Implementing clinical guidelines for chronic obstructive pulmonary disease: barriers and solutions
Introduction
Chronic obstructive pulmonary disease (COPD) is a complex lung disease that is characterised by progressive worsening of airflow limitation, punctuated with acute exacerbations that if severe, frequently require hospitalisation (1). COPD is the third leading cause of mortality worldwide (2). Several evidence-based guidelines for the diagnosis and management of COPD are available to clinicians, including the GOLD guidelines internationally and the COPD-X Plan: Australian and New Zealand Guidelines for the management of COPD. Although they are widely available, the knowledge and implementation of these guidelines are highly variable in actual clinical practice. Many barriers to the implementation of management guidelines by clinicians have been identified (3), but relatively few studies have investigated methods for enhancing the use of guidelines. This review explores these critical issues, gaining insight from efforts in clinical guidelines for other chronic diseases, and applying these principles to improving uptake of the COPD guidelines amongst clinicians.
Benefits of adhering to clinical recommendations contained in guidelines for COPD
The goals of therapy in COPD are to reduce symptoms and improve quality of life, and reduce future risk of adverse outcomes including exacerbations, hospitalisations and mortality. The evidence base for achieving these goals are encapsulated in international (1) and national clinical guidelines available throughout the world. By following these guidelines, clinicians will ensure that they are translating the best available evidence into their everyday clinical practice.
Spirometry is the gold standard diagnostic test to confirm fixed airflow limitation in individuals with dyspnoea, chronic cough or sputum production, and risk factors for COPD (1). Spirometric diagnosis of COPD at any stage is an essential step to ensure an accurate diagnosis and to guide therapy (4). The benefits from using non-pharmacological therapies in COPD are substantial—smoking cessation reduces lung function decline (5), influenza and pneumococcal vaccination decrease the risks of these infections (6,7), and pulmonary rehabilitation improves quality of life, increases exercise tolerance and reduces frequency of hospitalisations (8,9). In addition, pharmacological therapies provide benefit for patients, with long-acting bronchodilators (10-15) and inhaled corticosteroids (16) acting to reduce dyspnoea, improve quality of life and lung function, decrease risk of exacerbations and possibly reduce mortality (17). Early recognition and appropriate treatment of acute exacerbations with bronchodilators, systemic corticosteroids and antibiotics, where appropriate, reduce symptoms, shorten time to recovery and reduce risk of relapse (18,19).
Preparation of evidence-based clinical guidelines: the Australian COPD-X guidelines as an example
Many national guidelines have been written and adapted for use in specific countries. In the process of evidence-based guideline development, it is particularly important that the developers regularly review and critically appraise the evidence, to ensure that the guidelines are up-to-date, high quality, clinically relevant and beneficial to healthcare professionals and patients (20). As an example, many of us have been involved in the Australian COPD-X clinical guidelines developed by Lung Foundation Australia. COPD-X stands for Case detection and Confirm diagnosis, Optimise function, Prevent deterioration, Develop management plan of care, and manage eXacerbations. These guidelines were initially published in 2003 in the Medical Journal of Australia (21) and an update was published in 2006 (22). Since then, regular updates have been available on a dedicated website administered by the Lung Foundation (www.copdx.org.au), with the latest version (2.37) recently published online.
The guidelines are prepared by the Lung Foundation Australia’s COPD Guidelines Committee, which consists of eight clinical members plus executive administrative support. Conflict of interest statements from each Committee member are recorded on an annual basis and published on the COPD-X website. The Committee meets quarterly to appraise the latest published evidence and make recommendations on updating the guidelines. Prior to each meeting, searches are carried out in the Cochrane Database of Systematic Reviews, Database of Abstracts of Reviews of Effects and PubMed, using detailed search strategies (available on request) which include COPD and emphysema as key words.
At each meeting, search results are discussed to decide whether full papers should be obtained for review. At the subsequent meeting, committee members discuss their appraisal of the papers reviewed and recommend whether the papers should be cited in the guidelines, with any additional form of wording included. After an approval process, Lung Foundation Australia publishes online updates of COPD-X (typically two updates per year) to include the changes agreed at recent meetings of the Committee. An email is sent to all the registered users of the COPD-X website informing them when an update has been made and what changes have occurred. A COPD-X Concise Guide for Primary Care, based on the full guidelines, will be released by Lung Foundation Australia in November 2014 (www.copdx.org.au
Low concordance with guideline recommendations
A major issue is low awareness of clinical guidelines, which may subsequently translate into low adherence to guideline recommendations, and potentially suboptimal clinical care for patients in primary, secondary and tertiary care. Even with detailed processes for preparation and implementation of guidelines, such as the Australian COPD-X guidelines above, observational studies suggest that clinician knowledge of management guidelines is relatively low world-wide, both for chronic diseases generally and specifically for COPD.
Chronic disease guidelines
Many lessons can be learned from use of clinical guidelines in chronic diseases other than COPD, and applied in principle to COPD guidelines. As examples, comparison of studies examining chronic disease management reveals that many cardiovascular-related guidelines are largely adhered to; however, lower adherence has been generally observed to guidelines for metabolic diseases such as diabetes and osteoporosis (23-28).
Cardiovascular disease
In general, good adherence has been observed for cardiovascular disease guidelines (23,24). For hypertension, a study of 410 physicians in Finland found an 89% adherence rate to the guidelines, and that implementation improved in larger centres with more structured health care systems (24). Another study of general practitioners (GPs) in Austria found 83% adherence to cardiovascular disease and diabetes guidelines (23). However, when non-adherence occurred, factors included lack of familiarity with guidelines, even after education, and disagreement with guideline treatment recommendations (23,26,28,29).
Metabolic diseases
In general, rates of adherence to guidelines in the management of metabolic diseases have been observed to be relatively low. Studies of adherence to guidelines for screening of gestational diabetes found very low rates of adherence in obstetric units in France (25) and Canada (26). Factors identified included lack of familiarity with new guidelines, unfamiliar screening measures, poor acceptance and feasibility, difficulty with administration of recommendations, patient non-adherence, and ambiguity in guideline recommendations (25,26). Additionally, a retrospective survey of 200 GP referral letters to a hospital in Scotland showed that the introduction of local type 2 diabetes guidelines had no significant effect on screening for patient complications, or on GP referral letter content about complications of diabetes (27). In a survey of Canadian GPs, 35% of respondents had not read or been aware of the latest osteoporosis guidelines (28).
Though many guidelines for chronic diseases have been carefully developed, relatively low adherence to guideline recommendations—particularly for metabolic disease but less so for cardiovascular diseases—may result in suboptimal healthcare. Many barriers to adherence with chronic disease guidelines have been identified, as outlined for the examples above. Hence to improve adherence to guidelines, research has focused on strategies to target health professional education, decision-making algorithms (including electronic systems), and reminders at the time of consultation, and continuous quality assurance programmes.
COPD guidelines
Correct diagnosis and subsequent appropriate treatment selection have been the most common areas of deficiency identified in adherence to COPD guidelines. Most studies have focused on outpatient management of COPD, particularly primary care. A cross-sectional study of 455 primary care physicians and 243 physicians practicing in a hospital system, published in 2004, found that only 55% of Swiss physicians used spirometry in the diagnosis of COPD, and only one-third knew the GOLD criteria for COPD (30). Knowledge of the indications for use of inhaled steroids and referral to pulmonary rehabilitation were also low. A recent cross-sectional study of 593 GPs in Shanghai found that whilst 55% of GPs recognized the different severity classifications, only 8% of patients with COPD received prescriptions in accordance with GOLD guidelines (31). Thus, although COPD guidelines are widely available and accessible in print and online, studies suggest that clinician awareness of their specific recommendations is generally low, despite many efforts for their implementation and dissemination.
Several studies in COPD have demonstrated that actual clinical practice may deviate significantly from guideline recommendations (Table 1). A retrospective study of 450 outpatients with stable COPD in the US (33) found that 56% of patients received guideline-concordant pharmacotherapy, based on the 2007 GOLD guidelines available at that time (35). There was a significant relationship between suboptimal treatment and adverse outcomes: patients who received guideline-discordant treatment had nearly twice the number of exacerbations as those who received guideline-concordant care. A cross-sectional study of 1,517 primary care patients with COPD in the US found that 27% of patients had spirometry documented within the previous year, 25% had comorbid conditions appropriately managed, and 32% had appropriate measures in place for risk reduction (34). In a Swiss study, GP prescription of long-acting bronchodilators or inhaled steroids was guideline-concordant in only 20% of patients with GOLD spirometry stage I and II COPD, whereas 64% of patients with more severe stage III and IV COPD received guideline-concordant treatment (32). Finally, a retrospective study of 1,185 patients with moderate to severe COPD in Slovenia found that those who died during follow-up were more often found to have experienced suboptimal management according to guidelines when compared to patients who were alive at the end of the follow up period (including less long-acting inhaled medicine prescribed by their medical practitioners) (36). Overall, these findings support the value of guideline-based care in improving patient outcomes in COPD, and clearly demonstrate areas of practice that can be enhanced.
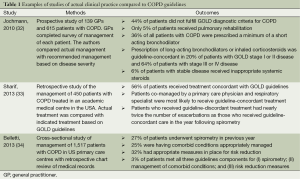
Full table
Barriers to guideline adherence
Specific barriers to adherence to COPD guidelines have been identified in observational studies. In one study of 154 general internists in the US, factors associated with reduced concordance with clinical guideline recommendations included low familiarity with COPD guidelines, perceived low self-efficacy for use of guidelines, and time constraints (37). In another US study, only 32% of 500 primary care physicians reported high familiarity with the GOLD COPD guidelines (38). In comparison, a larger proportion (76%) of the same group of physicians rated themselves as very familiar with guidelines for management of hypertension, indicating a relative disparity in awareness of guidelines for these two common chronic conditions. A qualitative Australian study, using semi-structured interviews of nine hospital-based registrars or interns, and seven GPs, found that barriers to implementation of evidence-based recommendations for COPD included lack of supportive enablers and complexity of the behavioural change needed in their patients (39).
Approaches to improving adherence to guidelines
Improving adherence to chronic disease guidelines
A number of methods of improving guideline implementation have been investigated in chronic diseases other than COPD that could feasibly be applied to COPD guidelines.
Distribution of guidelines
Having knowledge itself does not necessarily translate to clinical practice; therefore implementation and distribution strategies must be utilised. Use of brief summaries or storyboards of guidelines posted in clinical areas are associated with a positive impact on provider knowledge (40). Other distribution methods include mailing guidelines directly to clinicians or generating publicity prior to guideline publication (41). The act of voluntarily downloading guidelines also demonstrated active participation and greater likelihood that the guidelines would be considered useful.
Clinician professional development
Continuing medical development is another commonly used method with the aim to increase clinician adherence to guidelines. A study of infection management found a significant improvement in compliance with infection control protocols after active education when compared to no intervention (42). A third arm, the passive intervention group where education material was offered but not actively made available, resulted in only 34% of participants engaging in education, compared to the 91% in the active group. However, studies of diabetes care and lower back pain management showed no significant difference in guideline adherence after an educational program (43,44). A Cochrane review of 81 studies found that continuing medical development meetings can lead to a small improvement in practice and patient outcomes (45). Factors associated with effective educational meetings were higher attendance rates and a mix of didactic and interactive sessions.
Electronic health records (EHR)
EHR usage has been associated with improved provider knowledge (40). However, in a 2-year study comparing the EHR to non-EHR primary care practices, there was no significant difference in adherence to diabetes management guidelines between these two groups. In other studies of diabetes management before and after implementation of EHRs, EHRs have been demonstrated to improve attainment of healthcare management standards. For example, EHR implementation increased rates of patients with diabetes having their glycated haemoglobin (HbA1c) level checked at the appropriate intervals, being prescribed antihypertensive medication when indicated, and receiving pneumococcal vaccination (46). EHRs have also been shown to improve treatment intensification following abnormal HbA1c levels (47), and reduce both emergency department (ED) visits and hospitalisations in patients with diabetes (48).
The cost efficiency of EHRs is still controversial, and there are many factors to consider regarding their use. Ultimately, EHRs will be most successful when they can meet the needs of physicians and their patients, promote quality care, and maximise efficiency (49).
Reminders about guideline recommendations
Having guidelines in a readily accessible manner, when they are required at point-of-care, has been shown to improve guideline adherence (50). Similarly, establishing checkpoints, deadlines or cues during a consultation has been associated with improved provider knowledge (40). This has been found to be effective in increasing guideline adherence, which could then be translated into significantly improved patient quality of life (51,52). Reminders have been associated with positive clinician behavioural change, since relevant information is being presented during the clinical decision-making process (28,53). A Cochrane review of 32 studies found that computer-generated reminders for tasks such as ordering screening tests or giving vaccinations provided to clinicians on paper resulted in a median 11% improvement in process of care measures compared to usual care (54).
Though the reminder system has proven to be effective, it has been suggested that physician perception of the benefit of the reminder may also influence their usage. One study has shown that prompts perceived to be regulatory and for enforcement will be used less than prompts perceived to be for guidance (55). A Cochrane review of audit and feedback systems for clinicians found that the success of such programs depends on several factors (56). Characteristics associated with behavioural change in response to these programs include poor baseline performance, feedback from colleagues, repeated feedback, multimodal communication of feedback, and tangible goals with a clear process to achieve them.
Decision support systems
CDSS are software programs that can assist clinician decision-making. One randomised study published in 1999 utilising a CDSS on hypertension management showed no clinically significant improvement (57), possibly attributed to less than expected use of the CDSS. In contrast, a Cochrane review of 42 trials found that point-of-care computerised advice for drug dosing improved objective parameters for several drugs, including anticoagulants, insulin, and antibiotics, although this did not translate to improvements in mortality (58).
Multifaceted health care systems
Evidence is mixed on whether combining implementation techniques have a synergistic effect on adherence to guidelines. A multifaceted approach to gestational diabetes, using pamphlets, reminders and meetings, showed significantly increased guideline adherence in the prescription of screening tests after 2 years of implementation (25). A study of cervical cancer screening showed significant improvements in most of the clinical recommendations, with use of software modules which facilitated selection, attendance monitoring, follow up and also provided reminders (59). A study conducted of beta-blocker usage in patients with heart failure observed little improvement in prescription after using provider education alone and provider/patient notification, but significant improvements with the use of a nurse facilitator (60). However in diabetes management, implementation methods such as chart audits, performance feedback, reminders and computerized supports improved only 4 of 9 criteria in the first year of use, with effectiveness falling to 2 of the 9 criteria after the second year of implementation (61).
In summary for chronic disease guidelines, numerous methods for improving the implementation of guidelines have been studied, however the results are mixed. Professional education, EHRs and multifaceted implementation programs have shown benefit in some studies, but not in others. Programs that distribute guidelines in a way that promotes active participation by clinicians are more likely to have a positive effect, and interactive reminder systems at the point of care provide an effective solution for guidelines when they are most needed. Further work is needed to identify the aspects of these implementation programs that are beneficial.
Improving adherence to COPD guidelines
There is increasing recognition of the importance of independent research to further clarify the most effective methods for developing and implementing evidence-based guidelines (20). The publication of clinical practice guidelines is only the first step in a process that ends with an actual change in clinician behaviour. The importance of effective guideline dissemination methods cannot be overlooked. Grimshaw et al. (62) reviewed the studies of guideline dissemination methods and the role of guideline developers in this process. They concluded that developers must take an active role in including methods for disseminating and implementing their guidelines.
Most research to date on enhancing uptake of COPD guidelines has focused on improving clinician knowledge and awareness of guidelines through education sessions (Table 2). Studies have shown mixed results, with some suggesting minor improvements in management following the intervention, and others showing no effect.
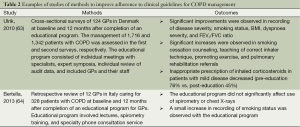
Full table
Two observational studies have evaluated the effect of an education program for GPs on COPD guideline uptake. A study of GPs in Denmark found that several guideline-related indices of diagnosis and management improved 12 months after a comprehensive education program (63). Better use of spirometry to classify disease severity and a reduction in inappropriate use of inhaled corticosteroids were observed. In contrast, a small study of GPs in Italy found no significant change in management following an educational program that consisted of lectures, spirometry training, and specialty phone consultation service (64). The discrepancy between these study results may be due to pre-existing levels of guideline uptake, contrasting styles of educational programs, different health system contexts or inadequate sample size.
Point-of care checklists may also be useful in hospital clinical practice. Previously, members of our group have undertaken a prospective pilot study of the use of an inpatient checklist to promote evidence-based recommendations (unpublished data, presented at the Thoracic Society of Australia and New Zealand Annual Scientific Meeting 2012) (65). Focus groups, statewide stakeholder consultation and a literature review were used to develop a paper-based, one page Inpatient Checklist for acute exacerbations of COPD (AECOPD), based on the Australian COPD-X guidelines. Demographic, process of care and patient outcome data for AECOPD admissions were collected in pre-checklist [2010] and checklist-implementation [2011] phases at one tertiary referral hospital. Two groups of admissions were studied in pre-checklist (n=42) and checklist-implementation (n=68) groups. Adherence to checklist use by ward medical staff in a respiratory ward was 51% (35 of the 68 checklist-implementation admissions).
Concordance with COPD-X Plan recommendations was high overall for patient assessment (e.g., admission chest X-ray 100%) and initial treatment (e.g., inhaled bronchodilators 100%, systemic corticosteroids 79%, and antibiotic therapy 91%). Concordance was lower for inpatient consideration of longer-term issues such as referral to pulmonary rehabilitation (36%). Checklist use was associated with significantly increased rates of arterial blood gas analysis (86% vs. 61%, P=0.02), sputum microbiology testing (83% vs. 58%, P=0.02) and influenza vaccination assessment (71% vs. 51%, P=0.04), compared with admissions without checklist use. Median length of stay did not change significantly with checklist use. In this pilot study, checklist use was associated with increased rates of several recommended strategies for management of inpatients with an AECOPD. This study has shown that there is opportunity to improve aspects of inpatient care for COPD and to refine methods of guideline dissemination (65). There may be even better uptake with electronic checklists for COPD, which could be used in both inpatient and outpatient settings to improve guideline adherence.
Lessons from implementation of COPD, asthma and pneumonia guidelines
While the individual interventions recommended by clinical practice guidelines are evidence-based, there are relatively few studies assessing patient outcomes following the implementation of COPD guidelines per se (66). Most studies of guideline implementation to date have focused on healthcare process rather than patient outcome measures. One small randomised controlled trial assessed change in mean peak expiratory flow rate (PEFR) in patients in general practice patients following a comprehensive guideline implementation program (67). Patients in the intervention group experienced a statistically significant improvement in mean PEFR, as well as respiratory symptoms and pain scores. However this improvement was small when compared to the control group receiving usual care. A large RCT of primary care practices in the US has been planned, which will incorporate systems such as computerised patient activation tools and web-based COPD guidelines to improve guideline uptake (68).
Beyond COPD, there are several examples of guideline implementation leading to improved patient outcomes, in particular in the treatment of pneumonia and asthma. A US study found that implementing pneumonia treatment guidelines significantly reduced 30-day mortality of elderly patients (69). The authors hypothesised that the improved patient outcomes were due to earlier and more accurate identification of high-risk cases, with a significant improvement in utilisation of appropriate antibiotics during the same time period.
In Australia, a multi-faceted approach to improving awareness and management of asthma was implemented with success in the early 1990s, in the form of new clinical guidelines published as an initiative of the National Asthma Council (originally the National Asthma Campaign). These guidelines were published in the Asthma Management Handbook, and now the Australian Asthma Handbook (70). The campaign involved promoting the best practice management for asthma to healthcare professionals, especially in primary care, and the general public (71). This highly effective approach likely played a role in improved asthma management and reduced asthma mortality (by 70% since the 1980s) after implementation (72,73).
Conclusions and future studies
COPD is a major cause of morbidity and mortality worldwide. Guidelines for the diagnosis and treatment of COPD are widely available, however, concordance with these guidelines remains sub-optimal. Numerous barriers to guideline adherence have been identified, but studies assessing methods for improving the uptake of guidelines in COPD management are limited to small-scale non-randomised studies. Given the significant resources invested in guideline development and the cost of management of COPD in general, there is a need for better strategies to ensure effective guideline implementation and optimise their use. Future studies should evaluate implementation strategies used in the management of other diseases for COPD. These studies could assess a combination of techniques to ascertain whether a synergistic response exists and to find the most efficient model with greatest marginal benefit for each different disease. This could allow the development of an optimal protocol that can assist with implementation of guidelines. There are many interventions that have a proven mortality or symptom benefit for patients with COPD. Given the benefits of these treatments, it would be logical to assume that guidelines comprising these interventions would lead to better patient outcomes. There are, however, very few studies assessing the effect of COPD guideline implementation on patient outcomes, and this is an area that requires further research. Clinical guidelines are an important modality for communicating evidence-based recommendations to clinicians at the point of care. The development of guidelines is an important early step, but more research is needed to determine the most effective ways to translate the evidence into everyday clinical practice.
Acknowledgements
We thank the patients and staff involved in our research projects, and the Lung Foundation Australia staff and health professionals in the COPD Evaluation Committee who are involved in the writing of the Australian COPD-X guidelines. We thank John Serginson, Lisa McCarthy and Rina Waller for their assistance with the inpatient COPD checklist study.
Funding: The University of Queensland Research Scholarship (JO), The Prince Charles Hospital Foundation New Investigator Grant (JO), NHMRC Career Development Fellowship 1026215 (IY), NHMRC Practitioner Fellowship 1019891 (KF), AusHSI Stimulus Grant (IY).
Disclaimer: this review article represents the views of the individual contributing authors, and should not necessarily be taken as representing the views of Lung Foundation Australia.
Disclosure: Michael Abramson holds investigator-initiated grants for unrelated research from Pfizer and Boehringer Ingelheim, has received conference support from BI and has undertaken an unrelated consultancy for AstraZeneca. The other authors have no financial conflicts of interest to declare. MA (Chair), IY (Deputy Chair) and JB (Executive Officer) are members of Lung Foundation Australia’s COPD Guidelines Committee which updates the Australian COPD-X clinical guidelines. Lung Foundation Australia receives some funding support from a number of pharmaceutical industry partners towards the COPD National Program. The authors declare no conflict of interest.
References
- Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. 2014. Available online: http://www.goldcopd.org
- World Health Organization. The 10 leading causes of death in the world, 2000 and 2012. 2014. (Accessed May 20, 2014). Available online: http://www.who.int/mediacentre/factsheets/fs310/en/
- Baker R, Camosso-Stefinovic J, Gillies C, et al. Tailored interventions to overcome identified barriers to change: effects on professional practice and health care outcomes. Cochrane Database Syst Rev 2010;CD005470. [PubMed]
- Abramson MJ, Schattner RL, Sulaiman ND, et al. Accuracy of asthma and COPD diagnosis in Australian general practice: a mixed methods study. Prim Care Respir J 2012;21:167-73. [PubMed]
- Anthonisen NR, Connett JE, Murray RP. Smoking and lung function of Lung Health Study participants after 11 years. Am J Respir Crit Care Med 2002;166:675-9. [PubMed]
- Poole PJ, Chacko E, Wood-Baker RW, et al. Influenza vaccine for patients with chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2006;CD002733. [PubMed]
- Walters JA, Smith S, Poole P, et al. Injectable vaccines for preventing pneumococcal infection in patients with chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2010;CD001390. [PubMed]
- Spruit MA, Singh SJ, Garvey C, et al. An official American Thoracic Society/European Respiratory Society statement: key concepts and advances in pulmonary rehabilitation. Am J Respir Crit Care Med 2013;188:e13-64. [PubMed]
- Bolton CE, Bevan-Smith EF, Blakey JD, et al. British Thoracic Society guideline on pulmonary rehabilitation in adults. Thorax 2013;68 Suppl 2:ii1-30. [PubMed]
- Kew KM, Mavergames C, Walters JA. Long-acting beta2-agonists for chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2013;10:CD010177. [PubMed]
- Chung VC, Ma PH, Hui DS, et al. Indacaterol for chronic obstructive pulmonary disease: systematic review and meta-analysis. PLoS One 2013;8:e70784. [PubMed]
- Tashkin DP, Celli B, Senn S, et al. A 4-year trial of tiotropium in chronic obstructive pulmonary disease. N Engl J Med 2008;359:1543-54. [PubMed]
- Karner C, Chong J, Poole P. Tiotropium versus placebo for chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2014;7:CD009285. [PubMed]
- Ni H, Soe Z, Moe S. Aclidinium bromide for stable chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2014;9:CD010509. [PubMed]
- Kerwin E, Hébert J, Gallagher N, et al. Efficacy and safety of NVA237 versus placebo and tiotropium in patients with COPD: the GLOW2 study. Eur Respir J 2012;40:1106-14. [PubMed]
- Celli B, Decramer M, Kesten S, et al. Mortality in the 4-year trial of tiotropium (UPLIFT) in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2009;180:948-55. [PubMed]
- Calverley PM, Anderson JA, Celli B, et al. Salmeterol and fluticasone propionate and survival in chronic obstructive pulmonary disease. N Engl J Med 2007;356:775-89. [PubMed]
- Vollenweider DJ, Jarrett H, Steurer-Stey CA, et al. Antibiotics for exacerbations of chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2012;12:CD010257. [PubMed]
- Walters JA, Tan DJ, White CJ, et al. Systemic corticosteroids for acute exacerbations of chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2014;9:CD001288. [PubMed]
- Schünemann HJ, Woodhead M, Anzueto A, et al. A guide to guidelines for professional societies and other developers of recommendations: introduction to integrating and coordinating efforts in COPD guideline development. An official ATS/ERS workshop report. Proc Am Thorac Soc 2012;9:215-8. [PubMed]
- McKenzie DK, Frith PA, Burdon JG, et al. The COPDX Plan: Australian and New Zealand Guidelines for the management of Chronic Obstructive Pulmonary Disease 2003. Med J Aust 2003;178 Suppl:S7-39. [PubMed]
- Abramson MJ, Crockett AJ, Frith PA, et al. COPDX: an update of guidelines for the management of chronic obstructive pulmonary disease with a review of recent evidence. Med J Aust 2006;184:342-5. [PubMed]
- Fürthauer J, Flamm M, Sönnichsen A. Patient and physician related factors of adherence to evidence based guidelines in diabetes mellitus type 2, cardiovascular disease and prevention: a cross sectional study. BMC Fam Pract 2013;14:47. [PubMed]
- Alanen SI, Johannala-Kemppainen R, Ijäs JJ, et al. Evaluation of current care effectiveness: a survey of hypertension guideline implementation in Finnish health centres. Scand J Prim Health Care 2007;25:232-6. [PubMed]
- Gayet-Ageron A, Poncet B, Guerre P, et al. Specific information about the WHO guidelines for gestational diabetes screening improves clinical practices. J Eval Clin Pract 2008;14:36-42. [PubMed]
- Clark HD, van Walraven C, Code C, et al. Did publication of a clinical practice guideline recommendation to screen for type 2 diabetes in women with gestational diabetes change practice? Diabetes Care 2003;26:265-8. [PubMed]
- Idiculla JM, Perros P, Frier BM. Do diabetes guidelines influence the content of referral letters by general practitioners to a diabetes specialist clinic? Health Bull (Edinb) 2000;58:322-7. [PubMed]
- Jaglal SB, McIsaac WJ, Hawker G, et al. Information needs in the management of osteoporosis in family practice: an illustration of the failure of the current guideline implementation process. Osteoporos Int 2003;14:672-6. [PubMed]
- Troein M, Råstam L, Selander S. Dissemination and implementation of guidelines for lipid lowering. Fam Pract 1991;8:223-8. [PubMed]
- Rutschmann OT, Janssens JP, Vermeulen B, et al. Knowledge of guidelines for the management of COPD: a survey of primary care physicians. Respir Med 2004;98:932-7. [PubMed]
- Li F, Cai Y, Zhu Y, et al. The Evaluation of General Practitioners’ Awareness/Knowledge and Adherence to the GOLD Guidelines in a Shanghai Suburb. Asia Pac J Public Health 2013. [Epub ahead of print]. [PubMed]
- Jochmann A, Neubauer F, Miedinger D, et al. General practitioner’s adherence to the COPD GOLD guidelines: baseline data of the Swiss COPD Cohort Study. Swiss Med Wkly 2010. [Epub ahead of print]. [PubMed]
- Sharif R, Cuevas CR, Wang Y, et al. Guideline adherence in management of stable chronic obstructive pulmonary disease. Respir Med 2013;107:1046-52. [PubMed]
- Belletti D, Liu J, Zacker C, et al. Results of the CAPPS: COPD--assessment of practice in primary care study. Curr Med Res Opin 2013;29:957-66. [PubMed]
- Gold PM. The 2007 GOLD Guidelines: a comprehensive care framework. Respir Care 2009;54:1040-9. [PubMed]
- Sarc I, Jeric T, Ziherl K, et al. Adherence to treatment guidelines and long-term survival in hospitalized patients with chronic obstructive pulmonary disease. J Eval Clin Pract 2011;17:737-43. [PubMed]
- Perez X, Wisnivesky JP, Lurslurchachai L, et al. Barriers to adherence to COPD guidelines among primary care providers. Respir Med 2012;106:374-81. [PubMed]
- Salinas GD, Williamson JC, Kalhan R, et al. Barriers to adherence to chronic obstructive pulmonary disease guidelines by primary care physicians. Int J Chron Obstruct Pulmon Dis 2011;6:171-9. [PubMed]
- Johnston KN, Young M, Grimmer-Somers KA, et al. Why are some evidence-based care recommendations in chronic obstructive pulmonary disease better implemented than others? Perspectives of medical practitioners. Int J Chron Obstruct Pulmon Dis 2011;6:659-67. [PubMed]
- Welke KF. What factors influence provider knowledge of a congestive heart failure guideline in a national health care system? Am J Med Qual 2003;18:122-7. [PubMed]
- Dennis SM, Edwards S, Partridge MR, et al. The dissemination of the British Guideline on the Management of Asthma 2003. Respir Med 2004;98:832-7. [PubMed]
- Onion CW, Bartzokas CA. Changing attitudes to infection management in primary care: a controlled trial of active versus passive guideline implementation strategies. Fam Pract 1998;15:99-104. [PubMed]
- Perria C, Mandolini D, Guerrera C, et al. Implementing a guideline for the treatment of type 2 diabetics: results of a cluster-randomized controlled trial (C-RCT). BMC Health Serv Res 2007;7:79. [PubMed]
- Dey P, Simpson CW, Collins SI, et al. Implementation of RCGP guidelines for acute low back pain: a cluster randomised controlled trial. Br J Gen Pract 2004;54:33-7. [PubMed]
- Forsetlund L, Bjørndal A, Rashidian A, et al. Continuing education meetings and workshops: effects on professional practice and health care outcomes. Cochrane Database Syst Rev 2009;CD003030. [PubMed]
- Cebul RD, Love TE, Jain AK, et al. Electronic health records and quality of diabetes care. N Engl J Med 2011;365:825-33. [PubMed]
- Reed M, Huang J, Graetz I, et al. Outpatient electronic health records and the clinical care and outcomes of patients with diabetes mellitus. Ann Intern Med 2012;157:482-9. [PubMed]
- Reed M, Huang J, Brand R, et al. Implementation of an outpatient electronic health record and emergency department visits, hospitalizations, and office visits among patients with diabetes. JAMA 2013;310:1060-5. [PubMed]
- Sinsky CA, Beasley JW, Simmons GE, et al. Electronic health records: design, implementation, and policy for higher-value primary care. Ann Intern Med 2014;160:727-8. [PubMed]
- Price M. Can hand-held computers improve adherence to guidelines? A (Palm) Pilot study of family doctors in British Columbia. Can Fam Physician 2005;51:1506-7. [PubMed]
- Murtaugh CM, Pezzin LE, McDonald MV, et al. Just-in-time evidence-based e-mail “reminders” in home health care: impact on nurse practices. Health Serv Res 2005;40:849-64. [PubMed]
- Feldman PH, Murtaugh CM, Pezzin LE, et al. Just-in-time evidence-based e-mail “reminders” in home health care: impact on patient outcomes. Health Serv Res 2005;40:865-85. [PubMed]
- Braun V, Heintze C, Rufer V, et al. Innovative strategy for implementing chronic heart failure guidelines among family physicians in different healthcare settings in Berlin. Eur J Heart Fail 2011;13:93-9. [PubMed]
- Arditi C, Rège-Walther M, Wyatt JC, et al. Computer-generated reminders delivered on paper to healthcare professionals; effects on professional practice and health care outcomes. Cochrane Database Syst Rev 2012;12:CD001175. [PubMed]
- McDermott L, Yardley L, Little P, et al. Developing a computer delivered, theory based intervention for guideline implementation in general practice. BMC Fam Pract 2010;11:90. [PubMed]
- Ivers N, Jamtvedt G, Flottorp S, et al. Audit and feedback: effects on professional practice and healthcare outcomes. Cochrane Database Syst Rev 2012;6:CD000259. [PubMed]
- Hetlevik I, Holmen J, Krüger O. Implementing clinical guidelines in the treatment of hypertension in general practice. Evaluation of patient outcome related to implementation of a computer-based clinical decision support system. Scand J Prim Health Care 1999;17:35-40. [PubMed]
- Gillaizeau F, Chan E, Trinquart L, et al. Computerized advice on drug dosage to improve prescribing practice. Cochrane Database Syst Rev 2013;11:CD002894. [PubMed]
- Hermens RP, Hak E, Hulscher ME, et al. Adherence to guidelines on cervical cancer screening in general practice: programme elements of successful implementation. Br J Gen Pract 2001;51:897-903. [PubMed]
- Ansari M, Shlipak MG, Heidenreich PA, et al. Improving guideline adherence: a randomized trial evaluating strategies to increase beta-blocker use in heart failure. Circulation 2003;107:2799-804. [PubMed]
- Kirkman MS, Williams SR, Caffrey HH, et al. Impact of a program to improve adherence to diabetes guidelines by primary care physicians. Diabetes Care 2002;25:1946-51. [PubMed]
- Grimshaw JM, Schünemann HJ, Burgers J, et al. Disseminating and implementing guidelines: article 13 in Integrating and coordinating efforts in COPD guideline development. An official ATS/ERS workshop report. Proc Am Thorac Soc 2012;9:298-303. [PubMed]
- Ulrik CS, Hansen EF, Jensen MS, et al. Management of COPD in general practice in Denmark--participating in an educational program substantially improves adherence to guidelines. Int J Chron Obstruct Pulmon Dis 2010;5:73-9. [PubMed]
- Bertella E, Zadra A, Vitacca M, et al. COPD management in primary care: is an educational plan for GPs useful? Multidiscip Respir Med 2013;8:24. [PubMed]
- Goddard JR, Serginson J, Mccarthy L, et al. An evidence-based checklist for acute exacerbations of chronic obstructive pulmonary disease. Respirology 2012;17:32. [PubMed]
- Heffner JE, Ellis R. The guideline approach to chronic obstructive pulmonary disease: how effective? Respir Care 2003;48:1257-66; discussion 1267-8. [PubMed]
- Jans MP, Schellevis FG, Le Coq EM, et al. Health outcomes of asthma and COPD patients: the evaluation of a project to implement guidelines in general practice. Int J Qual Health Care 2001;13:17-25. [PubMed]
- Parker DR, Eaton CB, Ahern DK, et al. The study design and rationale of the randomized controlled trial: translating COPD guidelines into primary care practice. BMC Fam Pract 2013;14:56. [PubMed]
- Dean NC, Silver MP, Bateman KA, et al. Decreased mortality after implementation of a treatment guideline for community-acquired pneumonia. Am J Med 2001;110:451-7. [PubMed]
- Australian Asthma Handbook, Version 1.0. 2014. Australia’s National Guidelines For Asthma Management. Available online: http://www.asthmahandbook.org.au
- Woolcock A, Rubinfeld AR, Seale JP, et al. Thoracic society of Australia and New Zealand. Asthma management plan, 1989. Med J Aust 1989;151:650-3. [PubMed]
- Comino EJ, Mitchell CA, Bauman A, et al. Asthma management in eastern Australia, 1990 and 1993. Med J Aust 1996;164:403-6. [PubMed]
- Australian Institute of Health and Welfare. Mortality from asthma and COPD in Australia. 2014. Available online: http://www.aihw.gov.au/publication-detail/?id=60129548233


