Epidemiology of thymoma
Thymoma is a rare malignancy which represents only 0.2–1.5% of all malignancies and has an estimated incidence of between 0.13 and 0.32/100,000/year (1,2). Unfortunately, there is limited published literature on which to base a review of the epidemiology of this condition. The majority of data come from relatively small, retrospective, single centre cohort reviews with a small number of population-based studies. However, it is possible to draw some conclusions regarding the observed patterns in this, the commonest tumour of the anterior mediastinum of the chest. Of note, the European RARECARE network, uses cancer registry data from within the EUROCARE projects to assess the incidence, prevalence, and survival of rare cancers in Europe.
Sex
On balance the majority of evidence suggests sex has no influence on the development of the disease (1-4), with some studies suggesting a small predominance in males (5-7), and others describe a small predominance in females (8,9).
Age
Thymoma is not a disease of young adults, but there is reported variation in whether the peak incidence is in middle age, 45–55 years, or as described by Engels et al. incidence peaks in the 7th decade (7). Engels et al. used registry data from the American National Cancer Institute’s Surveillance, Epidemiology and End Results (SEER) programme, between 1973–1998. This database reflects 26% of the American population, and is based on reported malignant diagnoses. Therefore, it is likely that not all cases of thymoma will have been captured by this registry-based system, if clinicians or pathologists have reported a case as benign in behaviour or limited to the thymic capsule. This may influence the patient characteristics reported by Engels, with an older cohort. However, although the population peak incidence was late, the mean age at presentation for this population cohort of 849 cases was still 56 years. Siesling et al. used data from the EUROCRE-4 (1978–2002) network of Cancer Registries in 21 countries of Europe (4). Eleven were national registries, whilst in 10 countries the registries were regional, but the network covered 40% of the total population in these European countries. They reported a higher incidence of thymic cancers in the over 65-year-old group. Several retrospective single centre cohort reviews reported a mean age at diagnosis of 45–55 years; 46 years (6), 46.5 years (9), 48.8 years (3), 51.8 years (5), and 54.7 years (10). The presentation in older patients is in keeping with almost every malignant process, attributed to age-related accumulation of genetic damage. But it is striking that this is the case given the marked reduction in size of the thymus gland itself with age.
Genetic predisposition and ethnicity
There does not appear to be any published literature regarding familial clusters of thymoma, and so a specific genetic mutation driving the development of this malignancy of the thymic gland seems unlikely. However, there is evidence of a variation in incidence between ethnic groups suggesting some level of genetic influence. Engels et al. published results using data from the SEER programme in America in 2003 which documented an increased incidence of thymoma among Blacks and Other ethnic groups compared with Caucasians. The rates reported were; 0.2/100,000 in blacks, 0.29/100,000 in other races, compared with 0.13/100,00 in Caucasians (7). They were able to subdivide ethnicity further for their subsequent publication in 2010, which demonstrated an overall incidence of 0.25/100,000 for Asian and Pacific islanders. Within this ethnic group, specific racial groups were represented; Japanese 0.30/100,000; Vietnamese 0.26/100,000; Filipino 0.18/100,000; Chinese and Korean patients 0.17/100,000 (1). These SEER data were able to demonstrate that the age at diagnosis varied with ethnicity too, with black patients presenting earlier than Caucasians or Asian and Pacific islanders. The median age at diagnosis for black Americans was 48 years, compared with 58 years for Caucasians.
Within Europe there is less detail about ethnic variation but the RARECARE data does show some variation in the incidence of thymic malignancies in different regions of Europe. A higher incidence rate was reported in Central (1.9/million/year) and Southern Europe (2.3/million/year) compared with Northern (0.9/million/year) and Eastern Europe (1.2/million/year) and the UK and Ireland (1.1/million/year) (4). Specific ethnic patterns are not reported, and this may be because there is no single system for recording ethnicity in use amongst cancer registries across Europe.
Exposure
The ideal method to investigate potential causal agents in the development of a condition is a case-control study. This would allow direct comparison between environmental exposures and the development of thymoma. Unfortunately, no such case-control studies have been performed, and it is difficult to see how they would be implemented given the rarity of the condition. Despite the lack of definitive evidence, there are no clear environmental or occupational exposures for the development of thymoma. Nor are there any published data regarding a link between tobacco, alcohol, diet and thymoma.
Studies have been published looking for a possible link between radiation to the chest and the development of thymoma. Two papers report the long-term effects of radiation to infants who received thymic radiation for benign enlarged thymus glands. None of the infants developed thymoma, although there was an increased rate of subsequent thyroid carcinoma (11) and breast cancer (12). In addition, there is no reported increase in the rate of thymoma following radiotherapy to the chest for lung or breast cancer or Hodgkins Lymphoma (1).
Given the intricate role the thymus plays in the immune system, there has been much written about possible links with other haematological disorders, with immunosuppression, and other infections. Viruses are implicated in other rare cancers, such as human herpes virus 8 in Kaposi sarcoma, but evidence in thymoma is limited. Patton et al. describe a case study of a young 15-year-old male who presented with a large anterior mediastinal mass, and histopathology revealed a thymic epithelial tumour. A year after combination chemo-radiotherapy, he developed recurrent disease, and at this stage, investigations revealed a defective Epstein-Barr Virus DNA. They speculate that this could have played a causative role (13). Further evidence of a link between EBV and thymic disease, has reported an association with thymic carcinoma, especially lymphoepithelial subtype, and in thymic lymphoid proliferation itself, rather than conclusive evidence of a link with thymoma (14,15). Other studies reported the detection of DNA from human T-cell lymphotropic virus type I (HTLV-I) and human foamy virus (HFV) in a small number of thymoma tumours, suggesting a potential causative link (16,17). However, in 2004, Li et al. published a study of 21 patients with thymoma and 20 patients with other malignancies, to assess if there was evidence of either of these viral infections. In conclusion they did not find any HTLV-I or HFV DNA sequences in the thymoma tissue examined, nor was there serological evidence of viral infection (18).
A population-based cohort study of individuals with AIDS has been made to review the link between immunosuppression and malignancies. Whilst a predominance of AIDS-related malignancies was seen, within the group of non-AIDS related malignancies, thymoma occurred with such infrequency that over a 32-year period it did not warrant its own category, so fell within the ‘other/unknown’ cancer group. This only totalled 73/124 respectively from a total of 375,933 individuals with AIDS and adequate follow-up data (19).
Thymoma and other malignancies
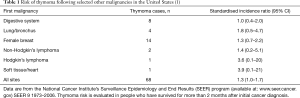
Several studies have looked at a potential link between thymoma and other malignancies, both before and after a thymoma diagnosis. Using the SEER dataset from 1973–2000, Travis et al. (2003) found a non-significant increased risk of thymoma as a second cancer, but with no clear link to a specific primary cancer (10). This was summarised in table format in the Engels et al. publication of 2010, see Table 1. However, Travis et al. did report an increased rate of malignancy following the diagnosis of thymoma, and quoted an estimated rate of 1 in 8 patients would develop an extra-thymic malignancy within 15 years (10). This result is supported by a single centre study from Taiwan, comparing patients with thymoma (n=192) with a group of patients who had a thymectomy for a non-thymoma diagnosis (n=253), and a third comparator group of patients with nasopharyngeal carcinoma treated with radiotherapy (n=1,426). They reported a rate of second malignancy in the thymoma group of 8% compared with 4% in both comparator groups (20). An association between thymoma and sarcoma, specifically malignant fibrous histiocytoma, has been reported in a cohort of 102 Japanese thymoma patients (21). However, it is not possible to draw firm causal links based on a single small study. Wilkins et al. reported a retrospective case note review of 136 thymoma patients, of whom 38 (28%) developed additional malignancies, and 14 patients had 3 or more unrelated malignancies (22). Gadalla et al. used the Swedish Cancer registry to investigate this possible link, and reported a 2-fold increased risk of second malignancy in patients with thymoma compared to the general population (23). In contrast to this, data from SEER published by Engels et al. reports no significant increased risk of subsequent malignancies except non-Hodgkins lymphoma (1,7). This may be because the patient demographics within the SEER database are slightly different to other studies, given it relies on the thymic tumour being classed as malignant, and is an older cohort. It may simply be that younger patients with more benign disease, as described in the other studies have seen more realistic trends over time. The association between thymoma and subsequent development of non-Hodgkins lymphoma is believed to be due to the disruption of T-cell function caused by either the thymoma itself or it’s treatment. It is not possible to draw an absolute conclusion, but there may well be a small increased risk of subsequent malignancies in those individuals who develop a thymoma.
Paraneoplastic and autoimmune conditions
Patients with thymomas usually present in one of three ways: with symptoms consistent with an anterior mediastinal mass (30%), with Myasthenia Gravis (40%), or as incidental findings in asymptomatic individuals (30%) (24). Of note, only 10–15% of patients with myasthenia Gravis have a thymoma. Other parathymic syndromes are seen in approximately 5% of cases and these are listed in Table 2. The commonest are hypogammaglobulinaemia, and red cell aplasia, but also frequently reported are systemic lupus erythematosus (SLE), pemphigus vulgaris, Sjogren’s syndrome and Rheumatoid arthritis (8,9,23).
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Dragana Jovanovic and Semra Bilaceroglu) for the series “Thymoma” published in Journal of Thoracic Disease. The article was sent for external peer review organized by the Guest Editors and the editorial office.
Conflicts of Interest: The author has completed the ICMJE uniform disclosure form, available at: http://dx.doi.org/10.21037/jtd-2019-thym-02. The series “Thymoma” was commissioned by the editorial office without any funding or sponsorship. The author has no other conflicts of interest to declare.
Ethical Statement: The author is accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Engels EA. Epidemiology of thymoma and associated malignancies. J Thorac Oncol 2010;5:S260-5. [Crossref] [PubMed]
- de Jong WK, Blaauwgeers JL, Schaapveld M, et al. Thymic epithelial tumours: a population-based study of the incidence, diagnostic procedures and therapy. Eur J Cancer 2008;44:123-30. [Crossref] [PubMed]
- Margaritora S, Cesario A, Cusumano G, et al. Thirty-five-year follow-up analysis of clinical and pathologic outcomes of thymoma surgery. Ann Thorac Surg 2010;89:245-52; discussion 252. [Crossref] [PubMed]
- Siesling S, van der Zwan JM, Izarzugaza I, et al. Rare thoracic cancers, including peritoneum mesothelioma. Eur J Cancer 2012;48:949-60. [Crossref] [PubMed]
- Yen YT, Lai WW, Wu MH, et al. Thymic neuroendocrine carcinoma and thymoma are both associated with increased risk of extrathymic malignancy: a 20-year review of a single institution. Ann Thorac Surg 2011;91:219-25. [Crossref] [PubMed]
- Aydiner A, Toker A, Sen F, et al. Association of clinical and pathological variables with survival in thymoma. Med Oncol 2012;29:2221-8. [Crossref] [PubMed]
- Engels EA, Pfeiffer RM. Malignant thymoma in the United States: demographic patterns in incidence and associations with subsequent malignancies. Int J Cancer 2003;105:546-51. [Crossref] [PubMed]
- Verley JM, Hollmann KH. Thymoma. A comparative study of clinical stages, histologic features, and survival in 200 cases. Cancer 1985;55:1074-86. [Crossref] [PubMed]
- Gripp S, Hilgers K, Wurm R, et al. Thymoma: prognostic factors and treatment outcomes. Cancer 1998;83:1495-503. [Crossref] [PubMed]
- Travis LB, Boice JD Jr, Travis WD. Second primary cancers after thymoma. Int J Cancer 2003;107:868-70. [Crossref] [PubMed]
- Hempelmann LH, Hall WJ, Phillips M, et al. Neoplasms in persons treated with x-rays in infancy: fourth survey in 20 years. J Natl Cancer Inst 1975;55:519-30. [Crossref] [PubMed]
- Hildreth NG, Shore RE, Dvoretsky PM. The risk of breast cancer after irradiation of the thymus in infancy. N Engl J Med 1989;321:1281-4. [Crossref] [PubMed]
- Patton DF, Ribeiro RC, Jenkins JJ, et al. Thymic carcinoma with a defective Epstein-Barr virus encoding the BZLF1 trans-activator. J Infect Dis 1994;170:7-12. [Crossref] [PubMed]
- Chen PC, Pan CC, Yang AH, et al. Detection of Epstein-Barr virus genome within thymic epithelial tumours in Taiwanese patients by nested PCR, PCR in situ hybridization, and RNA in situ hybridization. J Pathol 2002;197:684-8. [Crossref] [PubMed]
- McGuire LJ, Huang DP, Teoh R, et al. Epstein-Barr virus genome in thymoma and thymic lymphoid hyperplasia. Am J Pathol 1988;131:385-90. [PubMed]
- Manca N, Perandin F, De Simone N, et al. Detection of HTLV-I tax-rex and pol gene sequences of thymus gland in a large group of patients with myasthenia gravis. J Acquir Immune Defic Syndr 2002;29:300-6. [Crossref] [PubMed]
- Saïb A, Canivet M, Giron ML, et al. Human foamy virus infection in myasthenia gravis. Lancet 1994;343:666. [Crossref] [PubMed]
- Li H, Loehrer PJ Sr, Hisada M, et al. Absence of human T-cell lymphotropic virus type I and human foamy virus in thymoma. Br J Cancer 2004;90:2181-5. [Crossref] [PubMed]
- Engels EA, Pfeiffer RM, Goedert JJ, et al. Trends in cancer risk among people with AIDS in the United States 1980-2002. AIDS 2006;20:1645-54. [Crossref] [PubMed]
- Pan CC, Chen PC, Wang LS, et al. Thymoma is associated with an increased risk of second malignancy. Cancer 2001;92:2406-11. [Crossref] [PubMed]
- Masaoka A, Yamakawa Y, Niwa H, et al. Thymectomy and malignancy. Eur J Cardiothorac Surg 1994;8:251-3. [Crossref] [PubMed]
- Wilkins KB, Sheikh E, Green R, et al. Clinical and pathologic predictors of survival in patients with thymoma. Ann Surg 1999;230:562-72; discussion 572-4. [Crossref] [PubMed]
- Gadalla SM, Rajan A, Pfeiffer R, et al. A population-based assessment of mortality and morbidity patterns among patients with thymoma. Int J Cancer 2011;128:2688-94. [Crossref] [PubMed]
- Venuta F, Rendina EA, Anile M, et al. Thymoma and thymic carcinoma. Gen Thorac Cardiovasc Surg 2012;60:1-12. [Crossref] [PubMed]