Antihypertensive therapy with nicardipine for patients with aortic disease is associated with more esmolol usage than urapidil
Introduction
Acute aortic disease is a common and challenging emergency in clinical practice. Of them, aortic aneurysm and aortic dissection are of the most common type. The prognosis of aortic dissection is poor if untreated. Although the outcomes of patients with Stanford type A dissection improved after early repair, both the perioperative and one-year mortality remained high, with a 30-day hospital mortality varying from 9% to 30% and survival rates at five years varying from 50% to 80% (1,2). Titrate the blood pressure and heart rate to a target level is of paramount importance in the acute phase although whether an urgent surgical therapy is necessary varies according to the classification of aortic disease (3). Hence, in addition to the prior β-blockers, intravenous vasodilators are widely used to achieve aggressive blood pressure and heart rate control. Among the vasodilators, most established agents including intravenous sodium nitroprusside, nicardipine, urapidil, nitroglycerin, fenoldopam (4). Currently, parenteral infusion of nicardipine or urapidil are the most common used strategy in mainland China. Nevertheless, few empirical data was available with respect to the different effect on patients’ outcome of various antihypertensive strategies for patients with aortic disease. Especially given the potential deleterious effects of reflex tachycardia of vasodilators which may increase force of ventricular contraction and potentially worsen the diseased aorta (4). Therefore, this study was aimed to evaluate the difference of the abovementioned two antihypertensive strategies on the outcome of patients with aortic disease.
Materials and methods
Study design
This was a retrospective review of all aortic diseases admitted to our hospitals from January 1, 2013 to June 30, 2014, to examine their antihypertensive strategies and their association with patients’ outcomes. The institutional review board of our hospitals approved the study protocol and waived from the need for a consent form given the observational nature of this study.
As practiced in our hospitals, vast majority patients with aortic disease are required to be admitted to ICU for aggressive control of heart rate and blood pressure and close monitoring. Generally, esmolol was infused firstly to control heart rate for patients with tachycardia, then urapidil or nicardipine was administrated continuously for antihypertensive therapy. The target systolic blood pressure and heart rate for aortic disease in our ICU were defined as 100-120 mmHg and 60-70/min respectively. All the parenteral medications were administrated according the pharmacological instruction. The infusion rate was adjusted until the target level was reached within 30-60 min. After the target level had been reached, the rate of infusion was adjusted to maintain this level of heart rate or blood pressure. Given emergency operation indication and the possible clinically instability, all patients received parenteral medications for 3-5 days to manage the heart rate and blood pressure. Thereafter, it was switched to oral anti-hypertensive agents and β-blockers at the discretion of the attending physicians.
All adult patients with new diagnosed aortic diseases during the study period were screened to be included in the study. However, patients with the following characteristics were excluded: (I) did not necessitate the mentioned antihypertensive therapy after admission; (II) with prior signed “Do not resuscitation” directives; (III) refractory hypertension necessitated ≥2 intravenous antihypertensive agents administrated simultaneously; (IV) patients with a contraindication to esmolol such as asthma; (V) antihypertensive therapy with other medications.
Data sources and processing
The hospital admission database and the ICU database were queried to extract all the patients with aortic diseases during the study period. For each patient, the following data were extracted: (I) date and time of hospital and ICU admission; (II) demographic characteristics (age, gender); (III) CT images; (IV) clinical symptom on admission; (V) co-morbidity; (VI) management strategy and whether the patient underwent an urgent surgical intervention, what were the concomitant procedures, and the operation time; (VII) the start and end time for the administration of urapidil, nicardipine, or esmolol; (VIII) the time from the start of antihypertensive therapy to target level; (IX) cost of the above parenteral medications and the total ICU and hospital costs; (X) whether the patient underwent reoperation for postoperative bleeding or pericardial effusion, prolonged intubation >48 hours, renal replacement therapy, or stroke; (XI) ICU and hospital length of stay (LOS); (XII) patient’s ICU outcome.
Primary data analysis
Descriptive data were reported as either mean ± SD, median (interquartile range) or number and percentage. With respect to the differences between urapidil and nicardipine therapy groups, categorical variables were compared using chi-square analysis. Continuous variables were compared using Independent Sample t-test for normally distributed data and Mann-Whitney U test for non-normally distributed data. To evaluate whether various antihypertensive strategies associated with different outcomes for patients with aortic diseases, the median values of the ICU/esmolol cost and ICU LOS were used as cutoffs to transform the data into categorical variables (high/low ICU/esmolol cost, and long/short ICU LOS respectively) for regression analysis.
To clarify potential association between nicardipine antihypertensive therapy and ICU outcomes, binary logistic regression analysis was performed using ICU outcomes [high ICU/esmolol cost (yes/no), long ICU LOS (yes/no), necessitate renal replacement therapy (yes/no), and died in ICU (yes/no), respectively] as the dependent variable and nicardipine antihypertensive therapy (with urapidil as reference), patient demographics, co-morbidity, involved extend of aorta, interventional strategies were used as variables. Odds ratios (ORs) and their 95% confidence intervals (95% CIs) were calculated. Statistical analysis was performed by using SPSS 16.0 (Chicago, Ill, USA). Statistical significance was defined as a P value <0.05.
Results
A total of 120 patients with new diagnosed aortic disease were included in the study. Of them, 47 patients received urapidil while 73 patients received nicardipine antihypertensive therapy. The patients’ characteristics were shown in Table 1. There was no significant difference of age, male percent, classification of aortic disease, severe presentation on admission, and co-morbidity between two groups. However, it seemed that more patients in nicardipine group had aortic dissection of Debakey type I, and therefore a more extensive portion of aorta was involved (P=0.081 and P=0.056, respectively) (Table 2). As expected, patients with nicardipine were more quickly to reach the target blood pressure level (median, 18 vs. 35 min, P=0.024). The median duration of intravenous antihypertensive therapy was similar within the two groups. Moreover, the percent of patients who necessitated esmolol for heart rate control was comparable between the two groups (66/73 vs. 41/47, P=0.585). Surprisingly, patients of nicardipine group received a significant longer duration of esmolol administration and higher total dose of esmolol (P=0.001 and P=0.002, respectively) (Table 2). With respect to the management strategy, concomitant procedures, operation time and cardiopulmonary time, there was no significant difference between the two groups (Table 2).

Full table

Full table
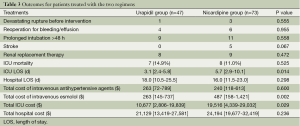
When it comes to the outcomes, there were no difference of percentage of patients with devastating rupture before intervention, reoperation for bleeding/effusion, prolonged intubation >48 h, stroke and renal replacement therapy among the two groups (Table 3). The ICU mortality was 11.0% (8/73) in nicardipine group and 14.9% (7/47) in urpidil group respectively (P=0.525, Table 3). Meanwhile, the total cost for urapidil or nicardipine, hospital LOS and total hospital cost were similar between the two groups (Table 3). Interestingly, the patients in the nicardipine group stayed a median 2.6 days longer in ICU than urapidil treated patients. Moreover, patients with nicardipine antihypertensive therapy spent more median money for intravenous esmolol and ICU stay ($487 vs. $263, P=0.002, and $19,516 vs. $10,677, P=0.029 respectively, Table 3).
Full table
The median esmolol cost, ICU cost and ICU LOS was $374, $15,115, and 4.7 days respectively. Hence, the esmolol/ICU cost and ICU LOS were dichotomized into high (≥ median) and low cost, and long (≥ median) and short ICU LOS respectively. Thereafter, the association between antihypertensive strategy and patients’ outcomes were further assessed by regression analysis with adjustment for age, patient gender, co-morbidity, involved extend of aorta and interventional strategies (Table 4). As a result, antihypertensive therapy with nicardipine in acute phase was significantly associated with high esmolol cost (OR: 6.2, 95% CI, 1.8-21.6, P=0.004) and longer ICU LOS (OR: 3.9, 95% CI, 1.5-10.3, P=0.006) (Table 4). However, there was no significant correlation between nicardipine use and ICU mortality (OR: 0.3, 95% CI, 0.1-1.4, P=0.123).

Full table
Discussion
This study demonstrated that although antihypertensive therapy with nicardipine for patient with aortic disease reached the target blood pressure level more quickly than urapidil, nicardipine was associated with more esmolol use and longer ICU LOS.
Treatment varies greatly according to the location and severity of the aortic disease. Surgery is generally indicated for those involving the ascending aorta, while medical management and subsequently endovascular stent is usually reserved for stable descending aortic disease. Despite contemporary surgical advances, aortic diseases are still a clinical challenge and are associated with high mortality and morbidity. Once the diagnosis of aortic aneurysm or dissection is made, initial management by controlling aortic shear stress while simultaneously determining which patients will benefit from surgical or endovascular repair is essential (4). Given that aortic wall stress is mainly correlated with the velocity of ventricular contraction (dP/dt), blood pressure and heart rate, using β-blockers to reduce heart rate and blood pressure is of top priority. Reasonable initial targets are a heart rate less than 60 bpm and a systolic blood pressure between 100 and 120 mmHg (4). Tight heart rate control was associated with a significantly reduction in aortic events compared to conventional heart rate control group (OR: 0.25, P<0.01) (5). Moreover, patients who started and maintained on β-blockers throughout their hospital course were associated with a significant reduction in postoperative adverse cardiac events (6). This may be because postoperative hemodynamic stability was help to maintain aortic stability and prevent aortic expansion with possible rupture and recurrent dissection.
Given arterial hypertension is the most important predisposing factor for aortic aneurysm or dissection, prompt anti-hypertensive therapy and maintenance of an optimal systolic blood pressure level is of paramount importance. Therefore, if beta-blockade alone does not control hypertension, combination with intravenous antihypertensive agents may be required for more severe hypertension. In acute aortic dissection, goals of anti-hypertensive therapy are the prevention of both the propagation of the dissection and early thrombus formation within the false lumen. The preferred method of antihypertensive therapy is the continuous infusion of parenteral anti-hypertensive drugs (4). An ideal antihypertensive agent should have a rapid onset of action and a predictable dose response, would be easily titratable to the desired blood pressure (7). Although sodium nitroprusside is a potent and short acting vasodilator and had been widely used hypertension emergency, it is photosensitive and requires time-consuming foil wrapping of the administration set to safeguard its potency. Furthermore, it may cause reflex tachycardia which is extraordinary hazardous for patients with aortic dissection (4). As a result, the nicardipine and urapidil had been the most widely used agents for antihypertensive therapy in patients with aortic disease. Urapidil is a competitive and selective short acting blocker of post-synaptic α1-receptor, which inhibits the vasoconstrictive action of catecholamines and consequently decreases blood pressure (8). On the other hand, nicardipine is an effective antihypertensive agent that decreases afterload by reducing total peripheral resistance without reducing cardiac output. Although nicardipine has been widely used in peri- or intra-operative hypertension, recent trials of urapidil in patients with phaeochromocytoma and pre-eclampsia had demonstrated the urapidil is efficient and also well tolerated in control of hypertension (8,9). Nevertheless, few study has compared the effect of this two different antihypertensive agents on the outcomes of patients with aortic disease. In this study, we demonstrated that although patients with nicardipine were more quickly to reach the target blood pressure level (median, 18 vs. 35 min, P=0.024), antihypertensive therapy with nicardipine was significantly associated with high esmolol cost (OR: 6.2, P=0.004). This may be because urapidil had additional central serotonin receptor-mediated antihypertensive activity, this mechanism could explain the lack of reflex tachycardia associated with urapidil use (10). In contrast, nicardipine may be associated with somewhat reflex tachycardia because of its significantly vasodilatation effect. Surprisingly, we also found the nicardipine use was associated with longer ICU LOS (OR: 3.9, P=0.006). This may be because patients in nicardipine group were more severe with more complicated aortic disease and more extensive aorta involved. Thus, some patients may prefer to stay in ICU a bit longer for close monitoring while discharged shortly after transfer from ICU to wards. This was consistent with that the median hospital LOS is comparable in the two groups.
Of note, the postoperative blood pressure level is also associated with the patients’ long-term prognosis. Tsai and colleagues found that patients who died within 3 years of surgery had higher systolic blood pressure compared with those who survived (130 vs. 122 mmHg, P<0.01) (11). In a recent study of 10 years follow-up demonstrated patients who maintained systolic blood pressure <120 mmHg had improved freedom from reoperation compared with those with blood pressure 120-140 or >140 mmHg (92%±5% vs. 74%±7% and 49%±14% respectively, P<0.001) (12). Thus, both the preoperative and postoperative heart rate and blood pressure control for patients with aortic disease play an important role in preventing the continuing damage to the already diseased aorta.
Conclusions
In summary, our finding demonstrated that although nicardipine tends to achieve the target blood pressure level more quickly than urapidil for patients with aortic disease, it was associated with more esmolol use and longer ICU LOS.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Pagni S, Ganzel BL, Trivedi JR, et al. Early and midterm outcomes following surgery for acute type A aortic dissection. J Card Surg 2013;28:543-9. [PubMed]
- Kim KH, Moon IS, Park JS, et al. Nicardipine hydrochloride injectable phase IV open-label clinical trial: study on the anti-hypertensive effect and safety of nicardipine for acute aortic dissection. J Int Med Res 2002;30:337-45. [PubMed]
- Boodhwani M, Andelfinger G, Leipsic J, et al. Canadian Cardiovascular Society position statement on the management of thoracic aortic disease. Can J Cardiol 2014;30:577-89. [PubMed]
- Hiratzka LF, Bakris GL, Beckman JA, et al. 2010 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM guidelines for the diagnosis and management of patients with Thoracic Aortic Disease: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, American Association for Thoracic Surgery, American College of Radiology, American Stroke Association, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Society of Thoracic Surgeons, and Society for Vascular Medicine. Circulation 2010;121:e266-369. [PubMed]
- Kodama K, Nishigami K, Sakamoto T, et al. Tight heart rate control reduces secondary adverse events in patients with type B acute aortic dissection. Circulation 2008;118:S167-70. [PubMed]
- Brooke BS, Dominici F, Makary MA, et al. Use of beta-blockers during aortic aneurysm repair: bridging the gap between evidence and effective practice. Health Aff (Millwood) 2009;28:1199-209. [PubMed]
- Khoynezhad A, Plestis KA. Managing emergency hypertension in aortic dissection and aortic aneurysm surgery. J Card Surg 2006;21:S3-7. [PubMed]
- Wacker JR, Wagner BK, Briese V, et al. Antihypertensive therapy in patients with pre-eclampsia: A prospective randomised multicentre study comparing dihydralazine with urapidil. Eur J Obstet Gynecol Reprod Biol 2006;127:160-5. [PubMed]
- Tauzin-Fin P, Sesay M, Gosse P, et al. Effects of perioperative alpha1 block on haemodynamic control during laparoscopic surgery for phaeochromocytoma. Br J Anaesth 2004;92:512-7. [PubMed]
- Alijotas-Reig J, Bove-Farre I, de Cabo-Frances F, et al. Effectiveness and safety of prehospital urapidil for hypertensive emergencies. Am J Emerg Med 2001;19:130-3. [PubMed]
- Tsai TT, Evangelista A, Nienaber CA, et al. Long-term survival in patients presenting with type A acute aortic dissection: insights from the International Registry of Acute Aortic Dissection (IRAD). Circulation 2006;114:I350-6. [PubMed]
- Melby SJ, Zierer A, Damiano RJ Jr, et al. Importance of blood pressure control after repair of acute type a aortic dissection: 25-year follow-up in 252 patients. J Clin Hypertens (Greenwich) 2013;15:63-8. [PubMed]


