Semi-Fowler vs. lateral decubitus position for thoracoscopic sympathectomy in treatment of primary focal hyperhidrosis
Introduction
Primary or essential hyperhidrosis is a disorder with an unknown cause and is characterized by excessive sweating beyond physiological needs, particularly in response to temperature and emotional stimuli (1). It affects men and women equally, with a peak incidence in the later second and early third decades of life, with incidence in the Western world of up to 2.8% of the population (2).
The underlying pathology of sweating disorders is yet not well understood. Recent research has concluded that the feature common to various types of hyperhidrosis is extreme non-thermoregulatory sympathetic stimulus of sweat glands. It has been shown that excessive sweating does not occur during sleeping times, which suggests that emotional stimuli play an important role (3).
Thoracoscopic sympathectomy is well known minimal invasive surgical procedure, which has evolved into an effective treatment for severe primary hyperhidrosis, due to its high immediate and permanent success rate and low morbidity (4,5). It can be done as an outpatient procedure or one day surgery safely and efficiently (6).
Thoracoscopic sympathectomy can be performed through lateral decubitus position using double lumen endotracheal intubation, or through Semi-Fowler supine position (semi sitting with arm abducted) using single lumen endotracheal intubation with or without insufflation of CO2.
Objective
The aim of this study is to compare usefulness of Semi-Fowler position vs. lateral decubitus position for thoracoscopic sympathectomy in treatment of primary focal hyperhidrosis.
Materials and methods
From January 2009 to January 2010, 263 consecutive patients with palmar and axillar hyperhidrosis underwent thoracoscopic sympathectomy Th2-Th4. Patients were divided into two groups: group A (n=133) underwent thoracoscopic sympathectomy through lateral decubitus using double lumen endotracheal intubation, and group B (n=130) underwent thoracoscopic sympathectomy through Semi-Fowler supine position (semi sitting with arm abducted) using single lumen endotracheal intubation without insufflation of CO2, but with short apnea period. All operations were performed with two 5 mm-operating ports (Aesculap): a videothoracoscopic camera (Telescope Aesculap 5 mm 0°) connected with the video data processing post (Richard Wolf 3CCD Camera System) and an endoscopic ultrasound surgical knife (Auto Sonix-Hook Probe; Auto Sonix-Ultrasonioc Surgical System Tyco).
The selection criteria were: no previous thoracic surgery procedures, serious cardiocirculatory or pulmonary insufficiency, pleural empyema, bradycardia. All the patients reported the history of excessive sweating persisting for several years unresponsive to the conservative treatment regimen (adapted diet, antiperspirants, medicaments, botox, iontophoresis). The study also excluded the patients suffering from secondary hyperhidrosis due to other diseases (diabetes mellitus, hyperthyroidism, carcinoid tumor, lymphoma).
Severity of sweating were graded using Hyperhidrosis Disease Severity Scale-HDSS (International Hyperhidrosis Society, www.sweathelp.org), between 1 (no symptoms) and 4 (worst symptoms). Patients were asked to rate their symptoms before and after the surgery: scores 3 and 4 indicated severe hyperhidrosis, while 1 and 2 indicates mild or moderate hyperhidrosis. After the surgery, patients rated their symptoms again: 1-point improvement was associated with a 50% reduction in sweat production, and 2-point improvement with 80% reduction in sweat production.
The intraoperative monitoring included the arterial blood pressure, electrocardiography, and pulse oximetry.
Surgical technique
In the group A, patient was positioned in the lateral decubitus, with a roll pillow at the level of the scapula peak to additionally extend the intercostal space. After intubation with double lumen endotracheal tube, having the lung on the operative side collapsed, the following instruments were introduced into the pleural space through two 5 mm-operating ports. Skin incisions were made through the third intercostal space in the middle axillary line, and through the fifth intercostal space in the posterior axillary line. The patient was then rotated to allow gravity to retract the lung away from the surface of the spine.
Having identified the first rib and the sympathetic chain, it was transected over the second, third and fourth rib heads. After that, the parietal pleura was resected over the body of the second and third rib, starting from the costovertebral angle onto the lateral direction, in the length of 4-5 cm, cutting off the accessory sympathetic nerves (Kuntz fibres). The surgery was ended by introducing a single chest tube No 16F connected to the active suction of −20 cm H2O. The chest tube was fixed by Sofsik 0 (Tyco) and the skin suture performed by Vicryl 3.0 (Ethicon). The patient was then repositioned, and the same surgical procedure was performed on the opposite side. Having obtained the radiological verification of the pulmonary parenchyma re-expansion, the chest tubes were removed on the 0th and 1st postoperative day.
In the group B, patient was positioned in the Semi-Fowler supine position-semi sitting with arms outstretched to allow access to the axillary region for the ports, using single lumen endotracheal intubation without insufflation of CO2, but with short apnea period. Skin incisions were made through the third intercostal space in the anterior axillary line, and through the fifth intercostal space in the middle axillary line. The same surgical procedure was performed like in group A. The chest tube was kept in the first side until the contralateral sympathectomy was completed. Identical technique was then performed on the contralateral side. After re-inflation of both lungs, chest tubes were removed in operating room and chest radiograph was obtained to look for residual pneumothoraces. Patients were discharged from the hospital a few hours after the surgery.
Statistical analysis
Data were presented as mean ± standard deviation for continuous variables, and as frequencies while categoric data were presented percentages. Means were compared by two-sided t-test for dependent samples. Two-sided t-test was used for comparison of percentages too. Statistical analysis was performed using JMP statistical software (JMP 7, SAS Institute, Cary, NC).
Results
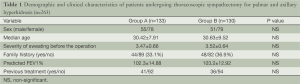
There were 107 males and 156 females with median age 30.31±8.35 years. Two groups were comparable in gender, age, the severity of sweating, family history, predicted FEV 1% and previous treatment (Table 1).
Full table
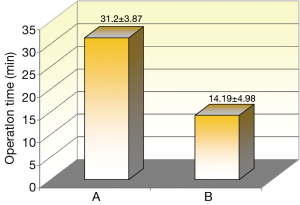
All operations were successfully performed with no major complications. For group A average operation time for both sides was 31.2±3.87 min and for group B average time was 14.19±4.98 min. (Figure 1).
In group B apnea period per one lung lasts 2.86±1.15 min and during that period observed saturation was 92.65%±5.66% without significant cardiorespiratory disturbances.
In group A five patients have pleural adhesions and eight patients in group B, adhesiolysis was performed successfully in both groups and followed by sympathectomy.
There were four patients (3.01%) in group A with incomplete lung re-expansion who needed re-drainage for a one day and two patients (1.54%) in group B needed re-drainage for one day.
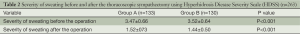
In both groups of patients there have been significant improvement in the mean HDSS score after the thoracoscopic sympathectomy: in group A from 3.47±0.66 to 1.52±073 and in group B from 3.52±0.64 to 1.44±0.50 (Table 2).
Full table
Discussion
Since the introduction of video-assisted thoracic surgery in the early 1990s and as the result of improved telescopes and video imaging technology, thoracoscopic sympathectomy has become a standard therapy for hyperhidrosis worldwide. The short hospital stay, with over 90% patients spending less than 24 hours in the hospital, is in part due to a generally young and fit population (6).
In this study, there were more female patients in both groups, than male patients, which can be explained that female patients are more considered for their outlook. Average age on presentation for the operation was 30 years in both groups. More female patients and average age in both groups is in accordance with some others studies (2,7,8).
Family history was positive in group A in 33.1% and in group B in 36.9%. These results are in agreement with other studies, where it ranges from 30% to 65% (9,10).
Technically, thoracoscopic sympathectomy can be performed through lateral decubitus position using double lumen endotracheal intubation, or through Semi-Fowler supine position (semi sitting with arm abducted) using single lumen endotracheal intubation with or without insufflation of CO2. Both procedures are highly effective with very good visualization.
Common side effects include paresthesias (1%), pneumothorax (1%), bleeding and infection (1%) and incisional pain (2%) (11,12).
The Semi-Fowler supine position negates gravity that is one of the main natural protective mechanisms from shunt fraction increase which is significant when lateral decubitus position is assumed. Moreover, it adds to the reduction of the functional residual capacity due to the displacement of the diaphragm in the supine position (13).
The average operation time for both sides was 31.2±3.87 min for group A and for group B average operation time was 14.19±4.98 min. There was a significant difference in operation time between these two groups. In group A operation lasts longer, due to the preparation of each side, changing the patient position from right lateral decubitus to left lateral decubitus position.
Pleural adhesions are not infrequent, and are usually, but not always, right sided. The incidence of pleural adhesions in the literature is from 1.3% to 6.4% (14,15). Older patients, especially those more than 40 years of age, have a higher rate of pleural adhesions. The most common cause of the pleural adhesions may be pulmonary infections, tuberculosis, chronic bronchitis. Sometimes, the creation of another incision is necessary for safer adhesiolysis. In this study, adhesiolysis was performed successfully in both groups (five patients in group A, and eight patients in group B) and followed by sympathecotomy. It was easier to perform the adhesiolysis in group B (Semi-Fowler position) due to the fact that gravity pulled down the apex of the lung.
On the right side, much more often than on the left side, sympathetic chain may be adjacent to, or even covered by bridging veins, which can complicate the sympathectomy. In these cases, the parietal pleura over the vein can be incised with cautery or by endoscopic scissors, and the sympathetic chain carefully dissected out, away from the vessel.
In group B apnea period per one lung lasts 2.86±1.15 min and during that period observed saturation was 92.65%±5.66% without significant cardiorespiratory disturbances.
The usage of intrapleural CO2 can be associated with some complications, such as tension pneumothorax, hemodynamic decompensation, cerebral oedema or even death (12). These complications are more often if the CO2 insufflation pressure is above 10 mmHg. In this study, it has been shown that thoracoscopic sympathectomy can be performed safely and efficient without using CO2 insufflation.
The significant improvement in the mean HDSS score after the thoracoscopic sympathectomy in both groups (in group A from 3.47±0.66 to 1.52±073 and in group B from 3.52±0.64 to 1.44±0.50) suggests that thoracoscopic sympathectomy can be performed effectively using lateral decubitus position or using Semi-Fowler position. These results are in agreement with other studies (6,16-19).
Morbidity was mostly related to postoperative pneumothoraces (20). Reported rates of pneumothoraces requiring chest drain vary from 0 to 8%, compared to 5.6% in the series of Wilson and co (21).
There are two types of pneumothoraces that occur after the thoracoscopic sympathectomies. The first one is the residual pneumothorax that can develop due to the failure of complete exsufflation of air or gas from the thoracic cavity after the operation. If the pneumothorax is small (2 cm or less) on the postoperative chest radiograph, and the patient is asymptomatic, there is no need for re-drainage or needle exsufflation, because it would be reabsorbed in a few days, with no sequelae (22,23).
The second type of pneumothorax occured after a lung injury from a trocar or diathermy hook, and it should be treated with chest tube drainage. Sometimes, this type of pneumothorax requires surgery for pleurodesis if a persistent air leak exists (24-40).
There were four patients (3.01%) in group A with incomplete lung re-expansion who needed re-drainage for a one day and two patients (1.54%) in group B needed re-drainage for one day. One patient from group A and one patient from group B had incomplete lung re-expansion after adhesiolysis, so re-drainage was performed and after the air leak stop, drains were taken out and patients were discharged from the hospital. Due to patient position (semi sitting), lung re-expansion was better in group B than in group A (lateral decubitus position) (41-64).
Conclusions
Based on this data (shorter operating time, lack of incomplete lung collapse, insignificant apnea and better re-expansion of lungs) we concluded that thoracoscopic sympathectomy through Semi-Fowler supine position is highly effective and easy to perform for primary hyperhidrosis (65-69).
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Bouma W, Klinkenberg TJ, Mariani MA. Bilateral single port thoracoscopic sympathectomy with the VasoView device in the treatment of palmar and axillary hyperhidrosis. Interact Cardiovasc Thorac Surg 2011;12:106-9. [PubMed]
- Strutton DR, Kowalski JW, Glaser DA, et al. US prevalence of hyperhidrosis and impact on individuals with axillary hyperhidrosis: results from national survey. J Am Acad Dermatol 2004;51:241-8. [PubMed]
- Vorkamp T, Foo FJ, Khan S, et al. Hyperhidrosis: evolving concepts and a comprehensive review. The Surgeon 2010;8:287-92. [PubMed]
- Neumayer C, Zacherl J, Holak R, et al. Limited endoscopic thoracic sympathetic block for hyperhidrosis of the upper limb. Surg Endosc 2004;18:152-6. [PubMed]
- Doolabh N, Horswell S, Williams M, et al. Thoracoscopic sympathectomy for hyperhidrosis: indications and results. Ann Thorac Surg 2004;77:410-4. [PubMed]
- Krasna MJ. Thoracoscopic sympathectomy: a standardized approach to therapy for hyperhidrosis. Ann Thorac Surg 2008;85:S764-7. [PubMed]
- Karimian-Teherani D, Panhofer P, Ringhofer C, et al. New epidemiological aspects of patients with severe hyperhidrosis presenting for sympathtic surgery. J Eur Acad Dermatol Venereol 2009;23:651-5. [PubMed]
- Lear W, Kessler E, Solish N. An epidemiological study of hiperhidrosis. Dermatol Surg 2007;33:S69-75. [PubMed]
- Hamm H, Naumann MK, Kowalsky JW, et al. Primary focal hyperhidrosis: disease characteristics and functional impairment. Dermatology 2006;212:343-53. [PubMed]
- Ro KM, Cantor RM, Lange KL, et al. Palmar hyperhidrosis: evidence of genetic transmision. J Vasc Surg 2002;35:382-6. [PubMed]
- Kwong KF, Hobbs JL, Cooper LB, et al. Stratified analysis of clinical outcomes in thoracoscopic sympathectomy for hyperhidrosis. Ann Thorac Surg 2008;85:390-3; discussion 393-4.
- Cameron AE. Complications of endoscopic sympathectomy. Eur J Surg Suppl 1998;580:33-5. [PubMed]
- Elia S, Guggino G, Mineo D, et al. Awake one stage bilateral thoracoscopic sympathectomy for palmar hyperhidrosis: a safe outpatient procedure. Eur J Cardiothorac Surg 2005;28:312-7. [PubMed]
- Chang YT, Li HP, Lee JY, et al. Treatment of palmar hyperhidrosis. T(4) level compared with T(3) and T(2). Ann Surg 2007;246:330-6. [PubMed]
- Wait SD, Killory BD, Lekovic BD, et al. Thoracoscopic sympathectomy for hyperhidrosis: Analysis of 642 procedures with special attention to Horners syndrom and compensatory hyperhidrosis. Neurosurgery 2010;19:526-31.
- Wolosker N, Yazbek G, de Campos JR, et al. Quality of life before surgery is predictive factor for satisfaction among patients undergoing sympathectomy to treat hyperhidrosis. J Vasc Surg 2010;51:1190-4. [PubMed]
- Murphy MO, Ghosh J, Khwaja N, et al. Upper dorsal endoscopic thoracic sympathectomy: a comparision of one- and two-port ablation techniques. Eur J Cardiothorac Surg 2006;30:223-7. [PubMed]
- Schmidt J, Bechara FG, Altmeyer P, et al. Endoscopic thoracic sympathectomy for severe hyperhidrosis: impact of restrictive denervation on compensatory sweating. Ann Thorac Surg 2006;81:1048-55. [PubMed]
- Bachmann K, Standl N, Kaifi J, et al. Thoracoscopic sympathectomy for palmar and axillar hyperhidrosis: four year outcome and quality of life after bilateral 5-mm dual port approach. Surg Endosc 2009;23:1587-93. [PubMed]
- Assalia A, Bahouth H, Ilivitzki A, et al. Thoracoscopic sympathectomy for primary palmar hyperhidrosis: resection versus transection-a prospective trial. World J Surg 2007;31:1976-9. [PubMed]
- Wilson MJ, Magee TR, Galland RB, et al. Results of thoracoscopic sympathectomy for treatment of axillary and palmar hyperhidrosis with respect to compensatory hyperhidrosis and dry hands. Surg Endosc 2005;19:254-6. [PubMed]
- Rodrígez PM, Freixinet JL, Husein M, et al. Side effects, complications and outcome of thoracoscopic sympathectomy for palmar and axillar hyperhidrosis in 406 patients. Eur J Cardiothorac Surg 2008;34:514-9. [PubMed]
- Dewey TM, Herbert MA, Hill SL, et al. One-year follow–up after thoracoscopic sympathectomy for hyperhidrosis: outcomes and consequences. Ann Thorac Surg 2006;81:1227-32. [PubMed]
- Jeganathan R, Jordan S, Jones M, et al. Bilateral thoracoscopic sympathectomy: results and long term follow up. Interact Cardiovasc Thorac Surg 2008;7:67-70. [PubMed]
- Kioumis IP, Zarogoulidis K, Huang H, et al. Pneumothorax in cystic fibrosis. J Thorac Dis 2014;6:S480-7. [PubMed]
- Kuhajda I, Zarogoulidis K, Kougioumtzi I, et al. Tube thoracostomy; chest tube implantation and follow up. J Thorac Dis 2014;6:S470-9. [PubMed]
- Manika K, Kioumis I, Zarogoulidis K, et al. Pneumothorax in sarcoidosis. J Thorac Dis 2014;6:S466-9. [PubMed]
- Kaur K, Singhal SK, Bhardwaj M, et al. Penetrating abdomino-thoracic injury with an iron rod: An anaesthetic challenge. Indian J Anaesth 2014;58:742-5. [PubMed]
- Kuhajda I, Zarogoulidis K, Kougioumtzi I, et al. Penetrating trauma. J Thorac Dis 2014;6:S461-5. [PubMed]
- Visouli AN, Zarogoulidis K, Kougioumtzi I, et al. Catamenial pneumothorax. J Thorac Dis 2014;6:S448-60. [PubMed]
- Huang Y, Huang H, Li Q, et al. Transbronchial lung biopsy and pneumothorax. J Thorac Dis 2014;6:S443-7. [PubMed]
- Terzi E, Zarogoulidis K, Kougioumtzi I, et al. Acute respiratory distress syndrome and pneumothorax. J Thorac Dis 2014;6:S435-42. [PubMed]
- Boskovic T, Stojanovic M, Stanic J, et al. Pneumothorax after transbronchial needle biopsy. J Thorac Dis 2014;6:S427-34. [PubMed]
- Li Z, Huang H, Li Q, et al. Pneumothorax: observation. J Thorac Dis 2014;6:S421-6. [PubMed]
- Huang Y, Huang H, Li Q, et al. Approach of the treatment for pneumothorax. J Thorac Dis 2014;6:S416-20. [PubMed]
- Browning RF, Parrish S, Sarkar S, et al. Bronchoscopic interventions for severe COPD. J Thorac Dis 2014;6:S407-15. [PubMed]
- Machairiotis N, Kougioumtzi I, Dryllis G, et al. Laparoscopy induced pneumothorax. J Thorac Dis 2014;6:S404-6. [PubMed]
- Ouellette DR, Parrish S, Browning RF, et al. Unusual causes of pneumothorax. J Thorac Dis 2014;6:S392-403. [PubMed]
- Parrish S, Browning RF, Turner JF Jr, et al. The role for medical thoracoscopy in pneumothorax. J Thorac Dis 2014;6:S383-91. [PubMed]
- Terzi E, Zarogoulidis K, Kougioumtzi I, et al. Human immunodeficiency virus infection and pneumothorax. J Thorac Dis. 2014;6:S377-82. [PubMed]
- Zarogoulidis P, Kioumis I, Pitsiou G, et al. Pneumothorax: from definition to diagnosis and treatment. J Thorac Dis 2014;6:S372-6. [PubMed]
- Tsakiridis K, Mpakas A, Kesisis G, et al. Lung inflammatory response syndrome after cardiac-operations and treatment of lornoxicam. J Thorac Dis 2014;6:S78-98. [PubMed]
- Tsakiridis K, Zarogoulidis P, Vretzkakis G, et al. Effect of lornoxicam in lung inflammatory response syndrome after operations for cardiac surgery with cardiopulmonary bypass. J Thorac Dis 2014;6:S7-S20. [PubMed]
- Argiriou M, Kolokotron SM, Sakellaridis T, et al. J Thorac Dis 2014;6:S52-9. [PubMed]
- Madesis A, Tsakiridis K, Zarogoulidis P, et al. Review of mitral valve insufficiency: repair or replacement. J Thorac Dis 2014;6:S39-51. [PubMed]
- Siminelakis S, Kakourou A, Batistatou A, et al. Thirteen years follow-up of heart myxoma operated patients: what is the appropriate surgical technique? J Thorac Dis 2014;6:S32-8. [PubMed]
- Foroulis CN, Kleontas A, Karatzopoulos A, et al. Early reoperation performed for the management of complications in patients undergoing general thoracic surgical procedures. J Thorac Dis 2014;6:S21-31. [PubMed]
- Nikolaos P, Vasilios L, Efstratios K, et al. Therapeutic modalities for Pancoast tumors. J Thorac Dis 2014;6:S180-93. [PubMed]
- Koutentakis M, Siminelakis S, Korantzopoulos P, et al. Surgical management of cardiac implantable electronic device infections. J Thorac Dis 2014;6:S173-9. [PubMed]
- Spyratos D, Zarogoulidis P, Porpodis K, et al. Preoperative evaluation for lung cancer resection. J Thorac Dis 2014;6:S162-6. [PubMed]
- Porpodis K, Zarogoulidis P, Spyratos D, et al. Pneumothorax and asthma. J Thorac Dis 2014;6:S152-61. [PubMed]
- Panagopoulos N, Leivaditis V, Koletsis E, et al. Pancoast tumors: characteristics and preoperative assessment. J Thorac Dis 2014;6:S108-15. [PubMed]
- Visouli AN, Darwiche K, Mpakas A, et al. Catamenial pneumothorax: a rare entity? Report of 5 cases and review of the literature. J Thorac Dis 2012;4:17-31. [PubMed]
- Zarogoulidis P, Chatzaki E, Hohenforst-Schmidt W, et al. Management of malignant pleural effusion by suicide gene therapy in advanced stage lung cancer: a case series and literature review. Cancer Gene Ther 2012;19:593-600. [PubMed]
- Papaioannou M, Pitsiou G, Manika K, et al. COPD Assessment Test: A Simple Tool to Evaluate Disease Severity and Response to Treatment. COPD 2014; [PubMed]
- Boskovic T, Stanic J, Pena-Karan S, et al. Pneumothorax after transthoracic needle biopsy of lung lesions under CT guidance. J Thorac Dis 2014;6:S99-S107. [PubMed]
- Papaiwannou A, Zarogoulidis P, Porpodis K, et al. Asthma-chronic obstructive pulmonary disease overlap syndrome (ACOS): current literature review. J Thorac Dis 2014;6:S146-51. [PubMed]
- Zarogoulidis P, Porpodis K, Kioumis I, et al. Experimentation with inhaled bronchodilators and corticosteroids. Int J Pharm 2014;461:411-8. [PubMed]
- Bai C, Huang H, Yao X, et al. Application of flexible bronchoscopy in inhalation lung injury. Diagn Pathol 2013;8:174. [PubMed]
- Zarogoulidis P, Kioumis I, Porpodis K, et al. Clinical experimentation with aerosol antibiotics: current and future methods of administration. Drug Des Devel Ther 2013;7:1115-34. [PubMed]
- Zarogoulidis P, Pataka A, Terzi E, et al. Intensive care unit and lung cancer: when should we intubate? J Thorac Dis 2013;5:S407-12. [PubMed]
- Hohenforst-Schmidt W, Petermann A, Visouli A, et al. Successful application of extracorporeal membrane oxygenation due to pulmonary hemorrhage secondary to granulomatosis with polyangiitis. Drug Des Devel Ther 2013;7:627-33. [PubMed]
- Zarogoulidis P, Kontakiotis T, Tsakiridis K, et al. Difficult airway and difficult intubation in postintubation tracheal stenosis: a case report and literature review. Ther Clin Risk Manag 2012;8:279-86. [PubMed]
- Zarogoulidis P, Tsakiridis K, Kioumis I, et al. Cardiothoracic diseases: basic treatment 2014;6:S1.
- Kolettas A, Grosomanidis V, Kolettas V, et al. Influence of apnoeic oxygenation in respiratory and circulatory system under general anaesthesia. J Thorac Dis 2014;6:S116-45. [PubMed]
- Turner JF, Quan W, Zarogoulidis P, et al. A case of pulmonary infiltrates in a patient with colon carcinoma. Case Rep Oncol 2014;7:39-42. [PubMed]
- Machairiotis N, Stylianaki A, Dryllis G, et al. Extrapelvic endometriosis: a rare entity or an under diagnosed condition? Diagn Pathol 2013;8:194. [PubMed]
- Tsakiridis K, Zarogoulidis P. An interview between a pulmonologist and a thoracic surgeon-Pleuroscopy: the reappearance of an old definition. J Thorac Dis 2013;5:S449-51. [PubMed]
- Huang H, Li C, Zarogoulidis P, et al. Endometriosis of the lung: report of a case and literature review. Eur J Med Res 2013;18:13. [PubMed]


