Uniportal VATS: the first German experience
Introduction
The development of video-assisted thoracic surgery (VATS) over the past two decades has led to a significant shift in the management of an increasing number of thoracic pathologies. The procedure gained acceptance due to its clinical benefits in comparison to the conventional thoracic procedures, this is true too for the economic context (1-6). VATS is associated with less pain, decreased general complications and shorter hospital stay (7,8). VATS reduces surgical trauma and maintains the oncological principles of traditional open procedures (9). VATS leads to a fast postoperative recovery which allows the earlier administration of adjuvant therapy when necessary (10-13). A further development of the 2-3 trocar VATS with a utility incision for major lung resections is the uniportal VATS. The first description of this technique took place in 1998 and concerned a series of six patients, five wedge resections and one foreign bodies removal (14). This paved the way for the development of more complex uniportal procedures for a range of thoracic and mediastinal pathologies. This first progress of uniportal VATS was mainly pioneered by Prof. Gaetano Rocco from the National Cancer Institute, Naples, Italy. Between 2003 and 2006, uniportal VATS was performed for pleural effusion, pleurodesis, pleural and mediastinal biopsies, lung wedge resections, and mediastinal pathologies (15-17) A milestone was the first report on a major lung resection with radical lymphadenectomy for non-small cell lung cancer (NSCLC), by Dr. Gonzalez-Rivas from Coruña University Hospital in Spain (18), followed by complex uniportal VATS lung resections including pneumonectomy, segmentectomy, bronchoplastic procedures and chest wall resection (18-21). The latest development was a lobectomy in a non-intubated patient by uniportal VATS (22). The implementation of uniportal technique into the clinical practice is spreading globally. Especially, a strong trend in research and practice of uniportal VATS is ongoing in Asia (23). The initial clinical outcomes and short-term results are encouraging, and more long term data is awaited (23,24).
The purpose of this study was to critically analyze the first preliminary experience on uniportal VATS in Germany, in order to contextualize it internationally and understand its benefits and disadvantages.
Patients and methods
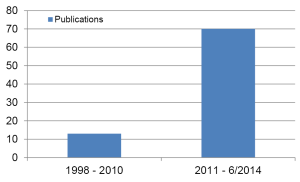
Between June 2012 and June 2014, a retrospective study from prospectively collected data was performed for patients undergoing a uniportal VATS procedure. 56 Patients were included in this study. The demographic data of the patients are present in Table 1. The first operations were performed together with Dr. Gonzalez-Rivas. This study was approved by the review board at the Charité - Universitätsmedizin Berlin and Charité Kompetenzzentrum für Thoraxchirurgie, and all patients provided written informed consent before operation. The main endpoint of this study was the feasibility of this technique for thoracic surgeons mainly performing a postero-lateral thoracotomy approach for major lung resections but experienced in minor VATS procedures. The outcome of uniportal VATS in terms of morbidity, 30 days mortality, conversion rate, operative time and hospital stay was studied.
Full table
Surgical technique
The patients were placed in a right or left sided position as for the postero-lateral thoracotomy but with modification of the arms’ position (Figure 1A). All procedures were performed under general anesthesia with single lung ventilation. The 3-5 cm single incision was placed in the 5th intercostal space. There was no rib spreading used. The 5 mm or 10 mm 30° scope camera was introduced in the upper part of the incision (Figure 1B). Nodule identification was performed through digital palpation under camera view in all cases where it was necessary. The incision allowed the introduction of more than two instruments beside the scope simultaneously. No additional skin incisions were made for any purpose such as placement of thoracoscope, graspers, or drains. A complete radical lymphadenectomy was performed in all patients with NSCLC. The surgeon and his assistant stand both in front of the patient. All tumor specimens were removed with an Endobag. At the end of the operation, one 24 or 20 Fr chest tube was inserted in the posterior part of the incision and was sutured to the anterior and posterior margins of the uniportal skin incision (Figure 1C). No additional incisions were made for the chest tube placement.

Postoperative management
The postoperative management applied an established Fast-Track concept of the thoracic surgery department. Most of the patients were admitted to an intermediate care unit and later on the same day to the normal ward. The mobilization and physiotherapy of the patients began on the operation day. Some of the patients received an epidural catheter while the others received an opiate pain medication. Thoracic X-ray was performed on the operation day and on the first postoperative day. The thoracic drainage was removed without clamping with normal X-ray findings, nor air leak and secretion below 200 mL within 24 hours. No patient was discharged with a chest tube in situ.
Statistical analysis
Parametric data are presented as mean values. SPSS v19 (SPSS Inc, Chicago, IL, USA) software was used and the significance level for all analyses was set at a P value of less than 0.05.
Results
Spectrum of the uniportal VATS
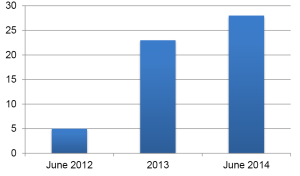
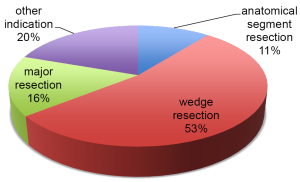
The uniportal VATS was introduced in the Charité department of thoracic surgery in June 2012 together with Dr. Gonzalez-Rivas. Until June 2014, there were 56 uniportal VAT procedures performed for different indications (Figure 2). There were 42 (75%) males and the mean age was 59.2±15 years. The 1 (41.1%), 2 (7.1%) and 3 (5.4%) wedge resections were the main procedures, being performed in 30 patients (53.6%). The 9 (16.1%) major lung resections included, 1 lower bilobectomy, 3 right upper, 4 right lower and 1 middle lobectomy. There were 6 (10.7%) anatomical one or more segment resections. The 11 (19.6%) other procedures included mainly pleurectomies, biopsies and lymphadenectomies (Figure 3). There were two conversions, in two cases of major resections. In one case the patient had a history of tuberculosis and there was a complete thoracic and mediastinal adhesion. In the other case, the lung resection was performed in a uniportal VATS technique but the lymphadenectomy was performed through a thoracotomy. In one anatomical segmentectomy the incision was enlarged, and a 12-cm thoracotomy with rib spreading was performed.
Operation time
The operation time was calculated from skin incision until wound closure. The operation time included also the time which was necessary for the frozen sections for histological examination. The median operation time for major lung resections, anatomical segment resections, wedge resections and others was 252, 114, 88 and 73 minutes, respectively.
Histology
In 14 (25%) of the patients, the histological finding was NSCLC. The other histological findings included different lung metastases, aspergillum, or no malignancy in 19 (33.9%), 2 (3.6%) and 21 (37.5%) of the patients, respectively. All tumors were completely resected (R0).
Perioperative morbidity and mortality
There were three revisions due to postoperative hemothorax. In two of these patients, a wedge resection was performed after adhesiolysis, and one of them was suffering from Child B liver cirrhosis while the other had previous heart transplantation and was under anti-coagulation due to lung artery embolism. The third patient had a severe pulmonary hypertonia and underwent a pleurectomy with adhesiolysis. In two patients, a postoperative pneumonia was noticed and successfully treated. One patient developed a pneumothorax after removal of the chest tube. In this patient, placement of a new thoracic drainage was necessary. Non-surgery related mortality was recorded on the 18th postoperative day by a patient who suffered from severe cardiac disease with preoperative ejection fraction of 10-15%.
Postoperative management
The thoracic drainage was removed with a secretion volume below 200 mL. The chest tube was removed after a mean of 3.4±2.1 days. Two postoperative lung fistulas were successfully treated conservatively. The mean hospital stay was 8.3±5.3 days.
Discussion
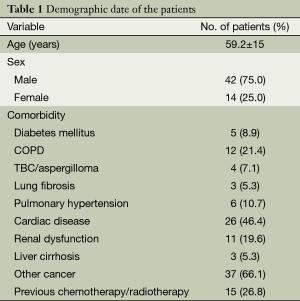
Uniportal VATS is becoming accepted worldwide for minor and major procedures to treat thoracic and mediastinal pathologies (23,24). The initial results are promising and the technical feasibility has been shown (24) To date, there are no results of randomized controlled trials to compare the role of minimally invasive techniques and open procedures. However, the non-randomized evidence has shown that minimally invasive techniques in thoracic surgery are feasible and associated with less postoperative morbidity and fast recovery allowing the begin of adjuvant therapy when necessary without delay (13,25,26). The 1 and 3 years survival of patients after VATS is at least equivalent to open procedures, with a trend towards better survival at 5 years with a VATS approach (7,8). Despite the 16 years experience with this technique, there were only 13 published cases with uniportal VATS until 2010. From 2011 till June 2014, there were 70 publications after the first report on Uniportal lobectomy (10) (Figure 4).
The uniportal VATS program was started at our institution in June 2012. The 3-port VATS was the standard procedure for minor procedures whereas the postero-lateral thoracotomy was the standard approach for major resections. The operations were performed according to the availability of the instruments and experience of the thoracic surgeon with a learning curve. Patient selection was not limited to low risk individuals. There were 1, 12, 38 and 5 patients with “The American Society of Anesthesiologists score” I, II, III and IV, respectively. Most of the patients had four or more comorbidities. This is reflected in the prolonged hospital stay despite the removal of the chest tube. A limiting factor was the unavailability of the special instruments for the technique with proximal and distal articulation as reported in other centers (20). Only four major lung resections were performed with these instruments while the other operations were performed with various endoscopic and conventional instruments. This resulted in a prolonged operation time. Certainly, the use of such instruments for retraction and dissection during uniportal VATS major lung resection is possible but far from optimal (23,27). Specifically designed uniportal VATS instruments are available with slight curvature and narrower shaft to allow for a smaller incision and reduced instrument fencing (19). All procedures were performed as pure uniportal VATS approach without the use muscle spreading. Only in one patient there was a use of an extra 5-mm port for the camera. Our report represents the first German experience with uniportal VATS in a heterogeneous group demonstrating feasibility with low conversion rate and morbidity.
Various technical aspects are of importance for the uniportal VATS. The procedure can be optimally learned under the supervision of a team experienced with it. The development of a uniportal VATS program requires special instrumentations and previous general experience in VATS and could be even performed by thoracic surgeons experienced in postero-lateral thoracotomy approach. Furthermore, randomized controlled studies are necessary to compare the uniportal VATS with other techniques in terms of lymph node dissection as well as mid and long term results, which will influence the future of uniportal VATS in Germany.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Garzon JC, Ng CS, Sihoe AD, et al. Video-assisted thoracic surgery pulmonary resection for lung cancer in patients with poor lung function. Ann Thorac Surg 2006;81:1996-2003. [PubMed]
- Date H, Yamashita M, Nagahiro I, et al. Living-donor lobar lung transplantation for primary ciliary dyskinesia. Ann Thorac Surg 2001;71:2008-9. [PubMed]
- Yim AP. VATS major pulmonary resection revisited--controversies, techniques, and results. Ann Thorac Surg 2002;74:615-23. [PubMed]
- Hazelrigg SR, Nunchuck SK, Landreneau RJ, et al. Cost analysis for thoracoscopy: thoracoscopic wedge resection. Ann Thorac Surg 1993;56:633-5. [PubMed]
- Van Schil P. Cost analysis of video-assisted thoracic surgery versus thoracotomy: critical review. Eur Respir J 2003;22:735-8. [PubMed]
- Lacin T, Swanson S. Current costs of video-assisted thoracic surgery (VATS) lobectomy. J Thorac Dis 2013;5 Suppl 3:S190-3. [PubMed]
- Sakuraba M, Miyamoto H, Oh S, et al. Video-assisted thoracoscopic lobectomy vs. conventional lobectomy via open thoracotomy in patients with clinical stage IA non-small cell lung carcinoma. Interact Cardiovasc Thorac Surg 2007;6:614-7. [PubMed]
- Sawada S, Komori E, Yamashita M, et al. Comparison in prognosis after VATS lobectomy and open lobectomy for stage I lung cancer: retrospective analysis focused on a histological subgroup. Surg Endosc 2007;21:1607-11. [PubMed]
- Park BJ. Is surgical morbidity decreased with minimally invasive lobectomy? Cancer J 2011;17:18-22. [PubMed]
- Gonzalez D, Delgado M, Paradela M, et al. Uni-incisional video-assisted thoracoscopic left lower lobectomy in a patient with an incomplete fissure. Innovations (Phila) 2011;6:45-7. [PubMed]
- Rocco G, Internullo E, Cassivi SD, et al. The variability of practice in minimally invasive thoracic surgery for pulmonary resections. Thorac Surg Clin 2008;18:235-47. [PubMed]
- Zhang Z, Zhang Y, Feng H, et al. Is video-assisted thoracic surgery lobectomy better than thoracotomy for early-stage non-small-cell lung cancer? A systematic review and meta-analysis. Eur J Cardiothorac Surg 2013;44:407-14. [PubMed]
- Teh E, Abah U, Church D, et al. What is the extent of the advantage of video-assisted thoracoscopic surgical resection over thoracotomy in terms of delivery of adjuvant chemotherapy following non-small-cell lung cancer resection? Interact Cardiovasc Thorac Surg 2014. [Epub ahead of print]. [PubMed]
- Yamamoto H, Okada M, Takada M, et al. Video-assisted thoracic surgery through a single skin incision. Arch Surg 1998;133:145-7. [PubMed]
- Rocco G, Martin-Ucar A, Passera E. Uniportal VATS wedge pulmonary resections. Ann Thorac Surg 2004;77:726-8. [PubMed]
- Jutley RS, Khalil MW, Rocco G. Uniportal vs standard three-port VATS technique for spontaneous pneumothorax: comparison of post-operative pain and residual paraesthesia. Eur J Cardiothorac Surg 2005;28:43-6. [PubMed]
- Rocco G, Brunelli A, Jutley R, et al. Uniportal VATS for mediastinal nodal diagnosis and staging. Interact Cardiovasc Thorac Surg 2006;5:430-2. [PubMed]
- Gonzalez-Rivas D, de la Torre M, Fernandez R, et al. Single-port video-assisted thoracoscopic left upper lobectomy. Interact Cardiovasc Thorac Surg 2011;13:539-41. [PubMed]
- Gonzalez-Rivas D. VATS lobectomy: surgical evolution from conventional VATS to uniportal approach. ScientificWorldJournal 2012;2012:780842.
- Gonzalez-Rivas D, Mendez L, Delgado M, et al. Uniportal video-assisted thoracoscopic anatomic segmentectomy. J Thorac Dis 2013;5:S226-33. [PubMed]
- Gonzalez-Rivas D, Delgado M, Fieira E, et al. Double sleeve uniportal video-assisted thoracoscopic lobectomy for non-small cell lung cancer. Ann Cardiothorac Surg 2014;3:E2. [PubMed]
- Gonzalez-Rivas D, Fernandez R, de la Torre M, et al. Single-port thoracoscopic lobectomy in a nonintubated patient: the least invasive procedure for major lung resection? Interact Cardiovasc Thorac Surg 2014. [Epub ahead of print]. [PubMed]
- Ng CS. Uniportal VATS in Asia. J Thorac Dis 2013;5:S221-5. [PubMed]
- Gonzalez-Rivas D, Fieira E, Delgado M, et al. Is uniportal thoracoscopic surgery a feasible approach for advanced stages of non-small cell lung cancer? J Thorac Dis 2014;6:641-8. [PubMed]
- Koizumi K, Haraguchi S, Hirata T, et al. Video-assisted lobectomy in elderly lung cancer patients. Jpn J Thorac Cardiovasc Surg 2002;50:15-22. [PubMed]
- Shiraishi T, Shirakusa T, Hiratsuka M, et al. Video-assisted thoracoscopic surgery lobectomy for c-T1N0M0 primary lung cancer: its impact on locoregional control. Ann Thorac Surg 2006;82:1021-6. [PubMed]
- Gonzalez-Rivas D, Paradela M, Fernandez R, et al. Uniportal video-assisted thoracoscopic lobectomy: two years of experience. Ann Thorac Surg 2013;95:426-32. [PubMed]