Palliative stent graft placement combined with subsequent open surgery for retrograde ascending dissection intra-thoracic endovascular aortic repair
Introduction
Thoracic endovascular aortic repair (TEVAR) is a safe and effective alternative to traditional open surgery for uncomplicated type B dissections (1). Retrograde ascending dissection (RAD) is a life-threatening complication that may occur on intra- or post-TEVAR. And RAD intra-TEVAR is extremely rare on clinic (2,3). In this case, we report a case management for a patient with RAD intra-TEVAR.
Case report
A 48-year-old Chinese man presented an acute severe chest pain with back irradiation and was sent to the local hospital at the onset of symptoms. He had a history of severe hypertension for four years. And no other positive medical history was reviewed. Computed tomography angiography (CTA) revealed Stanford type B aortic dissection with a site of entry tear at 2 cm upon the origin of renal artery. TEVAR was chosen to perform for this patient on emergency. However, acute RAD occurred before stent grafts placement. The retrograde dissection expanded to the middle of ascending aorta, with a new entry tear near the origin of left subclavian artery (LSCA).
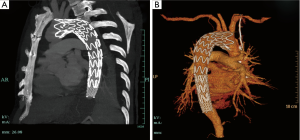
Given that the local hospital lacked cardiac surgery department, a distal bare stent restraint combined with proximal covered stent was then palliatively placed to cover the new entry tear, which kept from further retrograde dissection. After TEVAR, the patient felt symptom alleviation, but a little bit dizzy and amaurosis. CTA revealed that proximal part of stent graft covered the origins of LSCA and left common carotid (LCC) (Figure 1). He was then transferred to Zhongshan Hospital Fudan University for an open surgery on emergency. After induction of general anesthesia, the right axillary artery is exposed through a right subclavian incision as routinely used for cardiopulmonary bypass (CPB) and antegrade selective cerebral perfusion. And the femoral artery was cannulated in addition to the axillary artery cannulation. An arterial cannula is inserted into the right axillary artery, and a dual-stage caval cannula is inserted into the right atrium. The CPB flow is maintained between 2.2 and 2.4 L/min/m2, and the patient was cooled to a rectal temperature of 20 °C. During the cooling period, the ascending aorta is cross-clamped and the heart is arrested with cold blood cardioplegia. The brain is perfused through the right axillary artery at a flow rate of 5 to 10 mL/kg/min. Through the transverse incision of the ascending aorta, we found the ascending aorta dissection with a diameter of 55 mm, and confirmed that the proximal part of stent graft covered the new entry tears, as well as origins of LSCA and LCC. We cut off the dissection part of ascending aorta, aorta arch and proximal part of stent graft. A triple-branched artificial vessel was one by one sutured to the stent graft, aortic branches and ascending aorta. The CPB time was 189 minutes with aortic cross-clamp time of 117 minutes and cerebral perfusion of 30 minutes. The patient recovered well, and was discharged after 2 weeks.
Discussion
Published literatures have identified RAD as a lethal complication of TEVAR for all indications with an estimate of 1.3% to 6.8% (1-3). Given the recent evidence, this complication may be associated with the procedure or device, or as a result of natural progression of aorta disease. Potential risk factors for RAD include the following: (I) proximal stent graft with a free-flow bare spring; (II) endoleak at the proximal fixation site leading to retrograde enlargement of the false lumen; (III) passive bending of TEVAR at the arch with over-stenting of the LSCA leading to spring-back strength, which could yield stress on the greater curve of arch; (IV) wire and sheath handling or balloon dilatation during the endovascular procedure might trigger the intimal damage in the extremely fragile aortic wall; and (V) patients with connective tissue disorders such as Marfan, Ehlers-Danlos, and Loeys-Dietz syndromes (4-7).
The median interval between TEVAR and repair of retrograde dissection was 6 months. RAD intra-TEVAR is extremely rare on clinic (8). In our case, RAD occurred acutely before stent graft placement. The new entry tear led to the expansion of retrograde dissection with ascending aorta involved. We assumed that the introduction of guide wire and sheath handling during the endovascular procedure might injury the fragile and vulnerable aortic wall and result in acute RAD.
RAD is an emergency that requires surgical repair. And expanded dissection may result in the subsequently lethal aortic rupture (9). In the present case, cardiac surgery was unable to be done in the local hospital. Therefore, palliative TEVAR was performed alternatively, which aimed to cover the new entry tear and blocked further expansion of ascending dissection before the open surgery. The strategy earned time for transfer and reduced risk of death. And it could be applied in this specific situation. However, this strategy may result in the risk of coverage for branched artery origins, which may subsequently lead to cerebral ischemia. Therefore, lack of cardiac surgery department in a hospital posed difficulties for the management of a RAD patient. All contingency plans should be arranged before TEVAR, including standby of cardiac surgeons and operation room.
The operative strategies regarding the rescue of RAD are similar to those for acute type A dissection. The reverse frozen elephant trunk procedure or total arch replacement were the preferred choices for patients with a dissection tear involving the arch, and ascending and hemi-arch repair was sufficient in patients with the dissection limited to the proximal aorta (8-10). In this case, we chose to perform total arch replacement during the open surgery. We cut off proximal part of the stent graft and sutured the distal end of artificial vessel to the remaining stent graft, which could work as reverse elephant trunk technique.
Conclusions
In conclusion, we consider palliative TEVAR associated with open surgery may enable a novel strategy for acute RAD during endovascular procedure for hospital that is lack of cardiac surgery department. And emergency surgical repair is still the best choice for all patients.
Acknowledgements
This work was supported by a grant from the National Key Technologies R & D Program of China during the Twelfth Five-Year Plan Period (No. 2011BA11B20).
Disclosure: The authors declare no conflict of interest.
References
- Dake MD, Kato N, Mitchell RS, et al. Endovascular stent-graft placement for the treatment of acute aortic dissection. N Engl J Med 1999;340:1546-52. [PubMed]
- Dong ZH, Fu WG, Wang YQ, et al. Retrograde type A aortic dissection after endovascular stent graft placement for treatment of type B dissection. Circulation 2009;119:735-41. [PubMed]
- Eggebrecht H, Thompson M, Rousseau H, et al. Retrograde ascending aortic dissection during or after thoracic aortic stent graft placement: insight from the European registry on endovascular aortic repair complications. Circulation 2009;120:S276-81. [PubMed]
- Kische S, Ehrlich MP, Nienaber CA, et al. Endovascular treatment of acute and chronic aortic dissection: midterm results from the Talent Thoracic Retrospective Registry. J Thorac Cardiovasc Surg 2009;138:115-24. [PubMed]
- Williams JB, Andersen ND, Bhattacharya SD, et al. Retrograde ascending aortic dissection as an early complication of thoracic endovascular aortic repair. J Vasc Surg 2012;55:1255-62. [PubMed]
- Neuhauser B, Greiner A, Jaschke W, et al. Serious complications following endovascular thoracic aortic stent-graft repair for type B dissection. Eur J Cardiothorac Surg 2008;33:58-63. [PubMed]
- Svensson LG, Kouchoukos NT, Miller DC, et al. Expert consensus document on the treatment of descending thoracic aortic disease using endovascular stent-grafts. Ann Thorac Surg 2008;85:S1-41. [PubMed]
- Idrees J, Arafat A, Johnston DR, et al. Repair of retrograde ascending dissection after descending stent grafting. J Thorac Cardiovasc Surg 2014;147:151-4. [PubMed]
- Li B, Pan XD, Ma WG, et al. Stented elephant trunk technique for retrograde type A aortic dissection after endovascular stent graft repair. Ann Thorac Surg 2014;97:596-602. [PubMed]
- Lu S, Lai H, Wang C, et al. Surgical treatment for retrograde type A aortic dissection after endovascular stent graft placement for type B dissection. Interact Cardiovasc Thorac Surg 2012;14:538-42. [PubMed]


