
Initial experience with uniportal video-assisted thoracoscopic surgery for the treatment of lung cancer performed by a surgeon who did not have previous experience performing multiportal thoracoscopic surgery: a single center retrospective study
Introduction
Video-assisted thoracoscopic surgery (VATS) is an established surgical procedure for the treatment of early-stage lung cancer (1,2). More than 20 years ago, when open thoracotomy was the standard procedure, VATS had limited application due to immaturity of the instruments and techniques in Korea. Over time, however, surgeons gained familiarity with VATS, developed more convenient instruments, and improved their surgical techniques; currently, at our hospital, approximately 80% of early stage lung cancer operations are VATS procedures (3,4). VATS results in less postoperative pain and faster recovery than open thoracotomy (5). Also, VATS improves the survival of patients with early lung cancer (6,7).
Initially, multiportal (three- or four-port) VATS was the usual approach for lobectomy or segmentectomy. However, the development of new instruments and surgical techniques reduced the number of ports, enabling two-port VATS and eventually uniportal VATS, which is considered a form of evolution of multi-portal VATS (8). Some studies reported that uniportal VATS has advantages of less postoperative pain, faster recovery, decreased length of hospital stay, and potential earlier administration of adjuvant therapy than multiportal VATS (9,10). The advantages result from the use of only one intercostal space and the usual placement of the incision more anteriorly than in multiportal VATS.
Previously, most surgeons who performed multiportal VATS had experience with open thoracotomy. However, more recently, as VATS rapidly became the dominant lung cancer operation, many young surgeons had no opportunity to independently perform open thoracotomy (2). Residents and junior surgeons who received training in VATS lobectomy for 80% to 90% of all lung cancer procedures naturally became VATS-friendly surgeons. As a result, VATS may be the first procedure that young surgeons perform independently. Uniportal VATS may also be performed by surgeons who have fully integrated multiportal VATS. However, since the development of uniportal VATS lobectomy, a standardized surgical procedure has been proposed and recently, a uniportal VATS training program has been established, exposing many young surgeons to uniportal VATS. Therefore, many surgeons may perform uniportal VATS immediately after training, without previous experience with multiportal VATS.
The purpose of this study was to evaluate the surgical outcomes of uniportal VATS for the treatment of lung cancer performed by a surgeon without previous experience in open thoracotomy and multiportal VATS. We sought to determine if a new surgeon can perform uniportal VATS without first developing expertise in open thoracotomy or multiportal VATS. We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/jtd-20-242).
Methods
Patients
From January 2017 to December 2018, 657 patients were diagnosed with non-small cell lung cancer (NSCLC) and underwent curative surgery at a tertiary hospital in Korea. Of those patients, 581 underwent anatomical pulmonary resection (segmentectomy, lobectomy, bilobectomy, and pneumonectomy). Among the 581 patients, 85 underwent uniportal VATS performed by one surgeon. Multiportal VATS was performed in the remaining 269 patients by 3 senior surgeons, using 3 or 4 ports. To reduce the selection bias, all data were obtained from consecutive patient data. The three senior surgeons had never performed uniportal VATS. However, each had more than 10 years of surgical experience with multiportal VATS. Clinicopathological characteristics and surgical outcomes in all cases of uniportal or multiportal VATS were analyzed and compared.
Surgical experience of the uniportal VATS surgeon
The junior surgeon began performing uniportal VATS in 2017. Previously, he was a clinical fellow at a tertiary hospital from 2013 to 2016. During his fellowship, he served as 1st assistant for lung cancer surgery; his experience consisted of more than 400 lung cancer cases with open thoracotomy or multiportal VATS. He did not perform any independent lung cancer surgery during that time and had no experience with uniportal VATS. In January 2017, he attended a uniportal VATS training program at Tongji University Shanghai Pulmonary Hospital in Shanghai, China (11). The hospital is an ultra-high-volume center in thoracic surgery where more than 10,000 lung cancer resections are performed annually. There, the surgeon learned the techniques of uniportal VATS lobectomy and segmentectomy by observing the operations of Dr. Diego Gonzalez-Rivas and also learned Dr. Diego’s surgical techniques from articles and videos (10,12-14)). Subsequently, the surgeon performed his first operation for the treatment of lung cancer in May 2017. Uniportal VATS had never before been performed at our hospital.
Surgical procedures
Working incision and instruments
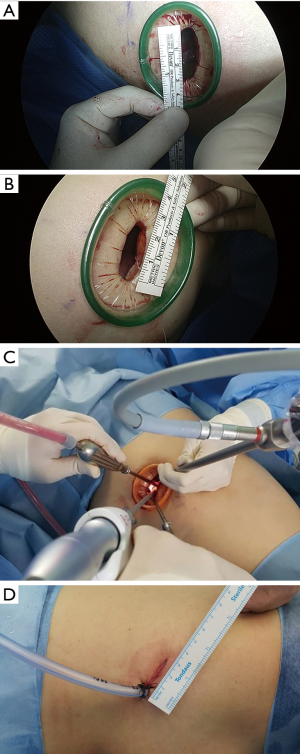
A skin incision was usually made in the 5th intercostal space between the mid- and anterior axillary lines. For right upper lobectomy, however, the 4th intercostal space was chosen. The incision length was usually 3 to 3.5 cm (Figure 1A,B). For masses larger than 3 cm, to allow removal of the resected lobe of the lung through the incision site, the working incision was extended to 4 to 5 cm. In most cases, however, the working incisions were no larger than 4 cm. The 30° high definition thoracoscope was always located at the top of the working wound. An energy device (HARMONIC ACE®) and curved long suction device (SCANLAN® Wolf Suction Instrument 9009-912) were located in the middle of the wound. The lung was retracted with a lung grasping clamp or suction device that was located in the lowest portion of the working wound (Figure 1C). After surgery, the chest tube was inserted into the thoracic cavity through the working incision, and the incision was closed layer-by-layer (Figure 1D).
Surgical techniques for pulmonary resection
The curved suction device plays the most important role in dissection of the tissue. Using the curved suction device and the straight energy device, the surgeon achieves an unobscured field of view. The suction device both aspirates the surrounding blood and pushes or pulls the surrounding tissues, facilitating tissue dissection (Figure 2A). Large vessels were divided with staplers. Small vessels were ligated with silk string or clips and divided with the energy device.
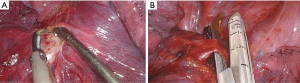
For upper lobectomy, the operation usually began with a hilar dissection, which easily exposes anterior and apical branches of the pulmonary artery. Then, by changing the angle of the stapler to orient the anvil into the proximal portion of the vessel, the vessels can be easily divided (Figure 2B). After dividing the anterior and apical branches of the pulmonary artery, the superior pulmonary vein can be divided by a stapler at the same angle. Finally, after dissection of the lymph nodes around the lobar bronchus, the bronchus was divided. For lower lobectomy, fissure dissection occurred first to expose the interlobar pulmonary artery. After division of the pulmonary artery, the lower lobe bronchus was easily divided with a stapler. The inferior pulmonary vein was the last structure to be divided during lower lobectomy.
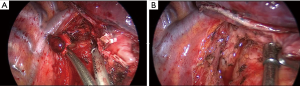
Lymph node dissection was performed in every patient by en bloc resection of the lymph nodes and adjacent fat tissues. The lymph nodes were dissected using a non-grasping technique, which involved dissection of the surrounding tissue with an energy device, using a suction device for pushing or pulling without grasping the lymph nodes (Figure 3). Uniportal VATS segmentectomy was performed in the same way as in multiportal VATS. The segmental branch of the pulmonary artery was found and divided first. Next, the segmental bronchus was found by the same route and divided with a stapler. Lastly, the segmental vein was divided. The segmental planes were then all divided by staplers.
Statistical analysis
The clinicopathological characteristics and surgical outcomes of uniportal VATS were defined and compared with those of multiportal VATS. The Student t-test or Wilcoxon rank-sum test was used for continuous variables, and the χ2 test or Fisher exact test was applied for categorical variables. A P value <0.05 was considered statistically significant.
Results
Surgical outcomes of uniportal VATS
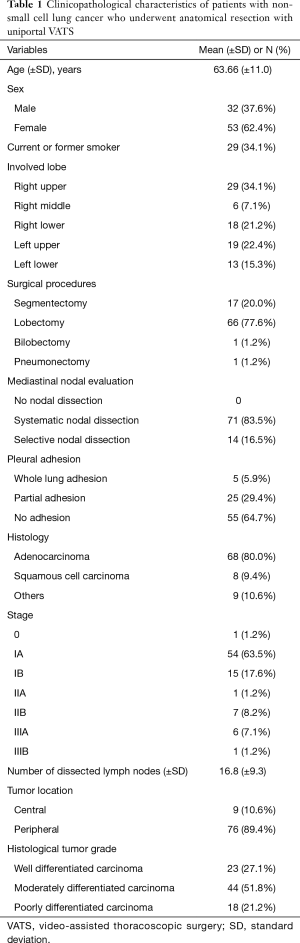
Table 1 shows the clinicopathological characteristics of the patients with NSCLC who underwent uniportal VATS anatomical pulmonary resection. Segmentectomy was performed in 17 patients (left upper lobe upper division segmentectomy, 7 patients; right upper lobe posterior segmentectomy, 4 patients; right lower lobe basal segmentectomy, 2 patients; and right upper lobe apicoposterior segmentectomy, right upper lobe apical segmentectomy, left lower lobe superior segmentectomy, and left lower lobe basal segmentectomy in 1 patient each). Lobectomy was performed in 66 patients, and bilobectomy and pneumonectomy were performed in 1 patient each. Systematic nodal dissection was performed in 71 patients (83.5%). The others (16.5%) underwent lobe-specific nodal dissection (15). Five patients had whole lung adhesions between the visceral and parietal pleurae. All uniportal VATS cases were completed without conversion to multiportal VATS or open thoracotomy.
Full table
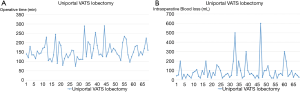
Table 2 shows the perioperative and postoperative outcomes of uniportal VATS. Postoperative complications occurred in 18 patients (21.2%). All complications were completely resolved before discharge from the hospital except for 2 cases of acute respiratory distress syndrome (ARDS). Of the 2 patients with ARDS, 1 had interstitial lung disease and the other had hypothyroidism. Both patients underwent lobectomy and the procedures were uneventful. However, 3 days postoperatively, both patients developed progressive, fatal pulmonary edema. Table 3 shows the comparison of surgical outcomes of lobectomy according to which of the 5 lobes were resected; no significant difference among the 5 lobes was identified. The operative time (Figure 4A) and intraoperative blood loss (Figure 4B) of uniportal VATS lobectomy tended to be similar from the first operation to the last operation even though the number of operations increased over time.
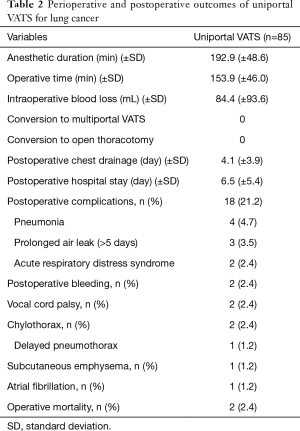
Full table
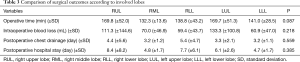
Full table
Comparison of surgical outcomes between uniportal VATS and multiportal VATS
Table 4 shows the comparison of clinicopathological characteristics in patients undergoing uniportal VATS or multiportal VATS for the treatment of NSCLC. Patients who underwent multiportal VATS were older, more often male, and more often smokers than those who underwent uniportal VATS. There were no differences between the two groups in terms of tumor location, surgical procedures, pleural adhesion, tumor histology, stage, tumor histologic grade, and neoadjuvant chemotherapy. The number of dissected lymph nodes was higher in uniportal VATS than in multiportal VATS (16.8 vs. 14.6, P=0.030).

Full table
Table 5 shows the comparison of perioperative and postoperative outcomes in patients undergoing uniportal VATS or multiportal VATS. Anesthetic time and operative time were shorter in uniportal VATS than in multiportal VATS (P<0.001 and P<0.001, respectively). Less intraoperative blood loss occurred in uniportal VATS than in multiportal VATS (P<0.001). There was no conversion to multiportal VATS or open thoracotomy in the uniportal VATS group, but conversion to open thoracotomy occurred in 24 patients (8.9%) in the multiportal VATS group (P=0.005). There were no significant differences between the two groups in chest tube drainage period, hospital stay, postoperative complication rate, and operative mortality rate.
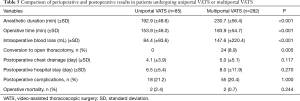
Full table
Discussion
Uniportal VATS lobectomy was first performed in 2011 by Gonzalez et al. (16). Since his initial report, uniportal surgery has been actively performed for anatomical pulmonary resection in the treatment of lung cancer. Uniportal VATS has been considered more difficult than multiportal VATS because the operation is performed by inserting 2 or 3 surgical instruments and the thoracoscope into only one incision. Therefore, it has been thought that a surgeon can perform uniportal VATS only after fully learning the multiportal VATS technique. However, the uniportal technique has evolved considerably (10). The 30° thoracoscope placed at the top of the wound provides an optimal field of view similar to that of actual open thoracotomy (10). Moreover, if the surgery is done in the order determined for each lobe using a long-curved suction device and energy device, the operation can be performed relatively easily and quickly. Also, if the suction device is used for aspiration as well as multiple other functions (e.g., to hold, dissect, expose, and compress), there is no need for an additional port.
In this study, one junior surgeon performed uniportal VATS using the technique developed by Gonzalez et al. (10,14,17). The operations were performed with uniportal VATS for all lung cancer surgeries, without conversion to multiportal VATS, even in 5 patients with whole lung adhesion who underwent complete pleural adhesiolysis. Systematic nodal dissection was done for all lobectomy cases. When the lesion was a ground glass nodule, lobe-specific nodal dissection was done because of the low possibility of nodal upstaging (4,18). All patients underwent mediastinal lymph node dissection. Six patients were diagnosed with stage IIIA and 1 patient was diagnosed with stage IIIB cancer; those patients underwent complete en bloc resection of lymph nodes including adjacent fat tissues. Mediastinal lymph node dissection was not more difficult in uniportal VATS than in multiportal VATS. In this study, the mean number of dissected lymph nodes in uniportal VATS was 16.8, which was higher than in multiportal VATS.
In the comparison of the uniportal and multiportal VATS groups, clinicopathological characteristics differed only for age, sex, and smoking history. The older patients more often were male and more often were smokers. Such older patients tended to prefer senior surgeons who performed multiportal VATS. Although this study was not a comparison between well-matched groups, there were no significant between-group differences in lung cancer characteristics.
The frequency of pleural adhesion or chronic lung disease, which can increase the difficulty of surgery, is high in older patients, men, and patients with a current or past history of smoking. Therefore, the surgical outcomes between the two groups cannot be accurately compared. Nevertheless, the comparison of surgical outcomes between the uniportal and multiportal VATS groups yielded useful information. Anesthesia duration and operative time were shorter and intraoperative blood loss was reduced in the uniportal VATS group. These findings do not indicate that uniportal VATS is superior to multiportal VATS; rather, they indicate that uniportal VATS is not a more difficult or lengthy procedure than multiportal VATS. Therefore, this study was not intended to compare the surgical results between the two groups, and was intended to show the surgical results of uniportal VATS. The surgical results of multiportal VATS are only reference values. A review of 22 articles on uniportal lung cancer surgery reported a mean operative time of approximately 150 minutes (range, 95.3–198.8 minutes) (19). In our study, the mean operative time was 153.9 minutes, and other results (intraoperative blood loss, postoperative chest drainage, and hospital stay) were also comparable with those previously reported (19). Therefore, we conclude that the uniportal VATS can be performed without great difficulty by a surgeon who lacks primary operative experience with multiportal VATS.
In this study, there was no conversion to open thoracotomy in the uniportal VATS group. In contrast, conversion was required in 8.9% of patients in the multiportal VATS group. As previously discussed, this is not a comparative study of surgical outcomes of uniportal and multiportal VATS. Rather, we sought to evaluate the surgical outcomes of uniportal VATS procedures performed by a surgeon who did not have previous experience performing multiportal VATS. Therefore, the comparison between the two groups was for reference purposes only, and the single meaningful observation is that the conversion rate with uniportal VATS was not significantly high.
After 4 years of clinical fellowship at a tertiary hospital as a first assistant for more than 400 cases of open thoracotomy or multiportal VATS for lung cancer, the author was able to independently perform uniportal VATS for pulmonary anatomical resection. Previously regarded as uncomfortable, difficult procedures affording a limited view of the surgical field, uniportal VATS became more widely accepted after development of the Gonzalez-Rivas approach. Young surgeons participating in uniportal VATS training, such as that provided at Shanghai Pulmonary Hospital (11) may readily learn to perform these procedures. Further, numerous surgery videos are available free of charge on many websites, making it easier to learn how to perform uniportal VATS. These resources enable young surgeons to independently perform uniportal VATS.
This study has several limitations. First, the unmatched comparison groups, in which one surgeon performed uniportal VATS and multiple surgeons performed multiportal VATS, limited the comparability and generalizability of the outcomes. Also, the clinicopathological characteristics slightly differed between the groups. However, the objective was to demonstrate the outcomes when a young surgeon initially performs uniportal VATS instead of open thoracotomy or multiportal VATS. Therefore, rather than comparing features of uniportal and multiportal VATS, the intention was to show that even a novice surgeon can independently perform uniportal VATS. Second, this study was retrospective. However, the hospital has implemented a longstanding electronic medical record system in which the detailed medical records and surgical pictures were stored, so that all the data can be easily reviewed. Therefore, there was no limit for analyzing the surgical results. Future prospective and randomized trials are warranted to obtain more accurate results. Third, only limited conclusions can be derived from the results of this study of uniportal VATS performed by one young surgeon. Therefore, it is difficult to generalize the results of this study. In the future, as young surgeons actively practice uniportal VATS, it will likely become clearer that uniportal VATS is not a difficult surgical method to learn.
Conclusions
In conclusion, surgical outcomes of uniportal VATS for pulmonary anatomic resection for the treatment of lung cancer performed by a surgeon with limited previous experience were not inferior to those of multiportal VATS performed by experienced surgeons. Even a surgeon who has never performed a uniportal VATS operation can do so after extensive experience assisting with multiple other types of lung surgery. The available training programs and materials explaining the standardized uniportal VATS techniques of Diego Gonzalez-Rivas can be easily followed, even by less experienced surgeons, enabling the wider implementation of uniportal VATS.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The author has completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/jtd-20-242.
Conflicts of Interest: The author has completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jtd-20-242). The author has no conflicts of interest to declare.
Ethical Statement: The authors is accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study was approved by the institutional review board of Eunpyeong St. Mary’s Hospital at the Catholic University of Korea and individual consent was waived (Referral number: PC19RISI0157).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Howington JA, Blum MG, Chang AC, et al. Treatment of stage I and II non-small cell lung cancer: Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 2013;143:e278S-e313S.
- Konge L, Petersen RH, Hansen HJ, et al. No extensive experience in open procedures is needed to learn lobectomy by video-assisted thoracic surgery. Interact Cardiovasc Thorac Surg 2012;15:961-5. [Crossref] [PubMed]
- Moon Y, Park JK, Lee KY, et al. Prognosis after wedge resection in patients with 8(th) edition TNM stage IA1 and IA2 non-small cell lung cancer. J Thorac Dis 2019;11:2361-72. [Crossref] [PubMed]
- Moon Y, Park JK, Lee KY, et al. Consolidation/Tumor Ratio on Chest Computed Tomography as Predictor of Postoperative Nodal Upstaging in Clinical T1N0 Lung Cancer. World J Surg 2018. [Crossref] [PubMed]
- Handy JR Jr, Asaph JW, Douville EC, et al. Does video-assisted thoracoscopic lobectomy for lung cancer provide improved functional outcomes compared with open lobectomy? Eur J Cardiothorac Surg 2010;37:451-5. [PubMed]
- Whitson BA, Andrade RS, Boettcher A, et al. Video-assisted thoracoscopic surgery is more favorable than thoracotomy for resection of clinical stage I non-small cell lung cancer. Ann Thorac Surg 2007;83:1965-70. [Crossref] [PubMed]
- Whitson BA, Groth SS, Duval SJ, et al. Surgery for early-stage non-small cell lung cancer: a systematic review of the video-assisted thoracoscopic surgery versus thoracotomy approaches to lobectomy. Ann Thorac Surg 2008;86:2008-16; discussion 16-8.
- Sihoe AD. The evolution of minimally invasive thoracic surgery: implications for the practice of uniportal thoracoscopic surgery. J Thorac Dis 2014;6:S604-17. [PubMed]
- Hirai K, Takeuchi S, Usuda J. Single-incision thoracoscopic surgery and conventional video-assisted thoracoscopic surgery: a retrospective comparative study of perioperative clinical outcomesdagger. Eur J Cardiothorac Surg 2016;49 Suppl 1:i37-41. [PubMed]
- Gonzalez-Rivas D, Sihoe ADL. Important Technical Details During Uniportal Video-Assisted Thoracoscopic Major Resections. Thorac Surg Clin 2017;27:357-72. [Crossref] [PubMed]
- Sihoe ADL, Gonzalez-Rivas D, Yang TY, et al. High-volume intensive training course: a new paradigm for video-assisted thoracoscopic surgery education. Interact Cardiovasc Thorac Surg 2018;27:365-71. [Crossref] [PubMed]
- Gonzalez-Rivas D, Yang Y, Ng C. Advances in Uniportal Video-Assisted Thoracoscopic Surgery: Pushing the Envelope. Thorac Surg Clin 2016;26:187-201. [Crossref] [PubMed]
- Gonzalez-Rivas D. Uniportal thoracoscopic surgery: from medical thoracoscopy to non-intubated uniportal video-assisted major pulmonary resections. Ann Cardiothorac Surg 2016;5:85-91. [Crossref] [PubMed]
- Gonzalez-Rivas D, Fieira E, Delgado M, et al. Uniportal video-assisted thoracoscopic lobectomy. J Thorac Dis 2013;5 Suppl 3:S234-45. [PubMed]
- Adachi H, Sakamaki K, Nishii T, et al. Lobe-Specific Lymph Node Dissection as a Standard Procedure in Surgery for Non-Small Cell Lung Cancer: A Propensity Score Matching Study. J Thorac Oncol 2017;12:85-93. [Crossref] [PubMed]
- Gonzalez D, Paradela M, Garcia J, et al. Single-port video-assisted thoracoscopic lobectomy. Interact Cardiovasc Thorac Surg 2011;12:514-5. [Crossref] [PubMed]
- Hernandez-Arenas LA, Purmessur RD, Gonzalez-Rivas D. Uniportal video-assisted thoracoscopic segmentectomy. J Thorac Dis 2018;10:S1205-s14. [Crossref] [PubMed]
- Moon Y, Sung SW, Namkoong M, et al. The effectiveness of mediastinal lymph node evaluation in a patient with ground glass opacity tumor. J Thorac Dis 2016;8:2617-25. [Crossref] [PubMed]
- Sihoe ADL. Uniportal Lung Cancer Surgery: State of the Evidence. Ann Thorac Surg 2019;107:962-72. [Crossref] [PubMed]


