
Conservative treatment for recurrent secondary spontaneous pneumothorax in patients with a long recurrence-free interval
Introduction
Primary spontaneous pneumothorax (PSP) is defined as a pneumothorax that occurs in patients without significant underlying lung disease and an apparent cause (1,2). Secondary spontaneous pneumothorax (SSP) is defined as a pneumothorax that occurs in patients with existing lung disease, such as chronic obstructive lung disease (COPD) or pulmonary tuberculosis (1-4). The goals of treatment for spontaneous pneumothorax (SP) are to fully expand the lung by evacuating air in the pleural space and to prevent recurrence (5-7). Management for SP includes observation, oxygen inhalation, aspiration, closed thoracostomy with or without pleurodesis, and surgery, which are differently applied depending on characteristics of SP, patient condition, and doctors (physicians vs. surgeons) (1,8). According to the American College of Chest Physicians (ACCP) and the British Thoracic Society (BTS) guidelines, the surgical indications for SP include a persistent air leak, contralateral or bilateral pneumothorax, hemopneumothorax, patients at high risk for occupational reasons, and recurrent episodes (9-12). However, there are substantial discrepancies in management and clinical practice when treating SP (3,9-11).
Recurrence is the most important issue for SP with a recurrence rate of up to 30% (1,9,10). Most recurrences occur during the first 6 months to 2 years after the first episode (1,4,13). Although recurrence is included in surgical indications, there is no definitive guideline for managing recurrent SP according to characteristics of recurrence such as the type [primary SP (PSP) or secondary SP (SSP)] and recurrence-free interval (RFI). In other words, it remains unclear whether treatment outcomes differ between early and late recurrence of SP (4,10,11,14). Patients with late recurrence or early cessation of air leak are often managed conservatively without surgical intervention. In addition, surgical interventions for elderly patients with SSP are usually avoided if at all clinically possible because of many medical issues (3,4,11). However, there is currently no definitive evidence to guide the optimal treatment modality (conservative and surgical treatment) according to characteristics of SP and recurrence interval, and the validity of this management is unclear (6). The aims of the present study are to analyze treatment outcomes for recurrent SP according to the type of SP and RFI, and to check the validity of conservative treatment for patients with a long RFI.
Methods
All consecutive patients who met criteria were included from January 2012 to June 2018. The medical records of all patients were retrospectively reviewed. Exclusion criteria for the present study included traumatic or iatrogenic pneumothorax, treatment-related death, catamenial pneumothorax, and any other obvious underlying diseases, such as lung or other primary cancer. Conservative treatment included oxygen inhalation and chest tube or pleurocatheter drainage with or without pleurodesis (14). We performed pleurodesis with autologous blood in patients with a prolonged air leak lasting more than five to seven days, regardless of treatment modality (14,15). Negative suction was usually applied for a persistent air leak lasting more than two days or collapsed lung (14-16). All surgical interventions were performed through video-assisted thoracoscopic surgery with or without pleurodesis. Surgical indications for patients with PSP generally followed the ACCP and BTS guidelines, and also included a prominent bulla on image studies. In addition, surgical intervention for SSP was usually avoided if at all clinically possible, due to its benign disease, our hospital policy, and the higher threshold for receiving surgery in our country, especially in elderly patients with medical comorbidities. However, when a prolonged air leak in SSP lasted more than two weeks and pleurodesis was not effective, surgical intervention was considered. Recurrence was defined as a subsequent episode of an ipsilateral SP, while a contralateral SP was regarded as an independent case (2). Surgical indications for recurrence cases were like those for the first episode. The patients were followed until December 2018.
Statistical consideration and study approval
The Student’s t-test was used to compare the groups with continuous variables. The Chi-squared test or the Fisher’s exact test was used to evaluate the associations between the groups with categorical variables as appropriate. To investigate the outcomes according to treatment modality in each condition, we estimated RFI during the observation period. RFI was measured from the completion of treatment to recurrence or last follow-up. RFI between subgroups was compared using the Kaplan-Meier method with the log-rank test. In addition, we divided patients into two groups [the early (EG) and the late (LG) recurrence group] according to one-year RFI and analyzed treatment outcomes according to one-year RFI. All statistical analyses were performed using the Statistical Package of Social Sciences version 22.0 (Chicago, IL, USA). A P value less than 0.05 (two-sided) was regarded as statistically significant. The present study was approved by the Institutional Review Board of Uijeoungbu St. Mary’s Hospital (IRB Approval number: UC17RESI0112).
Results
Study subjects
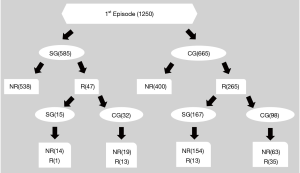
We included 1,250 consecutive cases (624 right sided and 626 left side cases for the first episode) hospitalized and treated conservatively or via surgical interventions January 2012 to June 2018. There were 1,145 male and 105 female cases with a mean age of 36.7 (±21.8) years in the first episode group. There were cases 775 of PSP and 475 cases of SSP. Conservative management and surgical intervention for the first episode of SP were performed in 665 and 585 cases, respectively. Recurrence occurred in 312 out of 1,250 cases. For the second episode of SP, there was 284 male and 28 female cases with a mean age was 38.0 (±23.0) years. Conservative management and surgical intervention for the recurrent cases were performed in 130 and 182 cases, respectively. There was no mortality related to surgical intervention for SP in the first or the second episode. The mean observation period was 25.6 (±28.8) months. The overall clinical characteristics and classifications of the study subjects are summarized in Table 1 and Figure 1.
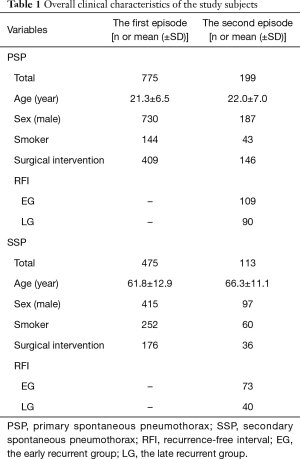
Full table
Recurrence (the second episode) after the first episode according to treatment modality and the type of SP
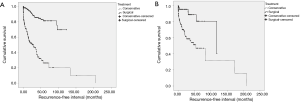
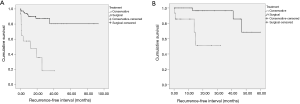
For the first episode of SP, conservative management and surgical intervention were performed in 665 and 585 cases, respectively. The surgical group (SG) had a significantly longer RFI than the conservative group (CG), regardless of the types of SP (both, P<0.001) (Figure 2).
Recurrence (the third episode) after the second episode according to treatment modality, the type of SP, and RFI
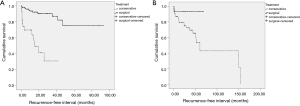
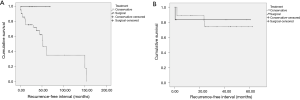
Recurrence occurred in 47 cases after surgical intervention for the first episode (585cases). Recurrence occurred in 265 cases (166 PSP and 99 SSP) after conservative treatment for the first episode of SP (665 cases). For management for these 265 recurrent cases, conservative management and surgical intervention were performed in 98and 167 cases, respectively. We analyzed recurrence after management for the second episode after conservative treatment for the first episode of SP, according to treatment modality and the type of SP. SG had a significantly longer RFI than CG, regardless of the types (PSP P<0.001, SSP P=0.031) (Figure 3). In addition, to check the validity of conservative treatment for patients with a long RFI, we analyzed recurrence by dividing patients into two groups according to one-year RFI. For PSP, the early recurrence group (EG, RFI ≤1 year) had 99 cases and the late recurrent group (LG, RFI >1 year) had 67 cases. SG had a significantly longer RFI than CG in both EG and LG (EG, P<0.001 and LG, P=0.001) (Figure 4). In addition, for SSP, there were 67 cases of EG and 32 cases of LG., SG had significantly longer RFIs than CG in EG (P=0.007). However, there was no significant difference in RFI between SG and CG in LG (P=0.748) (Figure 5).
Discussion
Recurrence is the most important issue for SP, with a recurrence rate up to about 30% (9,10). Most recurrences occur during the first six months to two years after the first episode (13). After the second episode of SP, the risk of a subsequent episode increases up to 60% (10). Despite the ACCP and BTS guidelines for surgical intervention in SP, there are substantial discrepancies in management and in clinical practice for SP (3,9,10,12). Because clinical situations of SP, especially of SSP, are highly various and there have been few studies regarding the management of recurrent SP according to characteristics of recurrence, such as RFI, the optimal treatment approach for recurrent SP according to RFI remains unknown (9). Although the ACCP and the BTS guidelines for surgical intervention for SP include recurrence, we often treat patients with recurrent SP without surgical intervention, especially when PSP with a long RFI and no definitive visible bullae, early cessation of air leak via chest tubes, or SSP in elderly patients with medical comorbidities (3,10). However, we do not know whether conservative management for these situations promotes recurrence (17). In addition, characteristics of recurrence according to RFI remain unclear, so it remains unclear whether managements should differ for the early vs. the late recurrence. Therefore, we investigated the outcomes of management for recurrent SP according to RFI when no surgical intervention for the first episode and examined the validity of conservative treatment for SP according to RFI.
As in many previous studies, surgical intervention for the first episode of SP showed better outcomes regardless of the types of SP (9,13). Surgical intervention for recurrent SP also led to better outcomes in both PSP and SSP. Although the overall RFI after surgical intervention for recurrent SP was longer than that of conservative treatment, management outcomes were different according to the types and the one-year RFI groups. Unlike PSP, surgical intervention for recurrent SSP showed a longer RFI only in the early recurrence cases, but did not show better results in the late recurrence cases compared to conservative treatment. The discrepancies in outcomes according to RFI can be attributed to wide heterogeneous clinical characteristics of SSP (2,13). The important point here is the characteristics of cases that received conservative treatment for recurrent SP. They were cases which had early cessation of air leak via chest tubes, PSP with no visible bullae and a long RFI, or SSP in elderly patients with medical comorbidities (7). Of course, surgical intervention was considered when a highly prolonged air leak and ineffective pleurodesis. Therefore, we attributed these findings to the assumption that conservative treatment for recurrent SSP with long RFIs can be clinically valid in terms of recurrence.
The present study has several limitations, including its retrospective single-center design, lack of ethnic diversity, nonrandomized, heterogeneous data, selection bias, and a small sample size. Because of conservative treatment for SSP per our hospital policy, non-standardized surgical intervention for SSP, the small number of cases, and data heterogeneity, the value of the present study findings might have been limited. Findings from the present study should be verified with large scaled, prospective, randomized studies to validate conservative treatment for recurrent SSP, especially with a long RFI. In addition, the present study showed that recurrence rate of surgical intervention for the first episode of SP was 8.03% which was relatively higher than standard recurrence rate after surgery for SP because a contralateral SP was regarded as an independent case, rate of smoking history was very high (27.7%), surgical indication included prominent bullae on image study, and many SSP cases were included. Of course, other parameters, such as morbidity and mortality, hospital days, duration of chest tube drainage, and economical cost should be considered to validate the treatment modality (9,18,19). However, the present study was performed with regard to SP recurrence. Health service accessibility is also important for the decision making. If patients do not have a good access to medical care, surgical approach may be preferred and the value of the present study findings might have been also limited. However, the health service accessibility in Republic of Korea is at the highest level in the world. Despite these limitations, the present study provides some evidences of the validity of conservative treatment in recurrent SSP with a long RFI. To the best of our knowledge, this is the first study to investigate the validity of conservative treatment in recurrent SSP according to RFI. Although surgical intervention for SP is very safe and effective, we attributed these findings to the assumption that surgical intervention for recurrent SSP can be selectively avoided and conservative treatment for recurrent SSP with long RFIs can be clinically valid with regard to recurrence (1-3,20).
Conclusions
The present study revealed diversity of management outcomes according to characteristics of recurrence and provides some evidences of the validity of conservative treatment for recurrent SSP with a long RFI. Further prospective and randomized large-scale trials are required to validate these findings.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jtd.2020.03.52). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The present study was approved by the Institutional Review Board of Uijeoungbu St. Mary’s Hospital (IRB Approval number: UC17RESI0112).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Li Z, Huang H, Li Q, et al. Pneumothorax: observation. J Thorac Dis 2014;6:S421-6. [PubMed]
- Tschopp JM, Bintcliffe O, Astoul P, et al. ERS task force statement: diagnosis and treatment of primary spontaneous pneumothorax. Eur Respir J 2015;46:321-35. [Crossref] [PubMed]
- Jeon HW, Kim YD, Choi SY, et al. When Is the Optimal Timing of the Surgical Treatment for Secondary Spontaneous Pneumothorax? Thorac Cardiovasc Surg 2017;65:50-5. [Crossref] [PubMed]
- Ueyama M, Asakura T, Morimoto K, et al. Pneumothorax associated with nontuberculous mycobacteria: A retrospective study of 69 patients. Medicine (Baltimore) 2016;95:e4246. [Crossref] [PubMed]
- Sayar A, Kök A, Citak N, et al. Size of pneumothorax can be a new indication for surgical treatment in primary spontaneous pneumothorax: a prospective study. Ann Thorac Cardiovasc Surg 2014;20:192-7. [Crossref] [PubMed]
- Uramoto H, Shimokawa H, Tanaka F. What factors predict recurrence of a spontaneous pneumothorax? J Cardiothorac Surg 2012;7:112. [Crossref] [PubMed]
- Casali C, Stefani A, Ligabue G, et al. Role of blebs and bullae detected by high-resolution computed tomography and recurrent spontaneous pneumothorax. Ann Thorac Surg 2013;95:249-55. [Crossref] [PubMed]
- Ibrahim IM, Elaziz MEA, El-Hag-Aly MA, et al. Early Autologous Blood-Patch Pleurodesis versus Conservative Management for Treatment of Secondary Spontaneous Pneumothorax. Thorac Cardiovasc Surg 2019;67:222-6. [Crossref] [PubMed]
- Treasure T, Hallifax RJ, Rahman N. Are we ready to go directly to videothoracoscopic surgery at a first presentation of primary spontaneous pneumothorax? Eur J Cardiothorac Surg 2016;49:860-1. [Crossref] [PubMed]
- Chen YY, Huang HK, Chang H, et al. Postoperative predictors of ipsilateral and contralateral recurrence in patients with primary spontaneous pneumothorax. J Thorac Dis 2016;8:3217-24. [Crossref] [PubMed]
- Bintcliffe OJ, Hallifax RJ, Edey A, et al. Spontaneous pneumothorax: time to rethink management? Lancet Respir Med 2015;3:578-88. [Crossref] [PubMed]
- MacDuff A, Arnold A, Harvey J. Management of spontaneous pneumothorax: British Thoracic Society Pleural Disease Guideline 2010. Thorax 2010;65:ii18-31. [Crossref] [PubMed]
- Asano H, Ohtsuka T, Noda Y, et al. Risk factors for recurrence of primary spontaneous pneumothoraxafter thoracoscopic surgery. J Thorac Dis 2019;11:1940-4. [Crossref] [PubMed]
- Brown SG, Ball EL, Perrin K, et al. Study protocol for a randomised controlled trial of invasive versus conservative management of primary spontaneous pneumothorax. BMJ Open 2016;6:e011826. [Crossref] [PubMed]
- Pompili C, Salati M, Brunelli A. Chest Tube Management after Surgery for Pneumothorax. Thorac Surg Clin 2017;27:25-8. [Crossref] [PubMed]
- Rocco G, Brunelli A, Rocco R. Suction or Nonsuction: How to Manage a Chest Tube After Pulmonary Resection. Thorac Surg Clin 2017;27:35-40. [Crossref] [PubMed]
- Primavesi F, Jäger T, Meissnitzer T, et al. First Episode of Spontaneous Pneumothorax: CT-based Scoring to Select Patients for Early Surgery. World J Surg 2016;40:1112-20. [Crossref] [PubMed]
- Chambers A, Scarci M. In patients with first-episode primary spontaneous pneumothorax is video-assisted thoracoscopic surgery superior to tube thoracostomy alone in terms of time to resolution of pneumothorax and incidence of recurrence? Interact Cardiovasc Thorac Surg 2009;9:1003-8. [Crossref] [PubMed]
- Goto T. Is surgery the choice for treatment for first presentation of pneumothorax? J Thorac Dis 2019;11:S1398-401. [Crossref] [PubMed]
- Yang Y, Dong J, Huang Y. Single-incision versus conventional three-port video-assisted surgery in the treatment of pneumothorax: a systematic review and meta-analysis. Interact Cardiovasc Thorac Surg 2016;23:722-8. [Crossref] [PubMed]


