Primary pulmonary cancer colliding with metastatic choriocarcinoma
Introduction
A collision tumor, which is a special entity of multiple primary cancers, is defined as two independent malignant neoplasms invading each other, and they have been reported in various primary sites. The two malignant neoplasms may originate from the same primary site or occur as metastases from other organs. There is no histological admixture or intermediate-transition cell population zone. These tumors are not easy to diagnose before operation and pathological identification of the dual components is usually the only method to make a clear diagnosis (1).
Choriocarcinoma is the most curable metastatic neoplasm because of its high chemotherapy sensitivity. However, mortality due to respiratory failure from metastatic choriocarcinoma remains high. About 60% of patients with choriocarcinoma developed pulmonary metastases (2,3). Although the development of effective chemotherapy has resulted in improved survival of patients with gestational trophoblastic tumor, lung lobectomy remains an important adjunct treatment in a selected subset of patients (4). Surgical resection is an effective therapeutic method for patients with drug-resistant and recurrent gestational trophoblastic neoplasia in the management of pulmonary metastatic disease (5).
There have been case reports of pulmonary collision tumors with various combinations of components, including: large-cell carcinoma and adenocarcinoma; squamous-cell carcinoma and T-cell lymphoma; adenocarcinoma and typical carcinoid; adenocarcinoma and metastatic adenoid cystic carcinoma; adenocarcinoma and metastatic breast carcinoma; squamous-cell carcinoma and metastatic breast carcinoma. But our study is the first report that describes a case of collision cancer in the lung consisting of a squamous-cell lung carcinoma (SCC) and a metastatic choriocarcinoma diagnosed by immunohistochemical techniques after surgery.
Case report
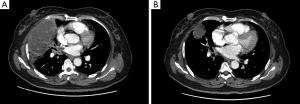
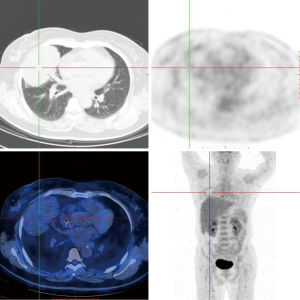
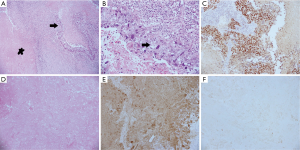
A 55-year-old, non-smoking mother of two children with a previous history of choriocarcinoma with lung metastasis (cIIIb) that had been treated by chemotherapy was admitted to our department after referral from her gynecologist. The patient underwent therapy with a BEP regimen (BLM, VP-16, DDP). In the course of the chemotherapy, the β-hCG decreased from 16,500 to 102.95 mIU/mL. In the primary survey, a computed tomography (CT) scan showed a 12.0 cm × 6.5 cm × 8.0 cm mass, with irregular morphology in the right middle lobe where pulmonary obstructive pneumonia occurred. In addition, a possible tumor embolus was revealed in the vein of the right middle lobe and the intersection between the right superior pulmonary vein and the left atrium (Figure 1). A positron emission tomography (PET) demonstrated a focus of low grade FDG uptake in the right middle lobe (Figure 2). Two cycles of chemotherapy later, a transbronchial biopsy was performed, demonstrating an area of coagulative necrosis. The coagulative necrosis strongly expressed Cytokinetic AE1/AE3, Cytokinetic 7 and HCG, but showed no significant reactivity with HPL (Figure 3). With these features, immunohistochemical stigmas of trophoblastic tumor were diagnosed. After seven circles of chemotherapy, the CT scan showed that the size of the mass decreased to 4.9 cm × 3.5 cm × 3.9 cm and the tumor embolus disappeared (Figure 1).

Based on the findings mentioned above, a right middle lobectomy with a partial resection of the superior lobe was performed on February 10th, 2014. No pleural effusion, dissemination, or pulmonary metastasis was observed. Given that the tumor was a metastasis, mediastinal lymph node dissection was not performed. The postoperative course was uneventful, and the patient was discharged on the 4th day after the operation.
Gross pathologic examination of the resected tumor indicated that it measured 5.5 cm × 3.8 cm × 3.5 cm and was pale grey with a gritty cut surface. A histopathologic examination showed that the carcinoma was composed of two histologic, distinct subtypes, which consisted of a poorly differentiated squamous-cell carcinoma and a great sheet of coagulative necrosis of choriocarcinoma, but no chorionic villus was detected. The SCC showed moderate reactivity with p63 but no significant reactivity with thyroid transcription factor-1 (TTF-1). And the tumor adjacent to the SCC consisted of coagulative necrosis and it showed moderate staining of HCG and AE1/3. Considering the patient’s medical history and the pathological diagnosis of the biopsy, this latter tissue was identified as a metastatic choriocarcinoma of lung. Based on these findings, we diagnosed a collision tumor of lung. No metastatic lesion could be observed in the resected regional lymph nodes. The two tumors did appear to be separate in which the neoplastic cells were not intimately admixed with one another (Figure 4). They did appear to buttress one another and formed one aggregate grossly and radiologically indistinguishable solitary mass. Therefore, a diagnosis of a true collision tumor of a SCC with that of a metastatic choriocarcinoma was made. Both tumors were staged separately. The squamous carcinoma of lung was pT2bN0M0 (stage IIa) and cIIIb for choriocarcinoma as it was a metastasis to the lung and the size of the tumor was over 3 cm. Considering that the rest of the tumor was lung squamous carcinoma, and that systematic mediastinal lymphadenectomy was not performed in the operation, we selected docetaxel and nedaplatin in the postoperative adjuvant chemotherapy scheme. A cycle of chemotherapy later, the chemotherapy regimen was adjusted and gemcitabine and cisplatin were administered. After three cycles of this chemotherapy, a CT scan showed a new lesion in the upper lobe of the right lung and the β-hCG increased from 463.16 to 800.90 mIU/mL. Given that the choriocarcinoma is resistant to gemcitabine and cisplatin, we adjusted the chemotherapy regimen again and the preoperative chemotherapy regimens of BEP were used. Two cycles of this chemotherapy later, the β-hCG decreased from 800.90 to 92.37 mIU/mL. In the second course of the BEP regimen, a III degree myelosuppression occurred in the patient. So the patient received hypodermic injections of rhIL-11 till the number of thrombocytes returned to a normal level. The patient is alive after lung resection and the regular follow-up is taken in the out-patient department.
Discussion
Collision tumors have been reported in various organs such as cervix, anorectal junction, oral cavity, liver, urinary bladder, and gastroesophageal junction. Cancer-to-cancer metastasis is a well-known, though exceedingly rare, form of collision neoplasm in the lung. In general, renal cell carcinoma and lung cancer are, respectively, the most common recipient and donor in tumor-to-tumor metastases (6).
The occurrence of multiple malignancies in the same anatomical site in organs such as the thyroid, breast and lymph nodes has been previously described (7). In the lung, single cases of pulmonary carcinoma have been unexpectedly found when pulmonary resection was performed for metastatic lung cancer (8). In spite of this, the occurrence of synchronous colliding tumors remains an extremely uncommon condition with a very limited number of cases having been published in the literature.
The therapeutic scheme is mainly targeted at the more aggressive component in the tumors (in this case, the SCC). Although collision tumors may represent an incidental curiosity or an academic exercise, sometimes they may cause important clinical dilemmas. Identification of the more aggressive tumor component is crucial to establishing the appropriate therapeutic strategies. In our case, the patient was diagnosed with a metastatic choriocarcinoma and got relevant treatments after the lung malignancy was completely excised.
It is difficult to diagnose pulmonary collision tumors before performing a surgical resection due to their lack of characteristic clinical features. Also the diagnosis of pulmonary collision tumor generally requires ample tissue such as wedge resection or lobectomy to clearly evaluate entire process with the extent of each tumor relative to each other (9). In our case, a chest CT scan showed a mass with obstructive pneumonia. In the resected specimen, the SCC and necrosis of choriocarcinoma abutted each other macroscopically but were separated microscopically. At the point of collision, there were no histological transitional features. We believe that up till now there have not been any reports in the literature about a collision tumor of lung that consists of SCC and metastatic choriocarcinoma.
In conclusion, a variant of cancer-to-cancer collision tumor of the lungs consisting of SCC and metastatic choriocarcinoma is described in this study. The diagnosis requires a careful morphologic examination, especially when patients have experienced extra-thoracic tumors previously. Appropriate therapy in such cases needs a balanced evaluation of the more aggressive component. Tumor stage and molecular analysis of predictive biomarkers may be misled when a cancer-to-cancer metastasis is missed (10).
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Willis RA. Structure and growth of tumors. In: Willis RA. eds. Pathology of Tumours. London: Butterworth, 1967:138.
- Yang J, Xiang Y, Wan X, et al. The prognosis of gestational trophoblastic neoplasia patient with residual lung tumor after completing treatment. Gynecol Oncol 2006;103:479-82. [PubMed]
- Song HZ, Wu BZ, Tang MY, et al. A staging system of gestational trophoblastic neoplasms based on the development of the disease. Chin Med J (Engl) 1984;97:557-66. [PubMed]
- Ren T, Xiang Y, Yang XY, et al. Evaluation of surgical resection of pulmonary metastasis of trophoblastic tumour. Zhongguo Yi Xue Ke Xue Yuan Xue Bao 2003;25:418-21. [PubMed]
- Cao Y, Xiang Y, Feng F, et al. Surgical resection in the management of pulmonary metastatic disease of gestational trophoblastic neoplasia. Int J Gynecol Cancer 2009;19:798-801. [PubMed]
- Lin WY, Hsu WH. Tumor-to-tumor metastasis: maxillary sinus adenoid cystic carcinoma metastasizing to double primary lung adenocarcinoma. Ann Thorac Surg 2010;90:e59-61. [PubMed]
- Pandey U, Naraynan M, Karnik U, et al. Carcinoma metastasis to unexpected synchronous lymphoproliferative disorder: report of three cases and review of literature. J Clin Pathol 2003;56:970-1. [PubMed]
- Kanemitsu S, Takao M, Shimamoto A, et al. Synchronous primary lung carcinoma and lung metastasis from extrathoracic carcinoma. Ann Thorac Surg 2001;72:270-2. [PubMed]
- Abbi KK, Hameed MK, Jiang Y, et al. Pulmonary collision tumor consisting of adenocarcinoma and typical carcinoid--a case report and review of literature. Am J Ther 2014;21:e234-8. [PubMed]
- Piacentini F, Rossi G, Casali C, et al. Primary pulmonary cancer colliding with metastatic breast carcinoma: hitherto unreported cases of cancer-to-cancer metastasis focusing on clinical implications. Lung Cancer 2011;74:145-8. [PubMed]


