Double lung point in an 18-month-old child: a case report and literature review
Introduction
Ultrasound has been utilized for assessment of pneumothorax in clinical practice for nearly two decades and its diagnostic performance has been demonstrated to be optimal (1). By using computed tomography (CT) as the “gold standard”, its sensitivity and specificity can reach as high as 95% and 100%, respectively (2). The most specific sign to confirm pneumothorax is the “lung point” which is generated by the inspiratory increase in the volume of collapsed lung (3). In typical situation, the air floats to the anterior-inferior chest zone of a supine patient, and the size of pneumothorax can be estimated by the location of lung point. However, in certain situations, there can be some variations of the typical sign of lung point. I describe here a double lung point sign in an 18-month old child who suffered from severe pneumonia.
Case presentation
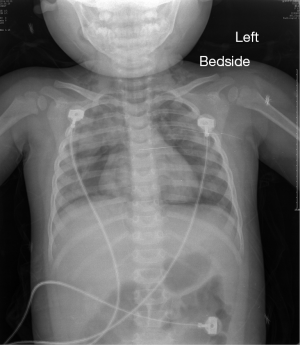
An 18-month-old female child was presented to the emergency department for febrile and productive cough for 6 days. On physical examination, she appeared weak and sluggish. The heart rate was 153 beats/min, blood pressure was 116/76 mmHg, temperature was 38.4 °C, and the pulse oxygenation was 93% on 6 L/min oxygen mask. A chest X-ray was immediately obtained and the result showed bilateral inflammatory infiltrates and pneumothorax (Figure 1). She was then transferred to the intensive care unit (ICU) for further monitoring and management. On the way to the ICU, a CT was obtained. The result of CT scan showed bilateral pneumothorax with 30% compression on the right side and less than 10% on the left side, and there were inflammatory infiltrates in both lungs (Figure 2).

The patient’s condition continued to deteriorate with respiratory distress and pulse oxygenation dropped to 76%. Emergent tracheal intubation was performed and mechanical ventilation was instituted. Thoracentesis was attempted and closed thoracic drainage was performed on the right side, but no gas was drawn on the left side. Due to the rapid respiratory rate despite mechanical ventilation, vecuronium was used for muscular relaxation. Analgesia and sedation were routinely instituted. Because there was pneumothorax found in CT scan and high inspiratory pressure, the extension of the pneumothorax should be suspected. Repeated portable ultrasonography was performed by experienced intensivist. The patient was assumed a supine position and the examination was started by scanning the anterior chest with a 7.5 MHZ probe (M-turbo, Sonosite, Washington, USA) (Figure 3). As shown in the video, there were two lung points on both sides of the screen. Between these two points, there was no lung sliding or B-line suggesting separation of visceral and parietal pleura. Laterally to the points, the pleural sliding and B-line sign were evident. Both lung points moved simultaneously with respiration.
The oxygenation continued to deteriorate and the child died in 36 hours after ICU admission.
Discussion
Lung point is a well-described sign on chest ultrasonography that if present has 100% specificity for the diagnosis of pneumothorax, and its sensitivity is superior to the chest X-ray (5,6). However, the diagnostic value of lung point may be compromised by the coexistence of subcutaneous emphysema, pleural calcifications, obese body habitus and thoracic dressing. Owing to complex conditions in the chest, some variations of lung point for pneumothorax are present (7). Among them the double lung point sign is an interesting sign that is rare in clinical practice. The term “double lung point” has been used to describe another completely different ultrasonographic sign in neonate where the patient suffers from transient tachypnea (8,9). However, this phenomenon was later renamed as “double transition point” by expert’s opinion. Therefore, I still used the term “double lung point” in the present study.
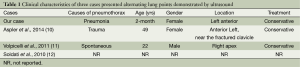
To the best of our knowledge, the double lung point sign has been reported in three cases in the literature (Table 1). One is a 49-year-old woman with occult pneumothorax in lung apex after trauma, and this case was confirmed by CT imaging (10). Another case is a 22-year-old male with spontaneous pneumothorax in right apex (11). The third case was not reported in a formal pattern, but it is mentioned with several sentences and a figure by the author in a letter to the editor. Thus, the clinical background of this is unknown (12). One common feature of the pneumothorax presented as double lung point is that the volume of gas is limited and invasive procedure for air drainage is not required. In two cases, the pneumothorax was observed and closely monitored and it absorbed spontaneously without any invasive procedure. The clinical outcome is generally good. In our case, the emergent condition was suspected to be associated with the pneumothorax and thoracentesis was attempted in the hope that it could relieve the emergency. However, no gas was drawn even under a skillful hand by a senior thoracic surgeon.
One important point in assessment of pneumothorax is to quantify its size. The plain chest X-ray is limited at this point and occult pneumothorax with small volume gas is often missed. Ultrasound is able to detect such occult pneumothorax and a little evidence suggests the position of lung point is able to differentiate between large and small pneumothorax. It is thought that the more laterally the lung point locates, the larger the size of pneumothorax would be. This notion was first hypothesized by Lichtenstein and then demonstrated in human Volpicelli et al. in a recent study (13,14). In an animal experiment, Oveland and coworkers (15) demonstrated a linear relation between the pneumothorax size and the lateral position of the lung point, and the relationship was comparable to that obtained by CT scan. However, there was uncertainty on the quantification of pneumothorax volume with conventional lung point. In the 2012 international evidence-based recommendations for point-of-care lung ultrasound, the statement “Bedside lung ultrasound is a useful tool to differentiate between small and large pneumothorax, using detection of the lung point” was assigned as grade C evidence without consensus (16). Herein, I propose that the presence of double lung point indicates limited pneumothorax and conservative management may well be attempted, which is supported by our case as well as by other cases as summarized in Table 1.
Full table
In aggregate, I reported the first case of double lung point in pediatric patient and the strength of our report is that pneumothorax was validated by CT scan. This finding supplemented the common form of lung point. Clinical implication of identifying double lung point is that the size of pneumothorax is small and surgical procedure may not be helpful.
Acknowledgements
Disclosure: The author declares no conflict of interest.
References
- Lichtenstein DA. Lung ultrasound in the critically ill. Ann Intensive Care 2014;4:1. [PubMed]
- Lichtenstein DA, Menu Y. A bedside ultrasound sign ruling out pneumothorax in the critically ill. Lung sliding. Chest 1995;108:1345-8. [PubMed]
- Lichtenstein D, Mezière G, Biderman P, et al. The “lung point”: an ultrasound sign specific to pneumothorax. Intensive Care Med 2000;26:1434-40. [PubMed]
- Zhang Z. The ultrasound demonstrated double lung point on 3-5 intercostal space of the left side of the chest, along the anterior axillary line. Asvide 2015;015. Available online: http://www.asvide.com/articles/467
- Burns BJ, Aguirrebarrena G. Occult traumatic loculated tension pneumothorax--a sonographic diagnostic dilemma. Prehosp Emerg Care 2013;17:92-4. [PubMed]
- Alrajab S, Youssef AM, Akkus NI, et al. Pleural ultrasonography versus chest radiography for the diagnosis of pneumothorax: review of the literature and meta-analysis. Crit Care 2013;17:R208. [PubMed]
- Volpicelli G, Boero E, Stefanone V, et al. Unusual new signs of pneumothorax at lung ultrasound. Crit Ultrasound J 2013;5:10. [PubMed]
- Copetti R, Cattarossi L. The ‘double lung point’: an ultrasound sign diagnostic of transient tachypnea of the newborn. Neonatology 2007;91:203-9. [PubMed]
- Verniquet A, Kakel R. About ultrasound in pneumothorax. Am J Emerg Med 2011;29:833-4. [PubMed]
- Aspler A, Pivetta E, Stone MB. Double-lung point sign in traumatic pneumothorax. Am J Emerg Med 2014;32:819.e1-2.
- Volpicelli G, Audino B. The double lung point: an unusual sonographic sign of juvenile spontaneous pneumothorax. Am J Emerg Med 2011;29:355.e1-2.
- Soldati G, Sher S, Copetti R. If you see the contusion, there is no pneumothorax. Am J Emerg Med 2010;28:106-7; author reply 107-8. [PubMed]
- Lichtenstein DA. Ultrasound in the management of thoracic disease. Crit Care Med 2007;35:S250-61. [PubMed]
- Volpicelli G, Boero E, Sverzellati N, et al. Semi-quantification of pneumothorax volume by lung ultrasound. Intensive Care Med 2014;40:1460-7. [PubMed]
- Oveland NP, Lossius HM, Wemmelund K, et al. Using thoracic ultrasonography to accurately assess pneumothorax progression during positive pressure ventilation: a comparison with CT scanning. Chest 2013;143:415-22. [PubMed]
- Volpicelli G, Elbarbary M, Blaivas M, et al. International evidence-based recommendations for point-of-care lung ultrasound. Intensive Care Med 2012;38:577-91. [PubMed]


