
Triglyceride to high-density lipoprotein cholesterol ratio as a risk factor of repeat revascularization among patients with acute coronary syndrome after first-time percutaneous coronary intervention
Introduction
Acute coronary syndrome (ACS) is a common fatal disease responsible for millions of deaths worldwide (1). In recent years, the prognosis of ACS patients has been dramatically improved due to the broad and early application of percutaneous coronary intervention (PCI), as well as innovations in pharmacotherapeutic regimes (2-6). Nevertheless, repeat revascularization due to in-stent restenosis (ISR) and plaque progression remains a relevant problem, which deteriorates the long-term outcomes of ACS patients (7-9). To improve the interventional efficacy, numerous modifications of drug-eluting stents (DES) and PCI procedure strategies have been developed, such as the utilization of biodegradable polymers and ultra-thin struts (10-12) and the double kissing crush technique (13,14). Meanwhile, it is of great clinical significance to identify high-risk ACS patients who may require repeat revascularization because these patients demand more intensive secondary prevention.
Dyslipidemia, including elevated triglycerides (TG), total cholesterol (TC), low-density lipoprotein cholesterol (LDL-C) or decreased high-density lipoprotein cholesterol (HDL-C), contributes to the increased risk of developing coronary artery disease (CAD) and has attracted tremendous attention from clinicians. Emerging evidence increasingly suggests that some indexes generated from lipid parameters (i.e., the TG/HDL-C ratio) possess advantages in stratifying the risk of cardiovascular disease compared to individual indexes, such as TG, TC, LDL-C, and HDL-C (15-17). The TG to HDL-C (TG/HDL-C) ratio, as an atherogenic index, has been highly correlated with myocardial infarction and coronary heart disease (18-20). Recently, accumulating studies support the use of the TG/HDL-C ratio as a prominent and accessible indicator of insulin resistance and metabolic syndrome (21,22). However, in the contemporary DES era, the predictive value of the TG/HDL-C ratio regarding repeat revascularization in ACS patients after a first-time successful PCI remains unclear.
The previous studies indicated that repeat revascularization events often occurred in the first year after DES (23). In this retrospective study, we analyzed the clinical characteristics of ACS patients who had coronary angiography performed during the period from 6 to 12 months after a first-time PCI, especially focused on the TG/HDL-C ratio, in order to identify the risk factors for a repeat PCI and enhance the long-term prognosis of ACS patients.
Methods
Study population
Consecutive ACS patients who had coronary angiography performed again during the period from 6 to 12 months after a first-time PCI from January 2014 and March 2019 in Zhongda Hospital were enrolled in the study. The inclusion criteria were: (I) ACS was the indication for the PCI procedure; (II) it was a first-time PCI; (III) the PCI procedure and DES implantation were successful; and (IV) informed consent was obtained from the patient. The exclusion criteria were: (I) the PCI procedure failed; (II) a previous history of angioplasty; (III) coronary angiography was not performed during the period from 6 to 12 months after a first-time PCI; and (IV) the patient failed to take the prescribed medications according to the doctor’s instructions during the follow-up period. According to the repeat PCI events, the patients were stratified into the event (+) group (n=101) and the event (−) group (n=170).
Data collection
Demographic data, medical history, and vital signs were accurately collected by the clinicians. Blood samples were obtained for laboratory analyses at admission. The laboratory results for erythrocyte, leukocyte, platelet, neutrophils, and lymphocyte counts, as well as random glucose, serum creatinine, TG, TC, LDL-C, and HDL-C, were obtained from the electronic medical record system. Ultrasonic cardiograms were performed before discharge.
PCI procedure and definition
All ACS patients were administrated a loading dose of 300 mg aspirin and a P2Y12 receptor inhibitor (300–600 mg clopidogrel or 180 mg ticagrelor) and were maintained with 100 mg of aspirin and 75 mg of clopidogrel daily or 90 mg of ticagrelor twice per day. PCI procedures were performed for any lesions in the presence of ischemic symptoms or objective ischemic signs and angiographic luminal diameter stenosis ≥50%, and any lesions with luminal diameter stenosis ≥70% by quantitative coronary angiography. PCI procedural decisions were made according to the consensus of three experienced operators. Beta-blockers, angiotensin-converting enzyme inhibitors (ACEIs) or angiotensin receptor blockers (ARBs) and statins were recommended during hospitalization and the follow-up period. A dual antiplatelet regimen was suggested for twelve months and all ACS patients who underwent PCI procedures were recommended to have a coronary angiography during the period from 6 to 12 months after their PCIs.
The primary outcome of the study was to identify the risk factors of repeat revascularization in ACS patients after a first-time successful PCI. A successful PCI procedure was defined as the achievement of final thrombolysis in myocardial infarction (TIMI) blood flow grade 3 with a residual luminal stenosis of less than 30%. Repeat revascularization events included target vessel revascularization (TVR) and de novo vessel revascularization (DVR). TVR was defined as repeat revascularization with a PCI in the previously treated vessel (24-27). DVR was defined as revascularization of the non-targeted coronary artery. Target lesion revascularization (TLR) was defined as repeat revascularization of the target vessel within the stented segment or the adjacent 5-mm region (24-27).
Statistical analyses
The normally distributed continuous variables are presented as means ± standard deviation. Student’s t-tests were applied to analyze the continuous variables. The categorical variables were compared using chi-squared tests. Fisher’s exact test was preferred when more than 25% of the values showed expected frequencies <5. Variables with P values <0.2 were entered into univariate or multivariate Cox proportional hazard model analysis. Hazard ratio (HR), 95% confidence interval (CI), and P value were used to evaluate the effects of the variables on repeat revascularization. All statistical analyses were two-tailed and performed with SPSS 21.0 (IBM Corporation, Armonk, NY, USA). Differences were statistically significant at P<0.05.
Results
Constitution of repeat revascularization events and baseline characteristics
According to the repeat PCI events, 271 patients were stratified into the event (+) group (n=101) and the event (−) group (n=170). In the event (+) group, TLR accounted for 20.79%, and TVR accounted for 50.49% of the patients. In contrast, DVR occurred in 52.47% of the ACS patients who received a repeat PCI, representing a significant proportion. The details are shown in Figure 1.
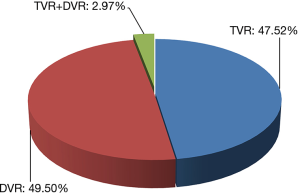
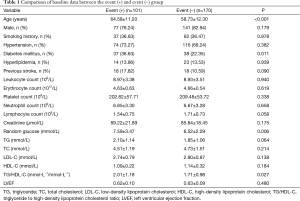
Table 1 shows the baseline characteristics of the ACS patients in the event (+) and event (−) groups. In the event (+) group, the patients were older [64.58±11.20 vs. 58.73±12.30 in the event (+) vs. event (−) group, respectively; P<0.001], more likely to have a history of diabetes mellitus [36.63% vs. 22.35%, in the event (+) vs. event (−) group, respectively; P=0.011]. Additionally, the random glucose concentrations and TG/HDL-C ratios in the event (+) group were higher than those in the event (−) group (7.59±3.47 vs. 6.52±2.29, P=0.006; and 2.01±1.18 vs. 1.71±0.98, P=0.027, respectively).
Full table
Characteristics of the interventional procedure and drug therapy
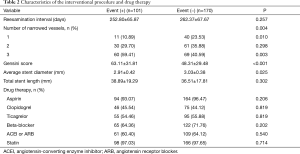
The reexamination intervals were similar between the two groups [252.80±65.87 vs. 262.37±67.67 in the event (+) vs. event (−) group, respectively; P=0.257]. In contrast to single-vessel disease, the percentage of patients with triple-vessel disease in the event (+) group was significantly higher than that in the event (−) group (59.41% vs. 40.59%, respectively; P=0.003). Accordingly, the Gensini scores were higher in the event (+) group [63.11±31.81 vs. 48.31±29.48, in the event (+) vs. event (−) group, respectively; P<0.001], indicating that patients in the event (+) group had more severe lesions. However, there was no significant difference in the use of medications, including aspirin, clopidogrel, ticagrelor, beta-blockers, ACEIs, ARBs, or statins, between the two groups of patients. The details are shown in Table 2.
Full table
Univariate and multivariate Cox proportional hazard model analysis
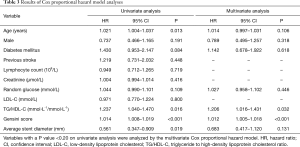
The univariate and multivariate Cox proportional hazard model analyses results are shown in Table 3. As a more meaningful scoring system for evaluating the severity of coronary lesions (28), Gensini scores were entered into the univariate Cox proportional hazard model analysis, instead of the number of narrowed vessels. Data from the univariate Cox proportional hazard model analysis suggested that age (HR =1.021, 95% CI: 1.004–1.037, P=0.013 for each age year higher), TG/HDL-C ratio (HR =1.237, 95% CI: 1.040–1.470, P=0.016 for each higher TG/HDL-C ratio unit), Gensini score (HR =1.014, 95% CI: 1.008–1.019, P<0.001 for each higher Gensini score unit), and average stent diameter (HR =0.561, 95% CI: 0.347–0.909, P=0.019 for each average stent diameter millimeter increased) were risk factors. After adjustment for the confounding factors (including age, male, diabetes mellitus, random glucose, TG/HDL-C ratio, Gensini score, and average stent diameter), the TG/HDL-C ratio (HR =1.206, 95% CI: 1.016–1.431, P=0.032 for each higher TG/HDL-C ratio unit) and Gensini score (HR =1.012, 95% CI: 1.005–1.018, P<0.001 for each higher Gensini score unit) remained independent risk factors for repeat revascularization in ACS patients after a first-time successful PCI.
Full table
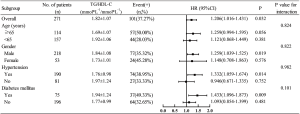
Subgroup analysis
As illustrated in Figure 2, the subgroup analysis showed that higher TG/HDL-C ratios were associated with a significantly higher risk of repeat PCIs in the male, hypertensive, and diabetes mellitus subgroups.
Discussion
In the present retrospective study, we evaluated the risk factors in the ACS population that required repeat revascularization. We validated for the first time that the TG/HDL-C ratio was independently associated with repeat PCIs in Chinese ACS patients, especially in the male, hypertensive, and diabetes mellitus subgroups.
As an epochal invention in the field of coronary interventional therapy, DES significantly decreases ISR by locally suppressing the inflammatory response and inhibiting the proliferation and migration of smooth muscles (29). However, repeat revascularizations are still required in certain PCI patients, not only due to ISR, but also the exacerbation of non-target lesions. Our data demonstrated that TLR accounts for 20.79% and DVR occurs in 52.47% of the ACS patients who received repeat PCIs. The results indicate that, with the upgrading of interventional instruments and continuous enhancement of cardiologists’ technology, the influence of PCI procedures on repeat revascularization is decreasing. The proportion of DVRs, which was more than 50%, suggests that intensive attention to modifying the risk factors for atherosclerosis exacerbation is warranted.
Individual factors in the PCI patients, such as age, gender, smoking, dyslipidemia, and diabetes mellitus, may significantly impact the need for repeat revascularization. In terms of the characteristics of the target lesions, the length and diameter of the diseased vessels, calcified lesions, and chronic totally occluded lesions are all related to target lesion failure (30). Our data showed that the Gensini score was positively correlated with repeat PCIs (HR =1.012, 95% CI: 1.005–1.018, P<0.001 for each higher Gensini score unit), which is consistent with previous conclusions (8). Undoubtedly, ACS patients with complex lesions require more intensive secondary prevention after a first-time PCI.
As an easily accessible parameter in routine clinical practice, the TG/HDL ratio may act as a powerful predictor for worse clinical outcomes and cardiovascular events. Turak et al. reported that high TG/HDL-C ratios were correlated with more fatal events and major adverse cardiovascular events (MACEs) in patients with essential hypertension (31). Several studies have suggested that an elevated TG/HDL-C is a useful predictor for future cardiovascular events in patients with diabetes mellitus or chronic kidney disease (32-34). Despite these findings, studies focusing on the relationship between TG/HDL-C ratios and repeat PCIs in the Chinese population are scarce. In this study, we showed that the TG/HDL-C ratio was an independent predictor of repeat revascularization in Chinese ACS patients after first-time PCIs (HR =1.206, 95% CI: 1.016–1.431, P=0.032 for each higher TG/HDL-C ratio unit). Although the underlying mechanisms have not been clearly elucidated, certain speculations for how the TG/HDL-C ratio predicts a repeat PCI can be made. First, the simultaneous application of TG and HDL-C in the ratio reflects the balance between atherogenic and protective lipoproteins and could be effective for evaluating plasma atherogenicity (35,36). Second, certain research has validated that the TG/HDL-C ratio could serve as a surrogate marker of insulin resistance, which contributes to the progression of coronary atherosclerosis (21,37,38). In addition, in spite of no direct evidence, a correlation between inflammation and the TG/HDL-C ratio has been reasonably suggested (31,34). Therefore, in theory, combining TG and HDL-C to create a ratio may be a better way to estimate the risk of repeat revascularization.
Certain limitations should be claimed here. First, this retrospective cohort study could not avoid case selection bias. Second, our study sample was from a single center and relatively small. The findings should be confirmed with further multicenter studies. Third, some factors which may influence the requirement for repeat revascularization were not included, since they were not measured in every patient.
Conclusions
In conclusion, DVR accounts for a significant proportion of ACS patients who received repeat PCIs. Therefore, intensive attention to modifying the risk factors for atherosclerosis exacerbation is warranted. After adjustment for confounding factors, the TG/HDL-C ratio and Gensini score remain independent risk factors of repeat revascularization in ACS patients after first-time successful PCIs.
Acknowledgments
Funding: This work is supported by grants from Jiangsu Provincial Key Medical Discipline (Laboratory) (No. ZDXKA2016023) and Jiangsu Provincial Key Research and Development Program (No. BE2016785).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was approved by the IEC for Clinical Research of Zhongda Hospital, Affiliated to Southeast University (No. 2017ZDSYLL023-P01).
References
- Feinberg J, Nielsen EE, Greenhalgh J, et al. Drug-eluting stents versus bare-metal stents for acute coronary syndrome. Cochrane Database Syst Rev 2017;8:CD012481. [PubMed]
- Neumann FJ, Sousa-Uva M, Ahlsson A, et al. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur Heart J 2019;40:87-165. [Crossref] [PubMed]
- Roffi M, Patrono C, Collet JP, et al. 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: Task Force for the Management of Acute Coronary Syndromes in Patients Presenting without Persistent ST-Segment Elevation of the European Society of Cardiology (ESC). Eur Heart J 2016;37:267-315. [Crossref] [PubMed]
- Levine GN, Bates ER, Bittl JA, et al. 2016 ACC/AHA Guideline Focused Update on Duration of Dual Antiplatelet Therapy in Patients With Coronary Artery Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol 2016;68:1082-115. [Crossref] [PubMed]
- Ibanez B, James S, Agewall S, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J 2018;39:119-77. [Crossref] [PubMed]
- Anantha-Narayanan M, Anugula D, Gujjula NR, et al. Bivalirudin versus heparin in percutaneous coronary intervention-a systematic review and meta-analysis of randomized trials stratified by adjunctive glycoprotein IIb/IIIa strategy. J Thorac Dis 2018;10:3341-60. [Crossref] [PubMed]
- Karjalainen PP, Nammas W, Ylitalo A, et al. Long-term clinical outcome of titanium-nitride-oxide-coated stents versus everolimus-eluting stents in acute coronary syndrome: Final report of the BASE ACS trial. Int J Cardiol 2016;222:275-80. [Crossref] [PubMed]
- Brener SJ, Ertelt K, Mehran R, et al. Predictors and impact of target vessel revascularization after stent implantation for acute ST-segment elevation myocardial infarction: lessons from HORIZONS-AMI. Am Heart J 2015;169:242-8. [Crossref] [PubMed]
- Piccolo R, Niglio T, Franzone A, et al. Novel treatments for in-stent restenosis: sirolimus-eluting balloons enter the arena. J Thorac Dis 2018;10:628-30. [Crossref] [PubMed]
- Zaman A, de Winter RJ, Kogame N, et al. Safety and efficacy of a sirolimus-eluting coronary stent with ultra-thin strut for treatment of atherosclerotic lesions (TALENT): a prospective multicentre randomised controlled trial. Lancet 2019;393:987-97. [Crossref] [PubMed]
- de Winter RJ, Katagiri Y, Asano T, et al. A sirolimus-eluting bioabsorbable polymer-coated stent (MiStent) versus an everolimus-eluting durable polymer stent (Xience) after percutaneous coronary intervention (DESSOLVE III): a randomised, single-blind, multicentre, non-inferiority, phase 3 trial. Lancet 2018;391:431-40. [Crossref] [PubMed]
- Lupi A, Schaffer A, Bongo AS. Should ultrathin strut drug eluting stents be considered the new benchmark for novel coronary stents approval? The complex interplay between stent strut thickness, polymeric carriers and antiproliferative drugs. J Thorac Dis 2018;10:678-81. [Crossref] [PubMed]
- Chen SL, Zhang JJ, Han Y, et al. Double Kissing Crush Versus Provisional Stenting for Left Main Distal Bifurcation Lesions: DKCRUSH-V Randomized Trial. J Am Coll Cardiol 2017;70:2605-17. [Crossref] [PubMed]
- Chen SL, Santoso T, Zhang JJ, et al. A randomized clinical study comparing double kissing crush with provisional stenting for treatment of coronary bifurcation lesions: results from the DKCRUSH-II (Double Kissing Crush versus Provisional Stenting Technique for Treatment of Coronary Bifurcation Lesions) trial. J Am Coll Cardiol 2011;57:914-20. [Crossref] [PubMed]
- Kawakami R, Matsumoto I, Shiomi M, et al. Role of the Low-Density Lipoprotein-Cholesterol/High-Density Lipoprotein-Cholesterol Ratio in Predicting Serial Changes in the Lipid Component of Coronary Plaque. Circ J 2017;81:1439-46. [Crossref] [PubMed]
- Zhong Z, Hou J, Zhang Q, et al. Assessment of the LDL-C/HDL-C ratio as a predictor of one year clinical outcomes in patients with acute coronary syndromes after percutaneous coronary intervention and drug-eluting stent implantation. Lipids Health Dis 2019;18:40. [Crossref] [PubMed]
- Wen J, Huang Y, Lu Y, et al. Associations of non-high-density lipoprotein cholesterol, triglycerides and the total cholesterol/HDL-c ratio with arterial stiffness independent of low-density lipoprotein cholesterol in a Chinese population. Hypertens Res 2019;42:1223-30. [Crossref] [PubMed]
- Gaziano JM, Hennekens CH, O'Donnell CJ, et al. Fasting triglycerides, high-density lipoprotein, and risk of myocardial infarction. Circulation 1997;96:2520-5. [Crossref] [PubMed]
- da Luz PL, Favarato D, Faria-Neto JR Jr, et al. High ratio of triglycerides to HDL-cholesterol predicts extensive coronary disease. Clinics (Sao Paulo) 2008;63:427-32. [PubMed]
- Hadaegh F, Khalili D, Ghasemi A, et al. Triglyceride/HDL-cholesterol ratio is an independent predictor for coronary heart disease in a population of Iranian men. Nutr Metab Cardiovasc Dis 2009;19:401-8. [Crossref] [PubMed]
- Ren X, Chen ZA, Zheng S, et al. Association between Triglyceride to HDL-C Ratio (TG/HDL-C) and Insulin Resistance in Chinese Patients with Newly Diagnosed Type 2 Diabetes Mellitus. PLoS One 2016;11:e0154345. [Crossref] [PubMed]
- Shin HG, Kim YK, Kim YH, et al. The Relationship between the Triglyceride to High-Density Lipoprotein Cholesterol Ratio and Metabolic Syndrome. Korean J Fam Med 2017;38:352-7. [Crossref] [PubMed]
- Al Muradi H, Mehra A, Okolo J, et al. Clinical presentation and predictors of target vessel revascularization after drug-eluting stent implantation. Cardiovasc Revasc Med 2012;13:311-5. [Crossref] [PubMed]
- Ahn JM, Roh JH, Kim YH, et al. Randomized Trial of Stents Versus Bypass Surgery for Left Main Coronary Artery Disease: 5-Year Outcomes of the PRECOMBAT Study. J Am Coll Cardiol 2015;65:2198-206. [Crossref] [PubMed]
- Li SJ, Ge Z, Kan J, et al. Cutoff Value and Long-Term Prediction of Clinical Events by FFR Measured Immediately After Implantation of a Drug-Eluting Stent in Patients With Coronary Artery Disease: 1- to 3-Year Results From the DKCRUSH VII Registry Study. JACC Cardiovasc Interv 2017;10:986-95. [Crossref] [PubMed]
- Kirtane AJ, Yeung AC, Ball M, et al. Long-term (5-year) clinical evaluation of the Resolute zotarolimus-eluting coronary stent: The RESOLUTE US clinical trial. Catheter Cardiovasc Interv 2019. [Epub ahead of print]. [Crossref] [PubMed]
- Hommels TM, Hermanides RS, Rasoul S, et al. Everolimus-eluting bioresorbable scaffolds for treatment of coronary artery disease in patients with diabetes mellitus: the midterm follow-up of the prospective ABSORB DM Benelux study. Cardiovasc Diabetol 2019;18:25. [Crossref] [PubMed]
- Gensini GG. A more meaningful scoring system for determining the severity of coronary heart disease. Am J Cardiol 1983;51:606. [Crossref] [PubMed]
- Dangas GD, Claessen BE, Caixeta A, et al. In-stent restenosis in the drug-eluting stent era. J Am Coll Cardiol 2010;56:1897-907. [Crossref] [PubMed]
- Konigstein M, Madhavan MV, Ben-Yehuda O, et al. Incidence and predictors of target lesion failure in patients undergoing contemporary DES implantation-Individual patient data pooled analysis from 6 randomized controlled trials. Am Heart J 2019;213:105-11. [Crossref] [PubMed]
- Turak O, Afşar B, Ozcan F, et al. The Role of Plasma Triglyceride/High-Density Lipoprotein Cholesterol Ratio to Predict New Cardiovascular Events in Essential Hypertensive Patients. J Clin Hypertens (Greenwich) 2016;18:772-7. [Crossref] [PubMed]
- Yang SH, Du Y, Li XL, et al. Triglyceride to High-Density Lipoprotein Cholesterol Ratio and Cardiovascular Events in Diabetics With Coronary Artery Disease. Am J Med Sci 2017;354:117-24. [Crossref] [PubMed]
- Sonmez A, Yilmaz MI, Saglam M, et al. The role of plasma triglyceride/high-density lipoprotein cholesterol ratio to predict cardiovascular outcomes in chronic kidney disease. Lipids Health Dis 2015;14:29. [Crossref] [PubMed]
- Kim JS, Kim W, Woo JS, et al. The Predictive Role of Serum Triglyceride to High-Density Lipoprotein Cholesterol Ratio According to Renal Function in Patients with Acute Myocardial Infarction. PLoS One 2016;11:e0165484. [Crossref] [PubMed]
- Millán J, Pintó X, Muñoz A, et al. Lipoprotein ratios: Physiological significance and clinical usefulness in cardiovascular prevention. Vasc Health Risk Manag 2009;5:757-65. [PubMed]
- Dobiásová M. Atherogenic index of plasma [log(triglycerides/HDL-cholesterol)]: theoretical and practical implications. Clin Chem 2004;50:1113-5. [Crossref] [PubMed]
- McLaughlin T, Abbasi F, Cheal K, et al. Use of metabolic markers to identify overweight individuals who are insulin resistant. Ann Intern Med 2003;139:802-9. [Crossref] [PubMed]
- Kim JS, Kang HT, Shim JY, et al. The association between the triglyceride to high-density lipoprotein cholesterol ratio with insulin resistance (HOMA-IR) in the general Korean population: based on the National Health and Nutrition Examination Survey in 2007-2009. Diabetes Res Clin Pract 2012;97:132-8. [Crossref] [PubMed]


