Effect of a combined anti-thrombotic therapy of thrombosis on prosthetic heart valves
Introduction
For patients who have experienced surgical replacements of heart valves, the well-being of the prosthetic valves is important. Since thrombosis can appear on the prosthetic valves especially on mechanical ones, these patient have to receive an anticoagulation therapy which mainly depends on vitamin K antagonist (warfarin) according to the guidelines (1). The international normalized ratio (INR) of pro-thrombin time need to be modulated to 2.0-3.0 for prosthetic aortic valves, and 2.5-3.5 for prosthetic mitral valves (MVs). Even if properly anti-coagulated, some patients still suffer from thrombosis and obstruction of prosthetic valves which is life-threatening. Since some patients are unwilling to receive a second surgery to eliminate the thrombi or to re-replace the concerned valves, we tried a medical treatment for thrombosis on prosthetic valves on a series of cases. It’s a combined anti-thrombotic therapy which consisted of an anti-platelet agent and anticoagulants. Clopidogrel, an adenosine di-phosphate receptor inhibitor (2), was applied in this study as the anti-platelet agent.
Methods
Patients
Twenty-two patients who had complaint of exertional dyspnea, fatigue and chest stuffiness (heart function of NYHA grade 2 to 3) due to thrombosis on prosthetic heart valves (either mechanical ones or bio-prosthetic ones) from April 2006 to April 2012 were enrolled.
Inclusion criteria
Patients who had suffered from thrombi on prosthetic heart valves demonstrated by transesophageal echocardiographies (TEE) and refused to undergo surgeries and signed informed consent including acceptance of medical treatment were included. The informed consent explained that the common treatments of thrombosis on prosthetic valves included surgery and medical treatment. The anti-thrombotic therapy could increase bleeding risks which increases mortality and morbidity, and could be ineffective and still called for a surgery.
Exclusion criteria
Unstable hemodynamics, unstable angina, acute myocardial infarction, within 3 months after revascularization, severe hepatic or renal dysfunction (serum ALT >2.5 folds of upper normal level, serum creatinine >2.0 mg/dL), obvious bleeding tendency (cirrhosis, liver failure, coagulation disorders due to hematologic diseases, cerebral vascular accidents within 6 months, etc.), malignant tumors or uncontrolled diseases of other systems including hyperthyroidism, pulmonary heart disease, acute pulmonary embolism, etc.
Grouping schedule
The patients were divided into two groups, the inpatient group and the outpatient group. The inpatient group would experience a period of hospitalization during the early stage of treatment, and then accept an ambulatory treatment and observation. The outpatient group would experience an ambulatory treatment and observation during the whole treatment.
Study design and follow-ups
For inpatients
The patients were treated in the hospital during the first week, and then treated and followed up in the outpatient department. These patients received clopidogrel (TN: Plavix) 75 mg per day as an anti-platelet agent and warfarin as an anticoagulation agent. And low molecular weight heparin (LMWH, inoxaparin, TN: Clexane, Sanofi, Inc., Paris, France) was given subcutaneously (4000 anti-Xa IU, Q12h) for the first 5 days in addition to clopidogrel and warfarin.
For outpatients
The patients were treated and observed in the outpatient department during the whole period. These patients received clopidogrel (TN: Plavix, Pfizer, Inc., New York, USA) 75 mg per day as an anti-platelet agent and warfarin as an anticoagulation agent.
For both groups
Patients were followed up regularly in the outpatient department. INR (aimed from 2.0 to 3.0) and transthoracic echocardiographies (TTE) were reviewed at least weekly in the first 2 months of the treatment and monthly thereafter. For TTE/TEE detectable thrombi before treatment, if thrombi were undetected by TTE and valvular function recovered to normal after treatment, thrombi were considered disappeared, otherwise they were considered to be existed, no matter enlarged or shrinked. For TTE/TEE undetectable thrombi before treatment, if valvular function recovered to normal, they were considered disappeared, otherwise they were considered to be existed, no matter valvular function improved or not. After a successful treatment (functions of the prosthetic valves recovered to normal and thrombi disappeared), dosage of clopidogrel was reduced to 25 mg per day, together with warfarin to prevent recurrence. Since the combined anti-thrombotic therapy could increase bleeding risks, we observed the patients’ general clinical status (including consciousness, limbs mobility, bleeding symptoms, hemoglobin levels, etc.) carefully during the whole period. If there were severe bleeding phenomena, the therapy would be ceased immediately.
Statistical analysis
The categorical data were expressed in percentages. The continuous variables such as ages, sizes of cardiac chambers, periods were expressed in mean ± SD. Differences of each cardiac chamber and the left ventricular ejection fractions (LVEF) between pre-treatment status and post-treatment status were evaluated by paired t-test. Differences of curative effects between inpatients and outpatients were evaluated by Fisher’s accurate test. Differences of treatment durations between inpatients and outpatients were evaluated by independent sample t-test. P<0.05 was considered significant.
Results
Baseline materials
There were 5 men and 17 women, average age 43±13 years. Twelve patients were enrolled in the outpatient group. Ten patients were enrolled in the inpatient group.
Ten patients had only prosthetic MVs, three had only prosthetic tricuspid valves (TVs), five had prosthetic mitral and aortic valves, three had prosthetic mitral and TVs, and one had a prosthetic MV, a prosthetic aortic valve and a prosthetic V. Thirteen patients suffered from thrombosis on the mechanical MVs, five on the mechanical TVs, one on the mechanical aortic valve and tricuspid bio-prosthetic valve, one on the mechanical aortic valve, one on the mitral bio-prosthetic valve, and one on the tricuspid bio-prosthetic valve. Totally 23 prosthetic valves were involved. TEE detected definitive thrombi on 18 concerned valves of 17 patients with an average size of (9.9±5.0) mm × (7.1±3.6) mm. Table 1 shows the baseline materials of all the patients. For the other five valves without detectable thrombi, confined mobility and obstruction of the valves were observed. According to their history, thrombosis was the most probable problem, so we treated them as thrombosis.
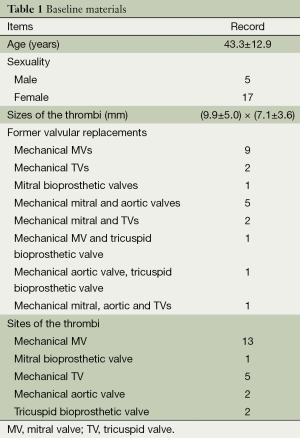
Full table
Analysis of the baseline materials including ages, genders, thrombi sizes, thrombi sites and property of prosthetic valves showed no statistical significant differences were found between the two groups (see Table 2, P >0.05).
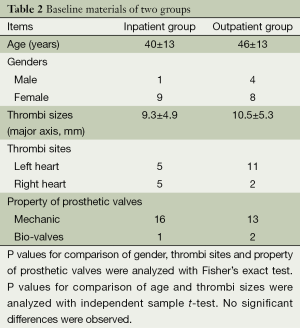
Full table
Outcomes
The thrombi took an average of 32.0±20.4 days on the prosthetic MVs (11 in 14) and average 36.2±20.1 days on the prosthetic TVs (5 in 7) to disappear (The patients whose thrombi did not disappear were excluded here). The thrombus on only 1 of the 2 aortic valves disappeared after 33 days. The average time for all the thrombi to disappear was 33.3±19.7 days (Table 3). After an average of 36.4±23.1 days’ observation, 16 (73%) patients’ valvular function became normal without TTE detectable thrombi during follow-ups, 6 (27%) patients’ valvular function remained abnormal including three patients without TTE detectable thrombi during follow-ups. For the 16 patients whose thrombi disappeared, their symptoms as exertional dyspnea, fatigue and chest stuffiness were relieved simultaneously. Among the six patients whose thrombi still existed, four patients’ symptoms were partially relieved after treatment; the other two patients’ symptom remained the same. One patient who suffered from severe obstruction on the mechanical MV before treatment had remained unimproved after 15 days’ treatment. She then accepted a second surgical valvular replacement, and the thrombus was confirmed to have organized.
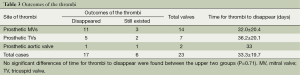
Full table
Comparison between the inpatient group and the outpatient group
For the ten cases in the inpatient group, the time in therapeutic range (TTR) was 54.6%±30.5%. For the 12 cases in the outpatient group, TTR was 51.1%±32.2%. No difference was found between the groups.
For the inpatient group, thrombi disappeared in nine patients, still existed in 1, with an average of 33.7±15.4 days for thrombi to disappear. For the outpatient group, thrombi disappeared in seven, still existed in five, with an average of 35.3±24.6 days for thrombi to disappear. No significant difference was observed in the comparison of outcomes between both groups (P=0.16, counted by Fisher’s exact test). No significant difference was found between both groups in the comparison of average time for thrombi to disappear (P=0.87, analyzed by independent samples t-test) (Table 4).
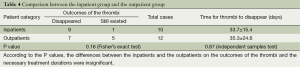
Full table
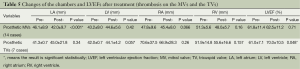
Changes of the chambers and LVEFs after treatment
For the 14 cases with thrombi on the prosthetic MVs, sizes of the left atriums (LAs) decreased an average of 4.1 mm after treatment (95% CI, 1.2-6.9 mm; P<0.001), but there were no obvious changes in other chambers and LVEFs. For the seven cases with thrombi on the prosthetic TVs, there were no obvious changes in all the chambers, but LVEFs improved an average of 10.5% (95% CI, 0.1-17.9%; P=0.048). Table 5 shows the changes of the chambers and LVEFs after treatment.
Full table
Clinical observation of adverse events
None of the patients experienced severe hemorrhages (including intracranial hemorrhages, gastrointestinal and urinary bleedings) during the entire treatment. Only two patients suffered from increased ecchymoses. We stopped clopidogrel and maintained warfarin, and ecchymoses disappeared gradually. No clinical embolizations associated with the thrombi were observed during the treatment.
Discussion
Prosthetic heart valves are foreign materials that can cause thrombosis. Since thrombosis is more likely to appear on mechanical valves although they are more durable than bio-prosthetic ones, such patients require a rigid lifelong anticoagulation.
Activation of clotting factors and platelet contribute to thrombosis. Since the combined anti-thrombotic therapy including anti-coagulants and anti-platelet agents can prevent both aspects of thrombosis, it is likely to obtain better effects than either type of the medicines. But improved effects inevitably lead to increased bleeding risks. Thus, we have to balance the benefits and the risks.
The European and the American guidelines for valvular diseases (3,4) recommended three ways to handle valvular thombosis, including surgery, anti-thrombotic therapy and thrombolytic therapy (5-7). Surgery is an essential method. Some doctors handled the matter by increasing warfarin dosage or applying heparin (8,9). There were some recommendations by the 2012 American College of Chest Physicians Evidence-Based Clinical Practice Guidelines of antithrombotic and thrombolytic therapy for valvular diseases (1): In patients with thrombosed prosthetic valves, fibrinolysis for right-sided valves and left-sided valves with thrombus area below 0.8 cm2 were recommended (grade 2C). For patients with left-sided prosthetic valve thrombosis and thrombus area over 0.8 cm2, early surgery was recommended (grade 2C). The combined anti-thrombotic therapy can enhance autolysis of thrombi. Only a few reports mentioned anti-platelet therapy along with anti-coagulants, such as Rahman et al. (10), who applied abciximab to relieve severe transvalvular gradients for a patient who suffered from thrombi on both the aortic and the mitral prosthetic valves without obvious hemorrhages, and Little et al. (11), who applied aspirin and dipyridamole. Being more risky, fibrinolysis (12,13) usually goes for patients with relatively nice overall status. In 2009, Roudaut et al. (14) presented a retrospective study that compared fibrinolysis to surgery. Their data suggested no difference between the approaches in respect of mortality and hemorrhage, a much higher rate of embolic episodes and less hemodynamic success in the fibrinolysis group.
For the sake of patients’ fear of repeated surgeries and high bleeding risks of fibrinolysis, we tried this combined anti-thrombotic therapy which consisted of anticoagulants and an anti-platelet agent with careful clinical monitoring. General clinical status, INR, TTE findings including sizes of the thrombi and functions of the valves were the main monitored items. We found that the combined anti-thrombotic therapy was quite advantageous. Firstly, it is noninvasive, effective, inexpensive, and also quite safe. But it also has some limitations. It takes days to obtain curative effects, and thus is unsuitable for hemodynamically unstable patients. Some of the irresponsive patients still need surgeries. And it can increase risks of moderate bleedings (two cases suffered from ecchymoses). After successful treatments, the valvular obstructions were resolved and the upstream chambers of the concerned valves could retract due to reduced preload. In our results, diameters of the LAs decreased obviously after dissolving of mitral thrombi. But the data didn’t show obvious right atrium (RA) retraction after dissolving of tricuspid thrombi. This was probably due to small sample sizes. Valvular obstruction could affect cardiac output, but for the hemodynamically stable patients, LVEFs were seldom affected since the LVs were downstream chambers.
Secondly, we recommend early diagnosis of valvular thrombosis in order to obtain better therapeutic effects because fresh thrombi are expected to dissolve more easily. In one of our cases, the thrombus was too “old” to dissolve, so surgery was needed. Meanwhile, since there weren’t any good imaging techniques to indicate accurately whether the thrombi were fresh or not, we didn’t try to confirm whether the thrombi were fresh before enrollment. Fortunately, most patients with valvular thrombosis are symptomatic which will urge them to see a doctor soon when the thombi are still “fresh”. Based on the good effect of the therapy, we suppose that the combined therapy could be carried out without confirming whether thrombi were fresh or not. What surprised us indeed was that it even took months’ for several patients to recover since thrombi could have become organized in such a long period. We attributed this phenomenon to the continuous treatment which might prevent organization of thrombi. Anyhow, it’s advisable that patients get diagnosis and treatments as early as possible. To fulfill this aim, both patients and medical staffs are obliged.
Moreover, totally 20 prosthetic mechanical valves were involved in this study, while only three bio-prosthetic valves were involved. We suppose that mechanical valves are more likely to be thrombosed than bio-prosthetic ones. It is due to the following factors: (I) the gaps between the leaflets and the frames of mechanical valves are suitable locations of thrombi; (II) the movements of mechanical valves destroy blood cells which can stimulate platelet; (III) the metal surface of mechanical valves can activate endogenous coagulation.
Limitations
There are some limitations in this study. Firstly, this study was an uncontrolled, single-center, cohort study. Secondly, sample size was small since such patients were scarce. Thirdly, we didn’t proceed TEE repeatedly during follow-ups which could provide better visualization of valves and thrombi in sake of repeated suffering that would bring forth.
Conclusions
The combined anti-thrombotic therapy based on clopidogrel and warfarin is a feasible treatment of thrombosis on prosthetic heart valves under a close monitoring.
Acknowledgements
Funding: This work was supported by the Natural Science Funding of China (No. 81370295) and the Medical Research Fund of Guangdong Province (No. B2011008).
Authors’ contributions: Taiming Dong designed the overall study; Wei Wei managed the manuscript and statistics, and also followed up the patients; Zhichao Zheng did the echocardiographies during treatments and follow-ups; Shuping Huang nursed the patients and took part in the follow-ups.
Disclosure: The authors declare no conflict of interest.
References
- Whitlock RP, Sun JC, Fremes SE, et al. Antithrombotic and thrombolytic therapy for valvular disease: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 2012;141:e576S-600S.
- Wei Wei, Luo Chufan, Du Zhimin, et al. Inhibitory Effect of Clopidogrel on Release of Soluble CD40 Ligand by ADP-activated Platelet in Patients With Non-ST-segment-elevation Acute Coronary Syndromes. South China Journal of Cardiology 2008;9:66-70.
- Vahanian A, Baumgartner H, Bax J, et al. Guidelines on the management of valvular heart disease: The Task Force on the Management of Valvular Heart Disease of the European Society of Cardiology. Eur Heart J 2007;28:230-68. [PubMed]
- Hirsh J, Guyatt G, Albers GW, et al. Executive summary: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest 2008;133:71S-109S.
- Ozkan M, Kaymaz C, Kirma C, et al. Intravenous thrombolytic treatment of mechanical prosthetic valve thrombosis: a study using serial transesophageal echocardiography. J Am Coll Cardiol 2000;35:1881-9. [PubMed]
- Gupta D, Kothari SS, Bahl VK, et al. Thrombolytic therapy for prosthetic valve thrombosis: short- and long-term results. Am Heart J 2000;140:906-16. [PubMed]
- Roudaut R, Lafitte S, Roudaut MF, et al. Fibrinolysis of mechanical prosthetic valve thrombosis: a single-center study of 127 cases. J Am Coll Cardiol 2003;41:653-8. [PubMed]
- Lengyel M, Horstkotte D, Völler H, et al. Recommendations for the management of prosthetic valve thrombosis. J Heart Valve Dis 2005;14:567-75. [PubMed]
- Mohammed M, Arnaout S, Dakik HA. Prosthetic valve thrombosis with adequate anticoagulation. Int J Cardiol 2007;117:e90-1. [PubMed]
- Rahman AM, Birnbaum Y, Mandava P, et al. Abciximab treatment for obstructive prosthetic aortic and mitral valve thrombosis in the presence of large thrombi, cardiogenic shock, and acute evolving embolic stroke. Echocardiography 2004;21:55-9. [PubMed]
- Little SH, Massel DR. Antiplatelet and anticoagulation for patients with prosthetic heart valves. Cochrane Database Syst Rev 2003;CD003464. [PubMed]
- Shapira Y, Herz I, Vaturi M, et al. Thrombolysis is an effective and safe therapy in stuck bileaflet mitral valves in the absence of high-risk thrombi. J Am Coll Cardiol 2000;35:1874-80. [PubMed]
- Ermis N, Atalay H, Altay H, et al. Comparison of fibrinolytic versus surgical therapy in the treatment of obstructive prosthetic valve thrombosis: a single-center experience. Heart Surg Forum 2011;14:E87-92. [PubMed]
- Roudaut R, Lafitte S, Roudaut MF, et al. Management of prosthetic heart valve obstruction: fibrinolysis versus surgery. Early results and long-term follow-up in a single-centre study of 263 cases. Arch Cardiovasc Dis 2009;102:269-77. [PubMed]


