Chinese National Guidelines on Diagnosis and Management of Cough: consensus and controversy
Cough, especially chronic cough, is a common condition in clinical practice. Chronic cough accounts for at least 30% of respiratory specialist visits and significantly interferes with patients’ daily life, and nearly 50% women patients with chronic cough suffer from urinary incontinence (1). The Asthma Workgroup of the Chinese Society of Respiratory Diseases (CSRD) issued The Chinese National Guideline on Diagnosis and Management of Cough (draft) in 2005 (2). The guideline primarily focuses on the etiological diagnosis and management of chronic cough. Since the establishment of the guideline, many clinicians, especially respiratory specialists, have significantly improved their expertise on the diagnosis of chronic cough, which has an important instructive impact on clinical practice. Therefore, the CRSD has revised the 2005 cough guideline to further improve the guideline and better present the progresses achieved both in China and abroad (3,4). The consensus and controversy on the guidelines are discussed in the present review.
General structure
The 2009 revised Chinese National Guidelines on Diagnosis and Management of Cough continue to adhere to principles of “comprehensive content, highlighted emphases, clinical practicability”; the structure and content of the earlier 2005 guidelines are preserved with only partial emendation (Table 1). There are seven sections and one annex in the 2005 guideline, and there are nine sections in the 2009 guideline, the added two sections of which include empirical treatment and expectorants for chronic cough. In addition, subacute cough is now listed independently. Acute cough covers acute tracheobronchitis besides the common cold. Post-infectious cough, also known as post-viral cough, is categorized under subacute cough. The common causes of chronic cough are upper airway cough symptoms [postnasal drip syndrome (PNDS)], cough variant asthma (CVA), eosinophilic bronchitis (EB), and gastroesophageal reflux cough (GERC). Other causes include chronic bronchitis, bronchiectasis, atopic cough (AC), bronchial tuberculosis, angiotensin-converting enzyme inhibitors induced (ACEI-induced) cough, and psychogenic cough. Central bronchogenic carcinoma has also been included in the 2009 guidelines because cough is often an early symptom.
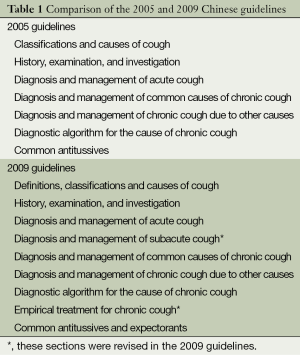
Full table
The annex includes induced-sputum differential cell tests, cough sensitivity test and 24 h pH monitoring, and evaluation methods of cough severity.
Diagnostic terminology
Four diagnostic terms for chronic cough have been revised in the 2009 guidelines (Table 1). PNDS was first introduced first in the United States. The syndrome is characterized by chronic cough caused by nasal secretions that accumulate in the pharynx or posterior nasal cavity, and is often associated with rhinitis or sinusitis. However, the classic signs of PNDS, cobblestone appearance of the oropharyngeal mucosa, and mucus accumulation in the posterior pharynx, are not observed in some patients with cough caused by upper airway disease. It is unclear whether cough secondary to upper airway disease is caused by stimulation of the pharynx by postnasal drip or by inflammatory stimulation of cough receptors. As a result, the definition of PNDS has not been widely accepted, and in Europe, “rhinitis/sinusitis” is instead used to refer to cough caused by nasal disease (5,6). For these reasons, the Guidelines Committee for Cough of the American College of Chest Physicians (ACCP) recommended replacing the term PNDS with a new term, upper airway cough syndrome (UACS), in their 2006 revision of the American Guidelines on Diagnosis and Management of Cough (7). The latest Chinese guidelines have also adopted this new diagnostic term. In the 2nd edition of the ACCP guidelines, the definition of UACS remained limited to rhinitis and sinusitis. Besides rhinitis and sinusitis, other upper airway diseases such as chronic laryngopharyngitis and chronic tonsillitis, and even lesions at the base of the tongue may initiate cough (8-10). Accordingly, the definition of UACS in the latest Chinese guidelines covers all these potential causes. PNDS is also described in the 2009 guidelines to maintain continuity although it is to be replaced with UACS. For patients who report postnasal drip as a typical symptom, the term PNDS is easier to understand. Because tuberculosis is a common disease in China, bronchial tuberculosis is also included among the causes in the 2005 guidelines.
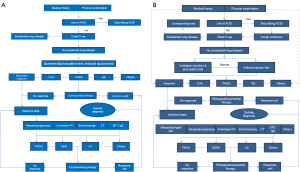
Diagnostic algorithm
There is no change in the diagnostic algorithm for determining the cause of chronic cough, and only a few revisions were made (Figure 1). CVA and EB are the most common causes of chronic cough, therefore, spirometry with airway hyperresponsiveness (AHR) and induced sputum differential cell test are listed as the first line tests in the 1st edition of the cough guidelines. However, the induced sputum test has not been widely conducted, so the latest guidelines provide an alternative diagnostic approach. Only patients with a negative AHR test should undergo an induced-sputum test. Moreover, empirical treatment has been added as one option in the diagnostic algorithm.
Diagnosis and management of common causes
Eosinophilic bronchitis (EB)
Currently, an eosinophil count (Eos% >3%) in induced-sputum is generally considered diagnostic standard for EB. However, based on the normal reference range of induced sputum cytology tests in China, the diagnostic criteria for EB were changed from an Eos% ≥3% to Eos% ≥2.5%. EB is one of common causes of chronic cough in China, ranging from 13.2-24% (11,12). A moderate dose of inhaled corticosteroid (ICS) is usually administered, typically budesonide 200-400 μg twice daily for at least 4 weeks duration. Oral prednisolone at 10-20 mg daily for 3-5 days may also be administered initially. EB responds well to corticosteroid, but there is no consensus on the appropriate treatment duration and it is based on evidence-based studies, and a few patients who experience recurrence after ceasing treatment may require a longer duration of therapy.
Cough variant asthma (CVA)
CVA is the most common cause of chronic cough in China, accounting for one thirds of chronic cough. The European and American guidelines do not discuss specific diagnostic criteria, but they do highlight the diagnostic value of AHR and recommend that the CVA diagnosis should be determined according to the therapeutic response. The Chinese guidelines take the successful treatment of bronchodilators as the basic diagnostic criteria of CVA, which is also done in the Japanese guidelines. In Japan, normal cough sensitivity is one of the diagnostic criteria for CVA; however, our studies showed that cough sensitivity may increase in some CVA patients (13). The guidelines in China, Europe, and the United States all state that the principles for CVA treatment are identical to those for classic asthma: a combination of low-dose ICS and bronchodilators initially for at least 8 weeks, along with short-term oral glucocorticoid if necessary. For refractory cough after treatment with ICS and bronchodilators, leukotriene receptor antagonist can be prescribed. Classic asthma is likely to develop in 30% of these patients (14), and an increased eosinophilia in the induced sputum is a risk factor (15). Long-term ICS can significantly reduce the incidence of classic asthma. However, a conclusion has yet to be reached on how long CVA should be treated.
Upper airway cough syndrome (UACS)
The diagnosis of UACS is based on history, symptoms, signs and response to treatment. There are not objective standards. Management varies with the underlying cause of UACS. Specific treatment is available for patients with a definitive cause, but effective empirical treatment can be offered before definitive diagnosis to patients with an unclear cause. First-generation antihistamines and decongestants should be the initial treatment for UACS that caused by non-allergic rhinitis and the common cold.
Gastroesophageal reflux cough (GERC)
GERC in China is not as common as it is in western countries. GERC is managed as follows: (I) adjustment of lifestyle: patients are encouraged to lose weight; eat more frequent but smaller meals; avoid overeating, meals immediately before sleeping, and acidic and greasy food or beverages; refrain from consuming coffee and smoking; (II) antacids: patients are generally prescribed a proton pump inhibitor (PPI) such as omeprazole or similar drugs, or an H2 receptor antagonist (H2RA) such as ranitidine; (III) prokinetic drugs such as domperidone; (IV) medical treatment for at least 3 months; (V) surgery: for the minority of patients with severe gastroesophageal reflux who fail to respond to medical treatment, anti-reflux surgery may be considered.
The efficacy of PPIs in treating GERC is not certain among different studies (16,17). It must be emphasized that chronic cough and reflux share a reciprocal causation relationship, meaning that for patients failing to respond to anti-reflux therapy, the reflux could merely be a symptom caused by the chronic cough instead of its cause.
Atopic cough (AC)
AC, a common cause of chronic cough, was initially defined in Japan and refers to patients presenting with eosinophilia in the induced sputum or with atopic features. Antihistamines and glucocorticoids are effective in these patients. According to the Japanese definition, 80% of AC cases overlap with EB. However, we have found that many patients do not show eosinophilia in the induced sputum and have no history of rhinitis or sinusitis; however, they do have atopic features or have been exposed to allergens, and are sensitive to antihistamines or glucocorticoids. This scenario can not be diagnosed as UACS or EB, therefore we defined it as AC in Chinese guidelines, which accounts about 10% of chronic cough cases. We do believe that AC exists, but there is still no definite conclusion in western countries. Further study of the mechanism and pathophysiological characteristics of AC have yet to be performed.
Expectorant agents
The section of common antitussives is unchanged basically in the revised guidelines. There are multiple expectorant agents. Some are effective in clinical practice but lack evidence-based support. In the current guidelines, common expectorant agents are described, including guaifenesin, ambroxol, bromhexine, acetylcysteine, and carbocisteine. Hypertonic saline and mannitol may improve airway hydration as well as removal of mucus.
Empirical treatment
Facilities remain inadequate in many primary hospitals in China, a developing country. Some patients receive empirical treatment because they are seldom examined due to economic and other limitations. The revised guidelines introduce six principles to improve the efficacy of empirical treatment. The first is to treat primarily according to the common causes of chronic cough. In western countries, empirical treatment generally targets UACS/PNDS owing to its high incidence in these locales. However, in China, the most common causes of chronic cough are CVA, EB, AC, which can be termed as hormone-sensitive cough. The second principle is to presume the potential cause according to the patient’s history. The case is treated as CVA if the main presenting symptom is an irritable cough in the night; treated as GERC if the cough is accompanied by obvious acid reflux, belching, and heartburn; managed as post-infection cough if the cough is secondary to cold and has persisted chronically; or as UACS or PNDS if the patient has nasopharyngeal disease accompanied by cough, nasal discharge, nasal obstruction and itching, constant throat clearing, and postnasal drip.
For UACS/PNDS, AC, and postinfectious cough, combined medications which are economical and effective to a wide variety of symptoms are initially recommended, such as compounds preparation which contains pseudoephedrine hydrochloride, first anti-histamine drugs and methoxyphenamine. For suspected cases of corticosteroids-sensitive cough, oral corticosteroids at low does is recommended for 3 to 5 days, which is followed by ICS therapy or combined corticosteroids and β2-adrenergic receptor agonist therapy if the symptoms improve. Antibiotics are recommended for cough accompanied by purulent sputum or purulent nasal discharge. Antibiotics are not advised for empirical treatment because infection is not related with chronic cough in most cases.
Empirical treatment generally requires 1 to 2 weeks duration in cases suspected as UACS, PNDS, CVA, or EB, and it requires at least 2 to 4 weeks in suspected GERC cases. Oral glucocorticoids should be administered for no longer than 1 week. Patients who are responsive well to initial treatment should continue the standard therapeutic regimen for that particular cause of cough. Finally, it must be emphasized that empirical treatment should be performed based on the cause distribution of chronic cough in the local area, and the traditional method of “chronic cough-chronic bronchitis/laryngitis-antibiotics combined with antitussives” should be avoided. Those patients who fail to respond to empirical treatment should be referred to large hospital to identify the potential causes.
Evaluation of cough symptom
Evaluation of cough includes cough symptom scoring, cough life quality, cough frequency monitoring, and cough sound analysis. Currently in China, cough frequency monitoring and cough sound analysis are not applied in clinical practice. The 2009 guidelines introduce the cough symptom scoring system and visual analogue scale (VAS).
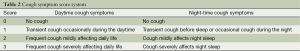
Cough symptom scoring
The cough symptom scoring system includes both day-time and night-time cough symptom scores. Each component is scored from 0 to 3 according to the severity (Table 2). This scoring system reflects the cough frequency, intensity, and its impact on life quality. Notably, in both adults and children, the day-time scores are significantly correlated with cough frequency, but the night-time scores and cough monitoring indicators do not show an obvious correlation.
Full table
Visual analogue scale (VAS)
VAS is a linear scoring method using a graduated line scaled from 0-10 cm or from 0-100 mm. The 0-score indicates an absence of cough, and a 10-score indicates the most severe cough. The score is generated by the patient according to the subjective severity of cough and may be conducted before and after treatment. The higher the score, the more severe the cough is. The VAS score is useful to describe differences in longitudinal comparison of cough severity before and after treatment. The VAS scale is also repeatable, efficient, and strongly correlated with life quality.
Conclusions
The great progress on diagnosis and treatment of chronic cough in China has been made although there are still problems to be resolved. We sincerely hope that the promotion and adoption of these guidelines will enhance the understanding of the etiological diagnosis and management of chronic cough by clinicians, advance more institutions to study chronic cough, promote international exchanges.
Acknowledgements
I hereby express my deep gratitude to Rebecca Rui Wong and Tina Chu Pei for their translating this manuscript and to Guangqiao Zeng and Baojuan Liu for their assist in proof reading and revising the manuscript. I am also grateful for the expert team involved in developing the guidelines.
Disclosure: The author declares no conflict of interest.
References
- Yang CZ, Chen RC, Li BK, et al. Survey of quality of life and incontinence in female patients with chronic cough. Chin J Asthma 2010;4:199-202.
- Asthma Workgroup of Chinese Society of Respiratory Diseases (CSRD), Chinese Medical, Association. The Chinese national guidelines on diagnosis and management of cough (draft). Chin J Tuberc Respir Dis 2005;28:738-44.
- Asthma Workgroup of Chinese Society of Respiratory Diseases (CSRD), Chinese Medical, Association. The Chinese national guidelines on diagnosis and management of cough. Chin J Tuberc Respir Dis 2009;32:407-13.
- Asthma Workgroup, Chinese Society, Respiratory, et al. The Chinese national guidelines on diagnosis and management of cough (December 2010). Chin Med J (Engl) 2011;124:3207-19. [PubMed]
- Morice AH, Fontana GA, Sovijarvi AR, et al. The diagnosis and management of chronic cough. Eur Respir J 2004;24:481-492. [PubMed]
- Morice AH, McGarvey L, Pavord I, et al. Recommendations for the management of cough in adults. Thorax 2006;61 Suppl 1:i1-24. [PubMed]
- Pratter MR. Chronic upper airway cough syndrome secondary to rhinosinus diseases (previously referred to as postnasal drip syndrome): ACCP evidence-based clinical practice guidelines. Chest 2006;129:63S-71S. [PubMed]
- Zhang Q, Ma QL, Huang ZS, et al. A Preliminary Study on Etiology of Upper Airway Cough Syndrome. Chin J Respir Crit Care Med 2010;9:458-61.
- Birring SS, Passant C, Patel RB, et al. Chronic tonsillar enlargement and cough: preliminary evidence of a novel and treatable cause of chronic cough. Eur Respir J 2004;23:199-201. [PubMed]
- Tan YX, Lin L, Lai KF, et al. Chronic cough caused by salivary gland ectopia at the base of tongue: A case report. Chin J Tuberc Respir Dis 2009;32:473-4.
- Brightling CE, Ward R, Goh KL, et al. Eosinophilic bronchitis is an important cause of chronic cough. Am J Respir Crit Care Med 1999;160:406-10. [PubMed]
- Lai K, Chen R, Lin J, et al. A prospective, multicenter survey on causes of chronic cough in China. Chest 2013;143:613-20. [PubMed]
- The committee for The Japanese Respiratory Society guidelines for management of cough (2006), Prolonged and chronic cough. Respirology 2006;11:S160-74.
- Matsumoto H, Niimi A, Takemura M, et al. Prognosis of cough variant asthma: a retrospective analysis. J Asthma 2006;43:131-5. [PubMed]
- Kim CK, Kim JT, Kang H, et al. Sputum eosinophilia in cough-variant asthma as a predictor of the subsequent development of classic asthma. Clin Exp Allergy 2003;33:1409-14. [PubMed]
- Chang AB, Lasserson TJ, Kiljander TO, et al. Systematic review and meta-analysis of randomised controlled trials of gastro-oesophageal reflux interventions for chronic cough associated with gastro-oesophageal reflux. BMJ 2006;332:11-7. [PubMed]
- Faruqi S, Molyneux ID, Fathi H, et al. Chronic cough and esomeprazole: a double-blind placebo-controlled parallel study. Respirology 2011;16:1150-6. [PubMed]


