongly correlated with severity of dyspnoea as compared with males (12). Increasing severity of COPD is associated with higher rates of depression and anxiety (14,15); for example, in patients requiring long-term oxygen, 57% were found to have depressive symptoms and 18% had depression classified as severe (16). End-stage COPD patients undergoing palliative care also have high rates of anxiety and depression (7).
Other important risk factors are patients that have been hospitalized for an exacerbation of COPD or recovering from an exacerbation (17,18), severity of respiratory symptoms especially dyspnoea (19), living alone, and severe impairment of physical functioning (9,10).
Pathophysiological mechanisms for anxiety and depression in COPD
The aetiology of the association between depression and COPD is not fully understood; however the relationship is complex and interactive. The most important risk factor for COPD is smoking. Smoking and depression have a bidirectional interaction. Depressed individuals are more likely to smoke (20), display higher risk to commence smoking (21,22), and find smoking cessation more difficult (20,23). Conversely, smokers are more likely to be depressed (24), which could be caused by activation of nicotinic acetylcholine receptors (25), or direct inflammatory effects of smoking (26).
Although smoking could have some part to play as a causative factor for depression, depression is still more prevalent among COPD patients than smokers without COPD (13). A possible mechanism could be related with ‘overspill’ of local lung inflammation in the circulation (26,27). It has been speculated that systemic inflammation may play a role in the presence of depression (28). Although there are difficulties in quantification of inflammatory markers in the ‘overspill’ theory (26), sTNFR-1 has shown a strong association with rates of depression in COPD patients (27), while TNF-α has shown conflicting results (28,29). It is not clear if the presence of systemic inflammation has a causative association with depression or that it is a marker a specific COPD phenotype; such as frequent exacerbators (27).
Hypoxia is an additional factor that may play a role in the development of depression in COPD. Low arterial oxygen saturation has been shown to be associated with periventricular white matter lesions (30), which are present in patients with depression (31). However, the significance of these findings is contentious since the localization of subcortical hyperintensity in depressed patients has been found to be variable due different imaging technologies, lesion definition and measurement techniques (31,32).
Although smoking, inflammation and hypoxia have potential impact on the prevalence of depression in COPD, the strongest predictors of depression among patients with COPD are their severity of symptoms and reported quality of life (13). Functional limitations have been similarly shown to mediate depression in other disorders such as arthritis and heart failure (33). The amount of perceived instrumental support (the need of assistance for activities of daily living) among COPD patients has also been shown to be correlated with depression (34).
Several theories have been proposed to explain the overlap of anxiety and panic attack symptoms with COPD (35). Hyperventilation is defined as the exaggerated breathing in excess of metabolic need, causing lowering pCO2 and causing respiratory alkalosis (36,37). This pattern of breathing can cause dyspnoea in healthy individuals and consequently panic attacks in those predisposed patients (37).
In panic disorder patients it is possible to evoke symptoms of dyspnoea and chest pain when infusing lactate or inhaling excessive CO2 (37). These findings are the basis of the carbon dioxide hyperventilation model (35). Areas of the brain with intrinsic CO2/H+-sensitive neurons such as the ventrolateral surface of the medulla and locus coeruleus are involved in ventilation, but also play role in panic behaviours. The activation of these areas may concomitantly activate a defensive behavior and precipitate a panic attack (37).
Another important theory is the cognitive behavior model which is based on the principle that normal bodily sensations are misinterpreted by patients with panic disorder and can consequently cause a panic attack (35). This misinterpretation may be associated with a behavioural sensitization event (trauma), since 20-30% of healthy panic disorder patients had a near-drowning or suffocating past experience (37). COPD patients are at greater risk of a traumatic event caused by an exacerbation, which may lead to an increased risk of developing panic disorders.
The pathophysiology of anxiety and depression among COPD patient is complex and poorly understood. Patients with depression and anxiety are at higher risk of developing COPD due to smoking. Likewise the physical, emotional and social impact of COPD is correlated with development depression and anxiety. This complex interaction between COPD and mental health diseases may cause a self-perpetuating cycle that has a severe impact upon a patient’s well-being.
Impact of depression and anxiety on COPD
Depression and anxiety have considerable impact on patients with COPD, in terms of associations with mortality, exacerbations and quality of life.
Effect on mortality
Among COPD patients, depressive symptoms are associated with increased mortality among hospitalized (18,38) and community patients (15,39-41). Some studies of COPD patients have shown an association of anxiety with increased mortality (18,38,42), whereas others have failed to show any association (41). A recent meta-analysis demonstrated that in COPD patients, comorbid depression and anxiety were associated with increased risk of mortality with relative risks of 2.29 and 1.27 respectively (6).
Importantly, a prospective study by Divo and colleagues, from the BODE cohort, has demonstrated that anxiety among female COPD patients was associated with a significant increase in mortality, with a hazard ratio of 13.76 which was more than the risk conferred by coronary heart disease, heart failure, or lung cancer (43). The potential causes of this increased mortality with anxiety are probably multifactorial. One factor is treatment compliance; for example, patients with depression are more likely to not complete rehabilitation (44,45). A meta-analysis has showed that patients with depression and anxiety symptoms are 3 times more likely to be non-adherent to their prescribed medications (46). Alternatively, anxiety may be secondary to the severity of the underlying COPD, and could therefore be a clinical marker of disease severity and risk of death.
Effect on exacerbations
Among COPD patients, exacerbations contribute significantly to morbidity and mortality (47). A systematic review of 20 studies has shown that depression and anxiety increases the risk of hospitalization for COPD patients (48). A meta-analysis by Laurin et al. showed that the relative risk of in-hospital treated COPD exacerbation was 1.12 for depression and 1.18 for comorbid depression and anxiety (49). Anxiety and depression symptoms were also associated with increased length of stay in hospital for COPD exacerbations (18,50,51).
There are multiple possible links between depression and anxiety, and increased rates of COPD exacerbation. The impact of symptoms of depression and anxiety could place patients at risk due to non-adherence with treatment (46,52), and suboptimal success with smoking cessation (18,49). Depression could have direct effects by impairing the immune system and consequently predisposing to infections (53) leading to increased frequency of exacerbations. Worsened perception of dyspnoea may lead patient to seek medical attention unnecessarily and increase hospital admissions; patients with anxiety and depression during admission have worse dyspnoea scores despite having less severe physiological parameters (e.g., pH, partial pressure of oxygen and carbon dioxide) (54). The meta-analysis by Laurin et al. has shown that patients with anxiety were at greater risk for exacerbations that required treatment in the community, whereas those with depression were at higher risk for exacerbations requiring treatment in hospital (49). This discrepancy could be explained by “early intervention” among anxious patients that could prevent the need for treatment in hospital (49).
Effect on quality of life
The detrimental impact of COPD on quality of life is well-documented (3). Depression and anxiety symptoms also have significant impact on quality of life and functional status in many chronic diseases (55,56). In general, patients with depression and anxiety perceive their health as poorer than the average population (57). Specifically for COPD, the impact of quality of life and functional status is also evident in several studies, independent of the severity of COPD or related comorbidities (14,56,58-62). A meta-analysis showed that the presence of depression and anxiety among COPD patients was one the strongest correlations with self-reported health status (63). Comorbid depressive symptoms in patients with COPD are associated with persistent smoking, increased symptom burden, poorer physical and social functioning (18), and difficulty in performing daily activities (64). Low self-confidence or self-efficacy is also common, which may lead to worsened ability to cope with chronic disease (49,56).
Depression and anxiety symptoms are associated with increased perception of dyspnoea (54,65,66). The presence of psychological symptoms (mainly depression and to lesser extent anxiety) has an effect on vital exhaustion, defined as a state characterized by fatigue and lack of energy, worsening irritability and feelings of demoralization (67). Fatigue and especially dyspnoea are independently negatively associated with poor health status (63,68).
The impact of depression and anxiety symptoms are not limited to an individual’s lung disease. The presence can influence a person’s end of life decisions (69) or may have negative impact upon partners and their respective relationships (70).
Diagnosis and screening of depression and anxiety
The gold standard for the diagnosis of depression or anxiety is based in the criteria listed in the DSM-IV and achieved through structured interviews performed by a psychiatrist or a clinical psychologist. As there is a strong positive relationship between self-reported severe symptoms and the existence of a mental disorder (71,72), screening instruments have also been developed, which are less costly, faster and easier to administer. These instruments can also monitor clinical outcomes of mental health treatments (73,74).
Several screening tools have been validated for use in COPD patients. The Geriatric Depression Scale and its 15-item short form (GDS-15) are validated as depression tools (75), and the Hospital Anxiety and Depression Scale (HADS) and the Geriatric Anxiety Inventory (GAI) have been validated for anxiety in COPD patients (76). Anxiety Inventory for Respiratory (AIR) Disease and Brief Assessment Schedule Depression Cards (BASDEC) are two other scales that have been developed exclusively for COPD (9,77).
There are concerns regarding the use of screening instruments due to the risk of false positives caused by the overlap of symptoms (78), and the uncertainty regarding impact on routine practice (79,80). The Global Initiative for Chronic Obstructive Lung Disease guidelines recommend that new COPD patients should have a detailed medical history including for depression and anxiety (3). However, to date, there is no consensus on the most appropriate screening approach for anxiety and depression (81).
Treatment approaches for anxiety and depression in patients with COPD
Depression and anxiety, when coexisting with COPD, significantly impact quality of life and functional outcomes. In acknowledgement of the biopsychosocial impact of chronic ill health, the World Health Organization has stated that patients with chronic diseases such as COPD should receive integrated care programs which are centered on the patient rather than just the disease (82). Fortunately, interventions targeting these psychological comorbidities are well-established for the general population (83). However psychological care guidelines are less well developed for the specific COPD patient population (84). Where psychological treatments have been used in COPD, these have typically been based on guidelines already in use for depression and anxiety in the wider population (85). Treatments can be divided into psychological [relaxation, cognitive behavioural therapy (CBT), self-management] and pharmacological interventions. Pulmonary rehabilitation, a specific treatment for COPD, also has beneficial effects on anxiety and depression.
Psychological therapies
For patients with a chronic health condition who are also experiencing clinical or sub-threshold depression, the UK’s National Institute for Health and Care Excellence (NICE) recommends use of low to high intensity psychosocial interventions depending on the severity of mood symptoms (85). Low intensity interventions may include individual or self-help programs, or online CBT, while high intensity interventions are typically individual or group CBT sessions. These recommendations are based on moderate quality randomized controlled trials and the experience and opinion of the Guideline Development Group (85). While the NICE guideline targets general chronic health presentations, good quality studies are somewhat lacking in COPD-specific populations. Existing studies show mixed results that are difficult to compare, because of factors such as small sample size, varied populations, lack of data on disease severity and differences in the screening tools used to assess these patients. A recent meta-analysis has described the benefits of the most common psychological interventions—relaxation therapy, CBT and self- management education programs (83).
Relaxation therapy
The aim of relaxation therapy is to promote psychological change through techniques that create a relaxed state. Techniques commonly used range from breathing exercises, hypnoses, meditation, body positioning, sequential muscle relaxation, mild forms of exercise and visualization techniques (86). These methods are used separately or as a element of other psychological treatments or pulmonary rehabilitation (4).
The effectiveness of relaxation-based therapies for COPD was evaluated in a meta-analysis by Devine et al., which showed significant improvements in symptoms of dyspnea and anxiety (87). For patients undergoing a pulmonary rehabilitation program, progressive relaxation techniques administered by tape-recorded classes showed a non-significant improvement in depression and, to a lesser extent, anxiety symptoms at the time of the end of the pulmonary rehabilitation program (88). There have been several smaller studies that have investigated other types of relaxation approaches. One small study using tai chi demonstrated a non-significant improvement of depression, dyspnoea and physical capacity as measured by six minute walk test results (89). A study examining yoga as the intervention showed a significant improvement in six minute walk results and functional performance, non-significant improvement in dyspnoea score and quality of life, but no change in anxiety or depression scores (90). In these types of studies, it is often difficult to determine whether the benefit is due to the physical activity or the relaxation components of the treatment.
Loosely related to relaxation interventions, singing classes have also been used as an intervention in COPD patients. The underlying theory is that singing lessons might improve patient quality of life and/or functional status by offering techniques that address both the sensory component of dyspnoea (e.g., control of respiratory pattern to reduce hyperinflation) and the affective component (e.g., anxiety and low mood around perceived breathlessness) (91). A moderate-sized study employing singing classes showed improvement in anxiety levels and the physical component of a quality of life questionnaire (92). In a further study by the same researchers, the improvements remained after controlling for the incidental beneficial effects of social interaction amongst the participants (93). In regards to these less traditional interventions, there is still a lack of clarity about their applicability, their long-term effectiveness, the active component (physical or psychological), and how they may be incorporated into standard care.
Cognitive behavioural therapy (CBT)
CBT is a type of psychotherapy used in the management of a range of psychiatric disorders. It is based on an information-processing model in which emotional symptoms are thought to be driven by negatively-biased evaluations of the world, the future, or the self (including bodily sensations) (94). Often performed in collaboration between the therapist and the patient, CBT utilizes a number of strategies to correct those biased evaluations and provide skills aimed at controlling their symptoms and consequently improving the management of their illness (4).
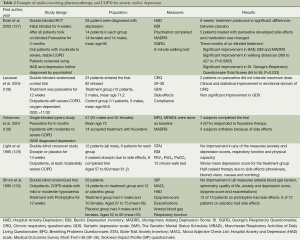
The use of CBT has gained traction because of its effectiveness in achieving symptomatic relief for patients with chronic illnesses (56,95). There have been numerous studies of varying quality and sample size that have shown promising results (96-101) (Table 1). The studies showed small to moderate improvements in anxiety and depression scores and quality of life; however direct comparison is hampered by the fact that interventions varied in regard to number of sessions, duration of each session and delivery format (group or face to face). The fact that positive impact was demonstrated in most studies, even those with shorter interventions, holds promise for future applicability.

Full table
Cost-effectiveness is undoubtedly an important issue, particularly given tightening health budgets, and increasing service imperatives to reduce health care spending. One study has shown that face-to-face CBT is effective and also may be cost neutral when implemented in COPD patients (95). If other less expensive approaches are interchangeable to face-to-face they may be more economically attractive. The use of telephone-based interventions for depression has shown to be just as effective as face-to-face (102-104), and such an approach has also been shown to be beneficial for patients with anxiety and depression associated with other chronic diseases (105,106). A novel alternative approach is the use of an Internet-based intervention, which has been shown to be as effective as face-to-face interventions for depression and anxiety (107-109). CBT-based therapies, particularly tightly manualised therapies for sub-clinical anxiety or depression, may not require a fully trained psychologist for its administration, adding to overall cost effectiveness. A nurse-administered minimal psychological intervention (MPI), based on the principles of CBT and self-management, was used in one study of COPD patients and showed promising results (110).
Not all aspects of CBT therapy may be necessary to produce a therapeutic effect. Purely behavioural interventions can be as effective as CBT for patients with depression (111). They are simpler to administer and theoretically could be used for patients with COPD.
Self-management strategies
Self-management programs aim to improve patient care by providing resources and guiding health behaviour change in ways that empower the individual. This empowerment is thought to increase their ability to carry out medical regimens designed to control their chronic disease, improve well-being and decrease exacerbations (112-114). Many self-management programs incorporate aspects of CBT.
The effects of self-management programs for patients with chronic health conditions are still unclear, and the results have been modest when compared to more specific psychological interventions (83). Jonker et al. found improvement in self-efficacy in older people, but no reduction in health care utilization or improvement in quality of life (112). In cardiac patients one study reported a moderate effect of self-management on functional outcomes and depressive symptoms after an acute coronary syndrome (115). For COPD patients, although a review by Kaptein et al. reported favourable outcomes for self-management on frequency of hospitalisation, greater exercise tolerance and increased quality of life (116), in the meta-analysis of 29 RCTs by Coventry et al., there was no overall benefit for self-management education alone for anxiety and depression in COPD (83).
A large multicenter randomized trial in COPD patients showed that a self-management intervention reduced exacerbation rates (114). Similarly, a Cochrane review by Effing et al. (113) showed a significant and clinically relevant reduction in the number of patients with one or more hospital admissions and a small but significant reduction of dyspnoea scores. Results were inconclusive for anxiety and depression symptoms, doctor and nurse visits, the use of courses of oral corticosteroids and antibiotics, and the use of rescue medication. No effects were seen for ER visits, lung function, exercise capacity, and days lost from work (113). Interestingly, conflicting results for quality of life questionnaires were seen, as a positive trend was seen for the St. Georges Respiratory Questionnaire (SGRQ), but not for SF-36 (113). This last result highlights the need for precision and clarity in the description of the construct being measured (e.g., quality of life) and consistency in the selection of measures. The wide range of measures used across the papers surveyed herein reveals the difficulty in both assessing the effectiveness of interventions within a study, and comparing findings across studies reported in the literature.
Finally, health mentoring is a self-management intervention that uses cognitive behavioural techniques to provide skills to improve self-efficacy and disease management, and to change unhealthy behaviours (117). Nursing-based mentoring has shown conflicting results with one study showing benefit in quality of life for patients with COPD (118), while other studies have failed to show any positive effect on quality of life (119,120) or anxiety and depression symptoms (119). A meta-analysis has shown case management was the least effective intervention for reducing anxiety and depression when compared to CBT, relaxation or self-management intervention (83).
Pharmacotherapy
Pharmacotherapy is a mainstream treatment for anxiety and depression. Although there is some controversy regarding effectiveness, meta-analyses have shown the overall benefit of pharmacotherapy in the treatment of anxiety and depression (121). In standard clinical practice, antidepressants are the main medication used for depression and anxiety. Other less common agents used are benzodiazepines, antipsychotics, anticonvulsants and azapirones (4).
Antidepressants work mainly by increasing synaptic monoamines, dopamine, serotonin and/or noradrenaline. They have similar effectiveness but mainly differ based on type and severity of side effects. The main categories are: selective serotonin reuptake inhibitors (SSRIs), serotonin and noradrenaline reuptake inhibitors (SNRIs), noradrenaline reuptake inhibitors, tetracyclic antidepressants, tetracyclic analogues of mianserin [sometimes called noradrenergic and specific serotonergic antidepressants (NaSSA)], tricyclic antidepressants (TCAs), reversible inhibitors of monoamine oxidase A (RIMAs), monoamine oxidase inhibitors (MAOIs) and melatonergic antidepressants [summarised in (122)]. Antidepressants are a moderately effective treatment for depression in healthy individuals, more so in cases of greater severity and in melancholia, but there is less certainty in physically ill patients. Among this population with subthreshold symptoms of depression (symptoms that are below the DSM-IV criteria for major depression) or mild to moderate depression, NICE guidelines advice that antidepressants should not be routinely prescribed (72).
A recent Cochrane review of antidepressants (mostly SSRI and TCA), for the treatment of depression or depressive symptoms among physically ill patients, demonstrated a significant improvement among patients with depression or milder depressive disorder, and a positive trend for depressive symptoms and other depressive disorders (123). This Cochrane review also observed that there was greater long-term improvement for SSRIs compared to TCAs. A study assessing the effects of the SSRI, fluoxetine, in hospitalized patients with depression showed a positive trend towards improvement of depression symptoms specially for those patients that were more severely ill (124).
In contrast to the wider general population or physically ill, at present, the data for efficacy of pharmacotherapy for anxiety and depression are limited for COPD. The main studies have been of SSRIs and TCAs. SSRIs are the first line pharmacotherapy treatment for depression and anxiety (125). For depression, small studies in COPD have shown mild improvements. Two studies of COPD patients using paroxetine showed variably significant improvement in quality of life questionnaires (126,127), and improvement of anxiety and depression scores and physical capacity after 3 months (127) (Table 2). A single-blinded open trial study of 57 COPD patients, aiming to assess the acceptability of fluoxetine therapy, showed that over two-thirds of patients declined to use fluoxetine therapy, mostly related to patient biases regarding use of psychiatric medication (128) (Table 2).
Full table
For TCAs, a number of small studies have been conducted in COPD. A study by Borson et al. showed that nortriptyline was effective in reducing depressive and anxiety symptoms and in increasing physical function (131), although a crossover study of similar size failed to show any benefit when using doxepin for patients with symptoms of anxiety and depression (129). In another study using protriptyline, the majority of the patients did not complete the trial because of the anticholinergic side effects (130). TCAs are no longer first line treatment for depression or anxiety, and consequently future trials for this medication class are unlikely (132).
Regarding the treatment of anxiety in COPD patients, a Cochrane review was unable to undertake any meta-analysis due to poor quality of the studies and very small sample sizes (122). Only four studies were analyzed, with two studies using SSRIs, and the other two using a TCA and azapirones. Two studies using SSRI showed a non-significant reduction in anxiety symptoms (122,127). The studies using TCA and azapirones did not show any improvement (129,133).
As was the case for psychological treatment, the overall effectiveness of pharmacotherapy for anxiety or depression in COPD has not been rigorously tested. Studies in COPD have been small, with large heterogeneity of sampling and tools used to assess efficacy of the treatments. In addition, there is limited evidence regarding the impact of side effects of pharmacotherapy, such as dry mouth and sexual dysfunction (123). Some side effects of treatment (such as dry mouth) may compound adverse effects of medications used for COPD, notably the anticholinergic activity of long-acting muscarinic antagonists (134). In addition, there are issues regarding patient refusal to take antidepressants due to misconceptions regarding depression and addiction, stigma associated with the disease, and lack of interest and motivation (132). Clearly, much more work needs to be done to test pharmacotherapy for anxiety and depressive symptoms in COPD, and to undertake head-to-head comparisons with psychological interventions and combinations of treatments (121).
The role of pulmonary rehabilitation
Pulmonary rehabilitation is an essential component of standard care for people who are symptomatic from chronic lung diseases causing breathlessness and functional impairment, such as COPD (135,136). Large observational studies of pulmonary rehabilitation participants have reported the prevalence of anxiety symptoms to range between 25% (137) and 32% (138), and depressive symptoms to range between 17% (137) and 27% (138). The symptoms of anxiety and depression have been associated with program non-completion (137,139), increased dyspnoea, fear of exercise and reduced functional performance both at commencement and completion of pulmonary rehabilitation (140,141). Furthermore, improvement in the symptoms of depression has been associated with improvements in specific domains of health-related quality of life (142). However, it is unclear if the symptoms of anxiety and depression should be addressed prior to entry to a pulmonary rehabilitation program or during the program.
Importantly, the symptoms of anxiety and depression have been shown to improve following completion of comprehensive pulmonary rehabilitation (143,144). In a large randomised controlled trial, participants completing pulmonary rehabilitation were shown to significantly improve symptoms of anxiety and depression when compared to the control group of usual care (144). Studies have also shown that participants with symptoms of anxiety or depression can gain similar improvements in other program benefits arising from pulmonary rehabilitation. For instance, in an observational cross-sectional study, individuals with symptoms of anxiety and depression had similar benefits in exercise capacity and health-related quality of life following pulmonary rehabilitation as participants not experiencing these symptoms (145). Moreover, another observational study reported that participants with greater symptoms of anxiety in fact had a larger improvement from exercise training following pulmonary rehabilitation (146). Therefore, the recent guideline on pulmonary rehabilitation in adults from the British Thoracic Society states that the psychological status of participants is improved with pulmonary rehabilitation when compared with usual care, and recommends that individuals with symptoms of anxiety and depression should not be excluded from pulmonary rehabilitation (147).
Recommendations and future directions in research and practice
Full spectrum anxiety and depression are highly prevalent among patients with COPD and are associated with poorer outcomes. This seems to hold even for milder or sub-threshold levels of anxiety and depression. The first step to improve practice is to achieve earlier and more accurate diagnosis of these psychological comorbidities in COPD. This is important since these conditions are underdiagnosed and consequently undertreated (8,58). Self-reported screening instruments are useful as an initial approach; however validated tools should then be utilized to minimize false positives and standardize care. When and in whom screening should be done is still not clear for patients with COPD. It is also not clear if it should be carried out with all COPD patients or just to those at higher risk of these comorbidities. After the psychological distress screening scale has been performed, high-scoring patients should be referred to a mental health specialist to facilitate access to comprehensive, gold-standard diagnostic assessment (85).
Due to the impact of associated depressive and anxiety disorders and symptoms on COPD patients, determining the best treatment approach is essential. Unfortunately, as highlighted in this review and by others, there is currently a relative scarcity of strong evidence of benefit for any specific pharmacological or non-pharmacological treatment for anxiety and depression in COPD (4). Furthermore, at this point of time, guidelines are based on treatment of depression and anxiety for the general population (3).
Due to the bidirectional nature of the association of COPD with depression and anxiety, an integrated approach that enhances the benefits between mental and physical health would be the most effective. There is extensive evidence of the benefits of pulmonary rehabilitation for patients with COPD and it has shown to significantly reduce symptoms of both anxiety and depression in COPD patients, possibly through improved physical capacity (148). Adding a depression or anxiety targeted treatment to the pulmonary rehabilitation program may have additive therapeutic benefits. This synergistic effect has been alluded to in a study where marked improvement in depression symptoms was shown when brief inpatient pulmonary rehabilitation plus antidepressants were used with COPD patients with major depression (149). Similarly, another study showed a significant improvement in anxiety and depression with improvement of physical capacity, when CBT was provided within a pulmonary rehabilitation program (101).
Future studies should aim to fill the current gaps in knowledge about treatment of psychological symptoms in COPD. First there are no large studies that have definitively assessed the true benefits of psychological, pharmacological or combined treatment modalities in the COPD population. Future studies should also focus on determining the best treatment for specific COPD groups e.g., based on gender, severity of COPD and frequency of exacerbations. There is also uncertainty regarding the cost-effectiveness of targeted treatment of anxiety and depression, and feasibility of restructuring health-care delivery to incorporate care for mood and anxiety disorders as an integral part of high quality, comprehensive chronic disease management of patients with COPD.
Summary
This review has provided an overview of the pathophysiology, prevalence and impact of anxiety and depression in patients with COPD, and has discussed diagnosis and treatment options for these important psychological comorbidities. In COPD patients, the presence of symptoms of anxiety and depression are common and have significant impacts that, adversely affect mortality rate, exacerbation rates, hospital length of stay, quality of life and functional status. Anxiety and depression are underdiagnosed in patients with COPD, and consequently undertreated. Studies examining specific pharmacological and non-pharmacological treatment of these conditions are limited and generally are comprised of small studies of varying quality. Given the current state of knowledge, many further areas of research are needed in the field of COPD chronic disease management, including in whom to screen for clinically important anxiety and depression, and the most effective and cost-effective treatment approaches for these conditions in COPD patients. A much greater awareness of the clinical importance of mental health comorbidities in COPD is urgently needed.
Acknowledgements
We sincerely thank the patients and staff of the Metro North Hospital and Health Service for their involvement in our research studies. We thank Hugh Walker (psychology intern at The Prince Charles Hospital) for assistance in the literature review.
Funding support: NHMRC Career Development Fellowship 1026215 (IY).
Authors’ contributions: All authors contributed to the writing and approved the final version of this review.
Disclosure: The authors declare no conflict of interest.
References
- Buist AS, McBurnie MA, Vollmer WM, et al. International variation in the prevalence of COPD (the BOLD Study): a population-based prevalence study. Lancet 2007;370:741-50. [PubMed]
- Australian Institute of Health and Welfare. COPD (chronic obstructive pulmonary disease). [cited 2013 Dec 28]. Available online: http://www.aihw.gov.au/copd/
- Global Strategy for the diagnosis, management and prevention of chronic obstruvtive pulmonary disease. Global Initiative for Chronic Obstructive Lung Disease; Revised 2013. Available online: http://www.goldcopd.org/ (accessed December 2013).
- Cafarella PA, Effing TW, Usmani ZA, et al. Treatments for anxiety and depression in patients with chronic obstructive pulmonary disease: a literature review. Respirology 2012;17:627-38. [PubMed]
- Hynninen KM, Breitve MH, Wiborg AB, et al. Psychological characteristics of patients with chronic obstructive pulmonary disease: a review. J Psychosom Res 2005;59:429-43. [PubMed]
- Atlantis E, Fahey P, Cochrane B, et al. Bidirectional associations between clinically relevant depression or anxiety and COPD: a systematic review and meta-analysis. Chest 2013;144:766-77. [PubMed]
- Solano JP, Gomes B, Higginson IJ. A comparison of symptom prevalence in far advanced cancer, AIDS, heart disease, chronic obstructive pulmonary disease and renal disease. J Pain Symptom Manage 2006;31:58-69. [PubMed]
- Kunik ME, Roundy K, Veazey C, et al. Surprisingly high prevalence of anxiety and depression in chronic breathing disorders. Chest 2005;127:1205-11. [PubMed]
- Yohannes AM, Baldwin RC, Connolly MJ. Depression and anxiety in elderly outpatients with chronic obstructive pulmonary disease: prevalence, and validation of the BASDEC screening questionnaire. Int J Geriatr Psychiatry 2000;15:1090-6. [PubMed]
- van Manen JG, Bindels PJ, Dekker FW, et al. Risk of depression in patients with chronic obstructive pulmonary disease and its determinants. Thorax 2002;57:412-6. [PubMed]
- Dowson C, Laing R, Barraclough R, et al. The use of the Hospital Anxiety and Depression Scale (HADS) in patients with chronic obstructive pulmonary disease: a pilot study. N Z Med J 2001;114:447-9. [PubMed]
- Di Marco F, Verga M, Reggente M, et al. Anxiety and depression in COPD patients: The roles of gender and disease severity. Respir Med 2006;100:1767-74. [PubMed]
- Hanania NA, Mullerova H, Locantore NW, et al. Determinants of depression in the ECLIPSE chronic obstructive pulmonary disease cohort. Am J Respir Crit Care Med 2011;183:604-11. [PubMed]
- Omachi TA, Katz PP, Yelin EH, et al. Depression and health-related quality of life in chronic obstructive pulmonary disease. Am J Med 2009;122:778.e9-15.
- Schneider C, Jick SS, Bothner U, et al. COPD and the risk of depression. Chest 2010;137:341-7. [PubMed]
- Lacasse Y, Rousseau L, Maltais F. Prevalence of depressive symptoms and depression in patients with severe oxygen-dependent chronic obstructive pulmonary disease. J Cardiopulm Rehabil 2001;21:80-6. [PubMed]
- Andenaes R, Kalfoss MH. Psychological distress in hospitalized patients with chronic obstructive pulmonary disease. Eur J Epidemiol 2004;19:851-9. [PubMed]
- Ng TP, Niti M, Tan WC, et al. Depressive symptoms and chronic obstructive pulmonary disease: effect on mortality, hospital readmission, symptom burden, functional status, and quality of life. Arch Intern Med 2007;167:60-7. [PubMed]
- Putman-Casdorph H, McCrone S. Chronic obstructive pulmonary disease, anxiety, and depression: state of the science. Heart Lung 2009;38:34-47. [PubMed]
- Glassman AH, Helzer JE, Covey LS, et al. Smoking, smoking cessation, and major depression. JAMA 1990;264:1546-9. [PubMed]
- Fergusson DM, Lynskey MT, Horwood LJ. Comorbidity between depressive disorders and nicotine dependence in a cohort of 16-year-olds. Arch Gen Psychiatry 1996;53:1043-7. [PubMed]
- Patton GC, Hibbert M, Rosier MJ, et al. Is smoking associated with depression and anxiety in teenagers? Am J Public Health 1996;86:225-30. [PubMed]
- Glassman AH, Covey LS, Stetner F, et al. Smoking cessation and the course of major depression: a follow-up study. Lancet 2001;357:1929-32. [PubMed]
- Wiesbeck GA, Kuhl HC, Yaldizli O, et al. Tobacco smoking and depression--results from the WHO/ISBRA study. Neuropsychobiology 2008;57:26-31. [PubMed]
- Mineur YS, Picciotto MR. Nicotine receptors and depression: revisiting and revising the cholinergic hypothesis. Trends Pharmacol Sci 2010;31:580-6. [PubMed]
- Sinden NJ, Stockley RA. Systemic inflammation and comorbidity in COPD: a result of ‘overspill’ of inflammatory mediators from the lungs? Review of the evidence. Thorax 2010;65:930-6. [PubMed]
- Eagan TM, Ueland T, Wagner PD, et al. Systemic inflammatory markers in COPD: results from the Bergen COPD Cohort Study. Eur Respir J 2010;35:540-8. [PubMed]
- Al-shair K, Kolsum U, Dockry R, et al. Biomarkers of systemic inflammation and depression and fatigue in moderate clinically stable COPD. Respir Res 2011;12:3. [PubMed]
- Marinho PE, Castro CM, Raposo MC, et al. Depressive symptoms, inflammatory markers and body composition in elderly with and without chronic obstructive pulmonary disease (COPD). Arch Gerontol Geriatr 2012;54:453-8. [PubMed]
- van Dijk EJ, Vermeer SE, de Groot JC, et al. Arterial oxygen saturation, COPD, and cerebral small vessel disease. J Neurol Neurosurg Psychiatry 2004;75:733-6. [PubMed]
- Campbell JJ 3rd, Coffey CE. Neuropsychiatric significance of subcortical hyperintensity. J Neuropsychiatry Clin Neurosci 2001;13:261-88. [PubMed]
- Brown FW, Lewine RJ, Hudgins PA, et al. White matter hyperintensity signals in psychiatric and nonpsychiatric subjects. Am J Psychiatry 1992;149:620-5. [PubMed]
- Dunlop DD, Lyons JS, Manheim LM, et al. Arthritis and heart disease as risk factors for major depression: the role of functional limitation. Med Care 2004;42:502-11. [PubMed]
- Penninx BW, van Tilburg T, Boeke AJ, et al. Effects of social support and personal coping resources on depressive symptoms: different for various chronic diseases? Health Psychol 1998;17:551-8. [PubMed]
- Mikkelsen RL, Middelboe T, Pisinger C, et al. Anxiety and depression in patients with chronic obstructive pulmonary disease (COPD). A review. Nord J Psychiatry 2004;58:65-70. [PubMed]
- Grassi M, Caldirola D, Vanni G, et al. Baseline respiratory parameters in panic disorder: a meta-analysis. J Affect Disord 2013;146:158-73. [PubMed]
- Freire RC, Perna G, Nardi AE. Panic disorder respiratory subtype: psychopathology, laboratory challenge tests, and response to treatment. Harv Rev Psychiatry 2010;18:220-9. [PubMed]
- Abrams TE, Vaughan-Sarrazin M, Van der Weg MW. Acute exacerbations of chronic obstructive pulmonary disease and the effect of existing psychiatric comorbidity on subsequent mortality. Psychosomatics 2011;52:441-9. [PubMed]
- Stage KB, Middelboe T, Pisinger C. Depression and chronic obstructive pulmonary disease (COPD). Impact on survival. Acta Psychiatr Scand 2005;111:320-3. [PubMed]
- de Voogd JN, Wempe JB, Koeter GH, et al. Depressive symptoms as predictors of mortality in patients with COPD. Chest 2009;135:619-25. [PubMed]
- Fan VS, Ramsey SD, Giardino ND, et al. Sex, depression, and risk of hospitalization and mortality in chronic obstructive pulmonary disease. Arch Intern Med 2007;167:2345-53. [PubMed]
- Crockett AJ, Cranston JM, Moss JR, et al. The impact of anxiety, depression and living alone in chronic obstructive pulmonary disease. Qual Life Res 2002;11:309-16. [PubMed]
- Divo M, Cote C, de Torres JP, et al. Comorbidities and risk of mortality in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2012;186:155-61. [PubMed]
- Keating A, Lee A, Holland AE. What prevents people with chronic obstructive pulmonary disease from attending pulmonary rehabilitation? A systematic review. Chron Respir Dis 2011;8:89-99. [PubMed]
- Bhandari NJ, Jain T, Marolda C, et al. Comprehensive pulmonary rehabilitation results in clinically meaningful improvements in anxiety and depression in patients with chronic obstructive pulmonary disease. J Cardiopulm Rehabil Prev 2013;33:123-7. [PubMed]
- DiMatteo MR, Lepper HS, Croghan TW. Depression is a risk factor for noncompliance with medical treatment: meta-analysis of the effects of anxiety and depression on patient adherence. Arch Intern Med 2000;160:2101-7. [PubMed]
- Groenewegen KH, Schols AM, Wouters EF. Mortality and mortality-related factors after hospitalization for acute exacerbation of COPD. Chest 2003;124:459-67. [PubMed]
- Pooler A, Beech R. Examining the relationship between anxiety and depression and exacerbations of COPD which result in hospital admission: a systematic review. Int J Chron Obstruct Pulmon Dis 2014;9:315-30. [PubMed]
- Laurin C, Moullec G, Bacon SL, et al. Impact of anxiety and depression on chronic obstructive pulmonary disease exacerbation risk. Am J Respir Crit Care Med 2012;185:918-23. [PubMed]
- Xu W, Collet JP, Shapiro S, et al. Independent effect of depression and anxiety on chronic obstructive pulmonary disease exacerbations and hospitalizations. Am J Respir Crit Care Med 2008;178:913-20. [PubMed]
- Koenig HG, Kuchibhatla M. Use of health services by hospitalized medically ill depressed elderly patients. Am J Psychiatry 1998;155:871-7. [PubMed]
- Bosley CM, Corden ZM, Rees PJ, et al. Psychological factors associated with use of home nebulized therapy for COPD. Eur Respir J 1996;9:2346-50. [PubMed]
- Cohen S, Tyrrell DA, Smith AP. Negative life events, perceived stress, negative affect, and susceptibility to the common cold. J Pers Soc Psychol 1993;64:131-40. [PubMed]
- Regvat J, Zmitek A, Vegnuti M, et al. Anxiety and depression during hospital treatment of exacerbation of chronic obstructive pulmonary disease. J Int Med Res 2011;39:1028-38. [PubMed]
- Ormel J, Kempen GI, Deeg DJ, et al. Functioning, well-being, and health perception in late middle-aged and older people: comparing the effects of depressive symptoms and chronic medical conditions. J Am Geriatr Soc 1998;46:39-48. [PubMed]
- Yohannes AM, Willgoss TG, Baldwin RC, et al. Depression and anxiety in chronic heart failure and chronic obstructive pulmonary disease: prevalence, relevance, clinical implications and management principles. Int J Geriatr Psychiatry 2010;25:1209-21. [PubMed]
- Wells KB, Golding JM, Burnam MA. Psychiatric disorder and limitations in physical functioning in a sample of the Los Angeles general population. Am J Psychiatry 1988;145:712-7. [PubMed]
- Kim HF, Kunik ME, Molinari VA, et al. Functional impairment in COPD patients: the impact of anxiety and depression. Psychosomatics 2000;41:465-71. [PubMed]
- Weaver TE, Richmond TS, Narsavage GL. An explanatory model of functional status in chronic obstructive pulmonary disease. Nurs Res 1997;46:26-31. [PubMed]
- Von Korff M, Katon W, Rutter C, et al. Effect on disability outcomes of a depression relapse prevention program. Psychosom Med 2003;65:938-43. [PubMed]
- Aydin IO, Ulusahin A. Depression, anxiety comorbidity, and disability in tuberculosis and chronic obstructive pulmonary disease patients: applicability of GHQ-12. Gen Hosp Psychiatry 2001;23:77-83. [PubMed]
- Borak J, Chodosowska E, Matuszewski A, et al. Emotional status does not alter exercise tolerance in patients with chronic obstructive pulmonary disease. Eur Respir J 1998;12:370-3. [PubMed]
- Tsiligianni I, Kocks J, Tzanakis N, et al. Factors that influence disease-specific quality of life or health status in patients with COPD: a review and meta-analysis of Pearson correlations. Prim Care Respir J 2011;20:257-68. [PubMed]
- Beck JG, Scott SK, Teague RB, et al. Correlates of daily impairment in COPD. Rehabilitation Psychology 1988;33:77-84.
- Kellner R, Samet J, Pathak D. Dyspnea, anxiety, and depression in chronic respiratory impairment. Gen Hosp Psychiatry 1992;14:20-8. [PubMed]
- Doyle T, Palmer S, Johnson J, et al. Association of anxiety and depression with pulmonary-specific symptoms in chronic obstructive pulmonary disease. Int J Psychiatry Med 2013;45:189-202. [PubMed]
- Tselebis A, Bratis D, Kosmas E, et al. Psychological symptom patterns and vital exhaustion in outpatients with chronic obstructive pulmonary disease. Ann Gen Psychiatry 2011;10:32. [PubMed]
- Balcells E, Gea J, Ferrer J, et al. Factors affecting the relationship between psychological status and quality of life in COPD patients. Health Qual Life Outcomes 2010;8:108. [PubMed]
- Janssen DJ, Spruit MA, Schols JM, et al. Predicting changes in preferences for life-sustaining treatment among patients with advanced chronic organ failure. Chest 2012;141:1251-9. [PubMed]
- Meier C, Bodenmann G, Morgeli H, et al. Dyadic coping, quality of life, and psychological distress among chronic obstructive pulmonary disease patients and their partners. Int J Chron Obstruct Pulmon Dis 2011;6:583-96. [PubMed]
- National Institute for Health and Clinical Excellence. Generalised anxiety disorder and panic disorder (with or without agoraphobia) in adults. Management in primary, secondary and community care. NICE clinical guideline 113. Issued: January 2011.
- National Institute for Health and Clinical Excellence. Depression. The treatment and management of depression in adults. This is a partial update of NICE clinical guideline 23. NICE clinical guideline 90. Issue date: October 2009.
- Trivedi MH, Daly EJ. Measurement-based care for refractory depression: a clinical decision support model for clinical research and practice. Drug Alcohol Depend 2007;88 Suppl 2:S61-71. [PubMed]
- Tang WK, Wong E, Chiu HF, et al. Examining item bias in the anxiety subscale of the Hospital Anxiety and Depression Scale in patients with chronic obstructive pulmonary disease. Int J Methods Psychiatr Res 2008;17:104-10. [PubMed]
- Julian LJ, Gregorich SE, Earnest G, et al. Screening for depression in chronic obstructive pulmonary disease. COPD 2009;6:452-8. [PubMed]
- Cheung G, Patrick C, Sullivan G, et al. Sensitivity and specificity of the Geriatric Anxiety Inventory and the Hospital Anxiety and Depression Scale in the detection of anxiety disorders in older people with chronic obstructive pulmonary disease. Int Psychogeriatr 2012;24:128-36. [PubMed]
- Willgoss TG, Goldbart J, Fatoye F, et al. The development and validation of the anxiety inventory for respiratory disease. Chest 2013;144:1587-96. [PubMed]
- Steer RA, Beck AT, Riskind JH, et al. Differentiation of depressive disorders from generalized anxiety by the Beck Depression Inventory. J Clin Psychol 1986;42:475-8. [PubMed]
- Jani BD, Purves D, Barry S, et al. Challenges and implications of routine depression screening for depression in chronic disease and multimorbidity: a cross sectional study. PLoS One 2013;8:e74610. [PubMed]
- Gilbody S, Sheldon T, House A. Screening and case-finding instruments for depression: a meta-analysis. CMAJ 2008;178:997-1003. [PubMed]
- Gilbody S, House AO, Sheldon TA. Screening and case finding instruments for depression. Cochrane Database Syst Rev 2005;CD002792. [PubMed]
- World Health Organization: Innovative Care for Chronic Conditions: Building Blocks for Action. World Health Organization: Innovative Care for Chronic Conditions: Building Blocks for Action. World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland: 2002.
- Coventry PA, Bower P, Keyworth C, et al. The effect of complex interventions on depression and anxiety in chronic obstructive pulmonary disease: systematic review and meta-analysis. PLoS One 2013;8:e60532. [PubMed]
- Abramson M, Crockett AJ, Dabscheck E, et al. On behalf of Lung Foundation Australia and the Thoracic So ciety of Australia and New Zealand. The COPD-X Plan: Australian and New Zealand Guidelines for the management of Chronic Obstructive Pulmonary Disease V2.37, April 2014.
- National Institute for Health and Clinical Excellence. CG91 Depression with a Chronic Physical Health Problem: NICE Guideline. National Collaborating Centre for Mental Health, London, 2009.
- Vickers A, Zollman C. ABC of complementary medicine. Hypnosis and relaxation therapies. BMJ 1999;319:1346-9. [PubMed]
- Devine EC, Pearcy J. Meta-analysis of the effects of psychoeducational care in adults with chronic obstructive pulmonary disease. Patient Educ Couns 1996;29:167-78. [PubMed]
- Lolak S, Connors GL, Sheridan MJ, et al. Effects of progressive muscle relaxation training on anxiety and depression in patients enrolled in an outpatient pulmonary rehabilitation program. Psychother Psychosom 2008;77:119-25. [PubMed]
- Yeh GY, Roberts DH, Wayne PM, et al. Tai chi exercise for patients with chronic obstructive pulmonary disease: a pilot study. Respir Care 2010;55:1475-82. [PubMed]
- Donesky-Cuenco D, Nguyen HQ, Paul S, et al. Yoga therapy decreases dyspnea-related distress and improves functional performance in people with chronic obstructive pulmonary disease: a pilot study. J Altern Complement Med 2009;15:225-34. [PubMed]
- Bonilha AG, Onofre F, Vieira ML, et al. Effects of singing classes on pulmonary function and quality of life of COPD patients. Int J Chron Obstruct Pulmon Dis 2009;4:1-8. [PubMed]
- Lord VM, Cave P, Hume VJ, et al. Singing teaching as a therapy for chronic respiratory disease--a randomised controlled trial and qualitative evaluation. BMC Pulm Med 2010;10:41. [PubMed]
- Lord VM, Hume VJ, Kelly JL, et al. Singing classes for chronic obstructive pulmonary disease: a randomized controlled trial. BMC Pulm Med 2012;12:69. [PubMed]
- Greenberger D, Padesky CA. Mind Over Mood: A Cognitive Therapy Treatment. Manual for Clients. New York, NY: Guilford Press, 1995.
- Tyrer P, Cooper S, Salkovskis P, et al. Clinical and cost-effectiveness of cognitive behaviour therapy for health anxiety in medical patients: a multicentre randomised controlled trial. Lancet 2014;383:219-25. [PubMed]
- Emery CF, Schein RL, Hauck ER, et al. Psychological and cognitive outcomes of a randomized trial of exercise among patients with chronic obstructive pulmonary disease. Health Psychol 1998;17:232-40. [PubMed]
- Hynninen MJ, Bjerke N, Pallesen S, et al. A randomized controlled trial of cognitive behavioral therapy for anxiety and depression in COPD. Respir Med 2010;104:986-94. [PubMed]
- Kunik ME, Braun U, Stanley MA, et al. One session cognitive behavioural therapy for elderly patients with chronic obstructive pulmonary disease. Psychol Med 2001;31:717-23. [PubMed]
- Kunik ME, Veazey C, Cully JA, et al. COPD education and cognitive behavioral therapy group treatment for clinically significant symptoms of depression and anxiety in COPD patients: a randomized controlled trial. Psychol Med 2008;38:385-96. [PubMed]
- Livermore N, Sharpe L, McKenzie D. Prevention of panic attacks and panic disorder in COPD. Eur Respir J 2010;35:557-63. [PubMed]
- de Godoy DV, de Godoy RF. A randomized controlled trial of the effect of psychotherapy on anxiety and depression in chronic obstructive pulmonary disease. Arch Phys Med Rehabil 2003;84:1154-7. [PubMed]
- Stiles-Shields C, Kwasny MJ, Cai X, et al. Therapeutic alliance in face-to-face and telephone-administered cognitive behavioral therapy. J Consult Clin Psychol 2014;82:349-54. [PubMed]
- Mohr DC, Hart SL, Julian L, et al. Telephone-administered psychotherapy for depression. Arch Gen Psychiatry 2005;62:1007-14. [PubMed]
- Mohr DC, Vella L, Hart S, et al. The Effect of Telephone-Administered Psychotherapy on Symptoms of Depression and Attrition: A Meta-Analysis. Clin Psychol (New York) 2008;15:243-53. [PubMed]
- Veazey C, Cook KF, Stanley M, et al. Telephone-administered cognitive behavioral therapy: a case study of anxiety and depression in Parkinson’s disease. J Clin Psychol Med Settings 2009;16:243-53. [PubMed]
- Watson M, White C, Davolls S, et al. Problem-focussed interactive telephone therapy for cancer patients: a phase II feasibility trial. Psychooncology 2013;22:1485-91. [PubMed]
- Andersson G. Guided internet treatment for anxiety disorders. As effective as face-to-face therapies? Stud Health Technol Inform 2012;181:3-7. [PubMed]
- Månsson KN, Skagius Ruiz E, Gervind E, et al. Development and initial evaluation of an Internet-based support system for face-to-face cognitive behavior therapy: a proof of concept study. J Med Internet Res 2013;15:e280. [PubMed]
- Cuijpers P, Donker T, van Straten A, et al. Is guided self-help as effective as face-to-face psychotherapy for depression and anxiety disorders? A systematic review and meta-analysis of comparative outcome studies. Psychol Med 2010;40:1943-57. [PubMed]
- Lamers F, Jonkers CC, Bosma H, et al. Improving quality of life in depressed COPD patients: effectiveness of a minimal psychological intervention. COPD 2010;7:315-22. [PubMed]
- Ekers D, Richards D, Gilbody S. A meta-analysis of randomized trials of behavioural treatment of depression. Psychol Med 2008;38:611-23. [PubMed]
- Jonker AA, Comijs HC, Knipscheer KC, et al. Promotion of self-management in vulnerable older people: a narrative literature review of outcomes of the Chronic Disease Self-Management Program (CDSMP). Eur J Ageing 2009;6:303-14. [PubMed]
- Effing T, Monninkhof EM, van der Valk PD, et al. Self-management education for patients with chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2007;CD002990. [PubMed]
- Bourbeau J, Julien M, Maltais F, et al. Reduction of hospital utilization in patients with chronic obstructive pulmonary disease: a disease-specific self-management intervention. Arch Intern Med 2003;163:585-91. [PubMed]
- McLaughlin TJ, Aupont O, Bambauer KZ, et al. Improving psychologic adjustment to chronic illness in cardiac patients. The role of depression and anxiety. J Gen Intern Med 2005;20:1084-90. [PubMed]
- Kaptein AA, Scharloo M, Fischer MJ, et al. 50 years of psychological research on patients with COPD--road to ruin or highway to heaven? Respir Med 2009;103:3-11. [PubMed]
- Robinson A, Courtney-Pratt H, Lea E, et al. Transforming clinical practice amongst community nurses: mentoring for COPD patient self-management. J Clin Nurs 2008. [Epub ahead of print]. [PubMed]
- Wood-Baker R, Reid D, Robinson A, et al. Clinical trial of community nurse mentoring to improve self-management in patients with chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis 2012;7:407-13. [PubMed]
- Walters J, Cameron-Tucker H, Wills K, et al. Effects of telephone health mentoring in community-recruited chronic obstructive pulmonary disease on self-management capacity, quality of life and psychological morbidity: a randomised controlled trial. BMJ Open 2013;3:e003097. [PubMed]
- Effing T, Kerstjens H, van der Valk P, et al. (Cost)-effectiveness of self-treatment of exacerbations on the severity of exacerbations in patients with COPD: the COPE II study. Thorax 2009;64:956-62. [PubMed]
- Huhn M, Tardy M, Spineli LM, et al. Efficacy of pharmacotherapy and psychotherapy for adult psychiatric disorders: a systematic overview of meta-analyses. JAMA Psychiatry 2014;71:706-15. [PubMed]
- Usmani ZA, Carson KV, Cheng JN, et al. Pharmacological interventions for the treatment of anxiety disorders in chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2011;CD008483. [PubMed]
- Rayner L, Price A, Evans A, et al. Antidepressants for depression in physically ill people. Cochrane Database Syst Rev 2010;CD007503. [PubMed]
- Evans M, Hammond M, Wilson K, et al. Placebo-controlled treatment trial of depression in elderly physically ill patients. Int J Geriatr Psychiatry 1997;12:817-24. [PubMed]
- Bystritsky A, Khalsa SS, Cameron ME, et al. Current diagnosis and treatment of anxiety disorders. P T 2013;38:30-57.
- Lacasse Y, Beaudoin L, Rousseau L, et al. Randomized trial of paroxetine in end-stage COPD. Monaldi Arch Chest Dis 2004;61:140-7. [PubMed]
- Eiser N, Harte R, Spiros K, et al. Effect of treating depression on quality-of-life and exercise tolerance in severe COPD. COPD 2005;2:233-41. [PubMed]
- Yohannes AM, Connolly MJ, Baldwin RC. A feasibility study of antidepressant drug therapy in depressed elderly patients with chronic obstructive pulmonary disease. Int J Geriatr Psychiatry 2001;16:451-4. [PubMed]
- Light RW, Merrill EJ, Despars J, et al. Doxepin treatment of depressed patients with chronic obstructive pulmonary disease. Arch Intern Med 1986;146:1377-80. [PubMed]
- Ström K, Boman G, Pehrsson K, et al. Effect of protriptyline, 10 mg daily, on chronic hypoxaemia in chronic obstructive pulmonary disease. Eur Respir J 1995;8:425-9. [PubMed]
- Borson S, McDonald GJ, Gayle T, et al. Improvement in mood, physical symptoms, and function with nortriptyline for depression in patients with chronic obstructive pulmonary disease. Psychosomatics 1992;33:190-201. [PubMed]
- Yohannes AM, Connolly MJ. Do antidepressants work in patients with chronic obstructive pulmonary disease with comorbid depression? Expert Rev Respir Med 2011;5:727-9. [PubMed]
- Singh NP, Despars JA, Stansbury DW, et al. Effects of buspirone on anxiety levels and exercise tolerance in patients with chronic airflow obstruction and mild anxiety. Chest 1993;103:800-4. [PubMed]
- Ejiofor S, Turner AM. Pharmacotherapies for COPD. Clin Med Insights Circ Respir Pulm Med 2013;7:17-34. [PubMed]
- Ries AL, Bauldoff GS, Carlin BW, et al. Pulmonary Rehabilitation: Joint ACCP/AACVPR Evidence-Based Clinical Practice Guidelines. Chest 2007;131:4S-42S. [PubMed]
- Coleman PG, Philp I, Mullee MA. Does the use of the Geriatric Depression Scale make redundant the need for separate measures of well-being on geriatrics wards? Age Ageing 1995;24:416-20. [PubMed]
- Bhandari NJ, Jain T, Marolda C, et al. Comprehensive pulmonary rehabilitation results in clinically meaningful improvements in anxiety and depression in patients with chronic obstructive pulmonary disease. Journal of cardiopulmonary rehabilitation and prevention 2013;33:123-7. [PubMed]
- Janssen DJ, Spruit MA, Leue C, et al. Symptoms of anxiety and depression in COPD patients entering pulmonary rehabilitation. Chronic respiratory disease 2010;7:147-57. [PubMed]
- Garrod R, Marshall J, Barley E, et al. Predictors of success and failure in pulmonary rehabilitation. Eur Respir J 2006;27:788-94. [PubMed]
- von Leupoldt A, Taube K, Lehmann K, et al. The impact of anxiety and depression on outcomes of pulmonary rehabilitation in patients with COPD. Chest 2011;140:730-6. [PubMed]
- Harris D, Hayter M, Allender S. Improving the uptake of pulmonary rehabilitation in patients with COPD: qualitative study of experiences and attitudes. Br J Gen Pract 2008;58:703-10. [PubMed]
- Pirraglia PA, Casserly B, Velasco R, et al. Association of change in depression and anxiety symptoms with functional outcomes in pulmonary rehabilitation patients. Journal of psychosomatic research 2011;71:45-9. [PubMed]
- Paz-Díaz H, Montes de Oca M, López JM, et al. Pulmonary rehabilitation improves depression, anxiety, dyspnea and health status in patients with COPD. Am J Phys Med Rehabil 2007;86:30-6. [PubMed]
- Griffiths TL, Burr ML, Campbell IA, et al. Results at 1 year of outpatient multidisciplinary pulmonary rehabilitation: a randomised controlled trial. Lancet 2000;355:362-8. [PubMed]
- Trappenburg JC, Troosters T, Spruit MA, et al. Psychosocial conditions do not affect short-term outcome of multidisciplinary rehabilitation in chronic obstructive pulmonary disease. Arch Phys Med Rehabil 2005;86:1788-92. [PubMed]
- Withers NJ, Rudkin ST, White RJ. Anxiety and depression in severe chronic obstructive pulmonary disease: the effects of pulmonary rehabilitation. J Cardiopulm Rehabil 1999;19:362-5. [PubMed]
- Bolton CE, Bevan-Smith EF, Blakey JD, et al. British Thoracic Society guideline on pulmonary rehabilitation in adults. Thorax 2013;68 Suppl 2:ii1-30. [PubMed]
- Coventry PA, Hind D. Comprehensive pulmonary rehabilitation for anxiety and depression in adults with chronic obstructive pulmonary disease: Systematic review and meta-analysis. J Psychosom Res 2007;63:551-65. [PubMed]
- Alexopoulos GS, Sirey JA, Raue PJ, et al. Outcomes of depressed patients undergoing inpatient pulmonary rehabilitation. Am J Geriatr Psychiatry 2006;14:466-75. [PubMed]


