Laparoscopic repair of Morgagni hernia by artificial pericardium patch in an adult obese patient
Introduction
Morgagni hernia is one kind of relatively rare congenital diaphragmatic hernias, which is generally asymptomatic and discovered incidentally in adulthood (1,2). Once the diagnosis of Morgagni hernia has been made clinically, surgical treatment is indicated, even in the asymptomatic cases (3,4). Here, we report an adult male patient with Morgagni hernia, who presented with non-specific gastrointestinal symptoms and underwent reduction of hernial contents followed by successfully intracorporeal suture repair of the diaphragmatic defect with artificial pericardium patch via the laparoscopic approach.
Case presentation
Patient characteristics
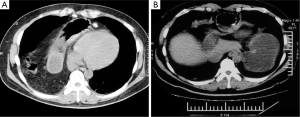
A formerly healthy, 34-year-old male obese patient was admitted to Zhongshan Hospital with chief complaints of postprandial nausea and vomiting, and accompanied by epigastric pain for 3 months. He denied blunt trauma and other risk factors for an acquired diaphragmatic hernia. The general physical examination was unremarkable except for mild deep tenderness in the epigastrium. Contrast enhanced computed tomography (CT) scan of the chest revealed that part of the stomach, transverse colon along with omentum herniated into the right pleural cavity via an anteromedial defect of the diaphragm (Figure 1). After completely clinical and imaging evaluations, the patient was planned for hernial contents reduction and diaphragmatic defect repair via the laparoscopic approach.
Surgical procedures
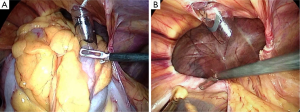
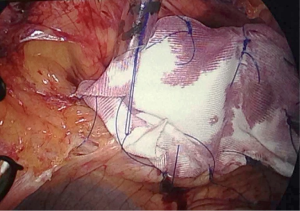
Under general anesthesia, the patient was placed in a supine position and close CO2 pneumoperitoneum (15 mmHg) was performed. One 10 mm trocar was inserted into abdominal cavity below the umbilicus for the video-laparoscope. Three additional trocars were placed in the right (one 5 mm trocar) and left (one 5 mm trocar and one 10 mm trocar) flanks, respectively. Intraoperatively, after the hernial contents (distal part of stomach, transverse colon and omentum) were gently pulled out and reduced back into the abdominal cavity, one diaphragmatic defect of measuring about 6×7 cm in size was present anterior to the right lobe of liver (Figure 2). The edge of the hernial defect was defined and the sac was not removed. As primary closure of this large diaphragmatic defect was not possible, one about 10×12 cm artificial pericardium patch was placed over the hernial defect and secured to the enough stitching margins; subsequent intracorporeal repair was performed by circumferentially interrupted sutures using 2-0 polypropylene to anchor the patch (Figure 3).
Results
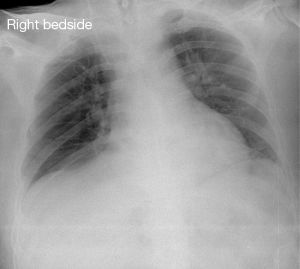
We achieved satisfactory intracorporeal repair of this large diaphragmatic defect, and postoperative chest radiography further confirmed the successfully closure of this defect (Figure 4). Recovery was uneventful, the patient was asymptomatic and started on oral diet on the first postoperative day, and then was discharged on the following day.
Discussion
The anteromedial hernia was firstly described by Giovanni-Battista Morgagni in 1761 as anatomical defect in the anterior diaphragm (5). Morgagni hernia can occur on either side of the sternum through a muscle-free triangular space, but more common on the right side (6,7). It’s reported that the peritoneal sac of almost all Morgagni hernias were well developed and herniated into the thoracic cavity; the most commonly found abdominal organs in the hernial sac were colon and omentum, less often stomach, small bowel and liver (1,8).
The patients with Morgagni hernias usually remain asymptomatic or present with vague gastrointestinal and respiratory symptoms, so most patients were diagnosed incidentally by chest X-ray until later in life (9,10). If present, the symptoms and signs are usually related to the size of the sac and contents in the hernial sac. Here, we reported a large Morgagni hernia in an adult obese patient presented with symptoms of postprandial nausea and vomiting, and accompanied by epigastric pain for 3 months. CT scan is very useful in assessing diaphragmatic hernias as it gives excellent anatomical detail on the contents of the hernia and its possible complications such as bowel obstruction or strangulation (6). CT scan of our patient showed that part of the stomach, transverse colon along with omentum herniated into the right pleural cavity, which was in accordance with the intraoperative findings.
Although complications are rare, once the diagnosis of Morgagni hernia has been made clinically, surgical repair should be performed to avoid potential intestinal obstruction and strangulation, except for those who can not tolerate surgical repair due to severe underlying diseases (4,11). Morgagni hernia can be repaired by a variety of surgical approaches including laparotomy, thoracotomy, laparoscopy and thoracoscopy, of which, the laparoscopic approach was firstly reported by Kuster et al. in 1992 (12) and has been the gold standard and the initial step for repair of non-complicated cases (11). For this patient, the hernia contents can be fully viewed and easily reduced back into abdominal cavity without incision the peritoneum at the perimeter of the defect. In addition, the hernial sac was not excised as this may result in massive pneumomediastinum with potential respiratory or circulatory complications (12). After careful assessment the extent of diaphragmatic defect, one appropriate size of artificial pericardium patch was anchored to repair this defect by circumferentially interrupted sutures using 2-0 polypropylene with intra-abdominal knotting. The patient’s excellent postoperative recovery and chest radiography well demonstrated that we have achieved satisfactory intracorporeal repair of this large diaphragmatic defect using artificial pericardium patch.
In conclusion, the review of literatures and our experience indicates that the diagnostic, therapeutic and minimally invasive advantages of laparoscopic approach offers a safe, reliable and satisfactory way to achieve the repair of non-complicated Morgagni hernia.
Acknowledgements
Funding: This work was supported by the “American Association for Thoracic Surgery’s Evarts A. Graham Memorial Traveling Fellowship”.
Disclosure: The authors declare no conflict of interest.
References
- Horton JD, Hofmann LJ, Hetz SP. Presentation and management of Morgagni hernias in adults: a review of 298 cases. Surg Endosc 2008;22:1413-20. [PubMed]
- Aydin Y, Altuntas B, Ulas AB, et al. Morgagni hernia: transabdominal or transthoracic approach? Acta Chir Belg 2014;114:131-5. [PubMed]
- Loong TP, Kocher HM. Clinical presentation and operative repair of hernia of Morgagni. Postgrad Med J 2005;81:41-4. [PubMed]
- Godazandeh G, Mortazian M. Laparoscopic Repair of Morgagni Hernia Using Polyvinylidene Fluoride (PVDF) Mesh. Middle East J Dig Dis 2012;4:232-5. [PubMed]
- Garriboli M, Bishay M, Kiely EM, et al. Recurrence rate of Morgagni diaphragmatic hernia following laparoscopic repair. Pediatr Surg Int 2013;29:185-9. [PubMed]
- Arora S, Haji A, Ng P. Adult Morgagni hernia: the need for clinical awareness, early diagnosis and prompt surgical intervention. Ann R Coll Surg Engl 2008;90:694-5. [PubMed]
- Chen Y, Wykes J, Haveman JW, et al. Laparoscopic repair of Morgagni hernia: an interesting case and complication. ANZ J Surg 2013;83:688-9. [PubMed]
- Kaida T, Ikeda A, Shimoda H, et al. Laparoscopic mesh repair of a Morgagni hernia using the double-crown technique: A case study. Asian J Endosc Surg 2014;7:323-6. [PubMed]
- Angrisani L, Lorenzo M, Santoro T, et al. Hernia of foramen of Morgagni in adult: case report of laparoscopic repair. JSLS 2000;4:177-81. [PubMed]
- Park A, Doyle C. Laparoscopic Morgagni hernia repair: how I do it. J Gastrointest Surg 2014;18:1858-62. [PubMed]
- Pironi D, Palazzini G, Arcieri S, et al. Laparoscopic diagnosis and treatment of diaphragmatic Morgagni hernia. Case report and review of the literature. Ann Ital Chir 2008;79:29-36. [PubMed]
- Kuster GG, Kline LE, Garzo G. Diaphragmatic hernia through the foramen of Morgagni: laparoscopic repair case report. J Laparoendosc Surg 1992;2:93-100. [PubMed]