
A simple and reliable method to preoperatively detect a common trunk of the left pulmonary vein
Introduction
There is a wide range of anatomical variations in the pulmonary vessels, which may cause intraoperative complications in lung cancer surgery (1-5). Confirmation of anatomic variant pulmonary vessels preoperatively based on three-dimensional and thin-section computed tomography (CT) has largely become standardized, and many variations are diagnosed successfully.
In the preoperative evaluation, anatomic variations of the pulmonary vein (PV) are also important to identify, as accidental disconnection of the PV of the lobe to be retained causes pulmonary congestion. A common trunk of the left PV is a pulmonary venous variation that can cause incorrect ligation of the drainage vein followed by massive lung edema and the need for pneumonectomy in some cases. There have been several reports on the intraoperative incorrect ligation of the left common PV (6-9) due to a lack of preoperative identification of the venous variation. Such an intraoperative accident may force surgeons to reconstruct the PV or convert lobectomy to pneumonectomy.
In general, it is difficult to detect a common trunk of the left PV by CT. Furthermore, it is quite difficult to judge whether the junction of the superior and inferior PVs is inside or outside the pericardium. Although Marom et al. reported that posterior colonal-oblique shaded-surface CT is needed in order to visualize the left common PV (10), it is difficult to perform such imaging examinations for all patients scheduled to receive lung cancer surgery. To avoid the risk of common trunk injury, the establishment of a simple and correct method of detecting a common trunk of the left PV based on a preoperative standardized examination is desired.
The purpose of the present study is to identify characteristic findings that indicate the presence of extra-pericardial common trunk of the left PV extra-pericardial in the axial view of CT and to establish the preoperative diagnostic method. We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/jtd-20-1446).
Methods
Subjects
From January 2013 to December 2017, a total of 1,615 patients underwent surgery for lung cancer at several institutions, including Nagoya City University Hospital, Suzuka Chuo General Hospital, Toyota Memorial Hospital, and Nagoya City West Medical Center. Of the 1,615 patients, 428 who underwent thin-section (1-mm collimation) chest CT preoperatively and anatomic pulmonary resection for left lung cancer were included in the present study. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). study was approved by the Institutional Review Board of Nagoya City University Graduate School of Medical Sciences (approval number: 60-18-0900).
Methods
We reviewed the medical records, CT examination findings, and surgical videos to identify a characteristic finding of a common trunk of the left PV in the axial view of chest CT. First, the patients with a left common PV were extracted based on the medical records and CT findings from Nagoya City University Hospital. Second, we checked the surgical videos and tried to determine the characteristic differences in the intraoperative findings in the hilar region between patients with and without the left common PV. We focused on the distance between the mediastinal side of the lower lobe bronchus and the junction of the superior and inferior PVs, and this finding was reflected on the axial view of the chest CT image. Finally, a thoracic surgeon (K.Y.) and a radiologist (Y.O.) with 16 and 17 years of experience, respectively, reviewed the 428 patients at the 4 institutes independently to confirm whether or not the characteristic findings could be used to diagnose common trunk. Although the CT scans were performed with different multi-detector scanners at the four institutions, the images were obtained with 1-mm collimation and a 1-mm interval and evaluated in the lung window settings. For the patients who underwent contrast-enhanced scanning, we used the contrast-enhanced images in the lung window. In the present study, the contrast-enhanced images were obtained in 414 patients among the 416 patients who were able to be evaluated.
Identification of characteristic findings
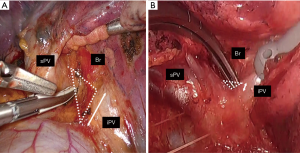
To identify characteristic findings in the axial view of chest CT, 113 patients were extracted based on the medical records and CT studies from Nagoya City University Hospital. Of these 113 patients, common trunk existed in 5 (4.4%). We then reviewed the surgical videos to search for intraoperative finding indicating common trunk. When Subcarinal lymph node dissection for left lung cancer is performed from in front of the hilum, the space surrounded by the left upper and lower PVs and the mediastinal side of the left lower bronchus is utilized for the lymph node dissection (Figure 1A). The intraoperative findings in patients with the common trunk showed that the junction of the left upper and lower PVs was quite close to the left lower bronchus, and there was almost no space surrounding them (Figure 1B). This finding was thought to be a factor supporting the detection of a common trunk in the axial view of chest CT. Based on this finding, two criteria for evaluation were set in the present study.
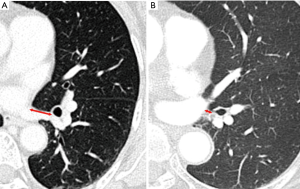
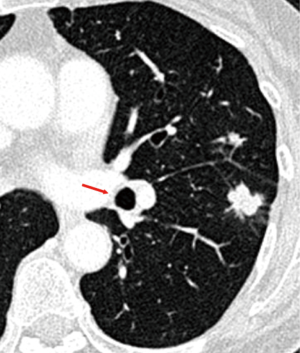
As the objective criteria, the distance between the mediastinal side of the left lower bronchus and the site where the left lower PV joins with the left atrium was measured in the axial view of CT (Figure 2A). In patients with a common trunk, the distance between the left lower bronchus and the junction of each left PV was extremely short (Figure 2B), and the axial section of the left lower bronchus was found to be close to the junction of each left PV in images (Figure 3).
As the subjective criteria, we evaluated whether an image was positive or not. In the analysis of the 113 patients at Nagoya City University Hospital, the patients with a common trunk as confirmed by surgical videos completely matched those who had been diagnosed with a common trunk by CT.
Statistical analysis
The correlation coefficient was used, and a scatter diagram was created to assess the concordance between the measured values of the two evaluators in the objective criteria. Student’s t-test was used to assess the difference in the distance between the junction of the left upper and lower PVs and the mediastinal side of the left lower bronchus in patients with and without a common trunk. A cut-off value of the distance in the objective criteria was evaluated and determined using a receiver operating characteristic (ROC) curve in each evaluator. The K statistic was used to assess the reproducibility between the two evaluators in the subjective criteria.
Results
Based on the findings in the patients from Nagoya City University Hospital, the 428 total patients from the 4 institutions were evaluated using the 2 evaluators independently. Of the 428 total patients, 256 (60%) were men. At the time of the CT examination, the mean age of the patients was 68.4 years old (range, 34–89 years old). Among the 428 patients, 12 were excluded because of another PV variation (n=8), hilar tumor invading the PV and lower bronchus (n=3), and a history of left lower lobectomy (n=1). The other PV variations included confluence of the lingular segment vein into the inferior PV or the PV of the superior segment into the superior PV.
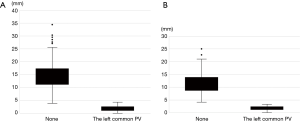
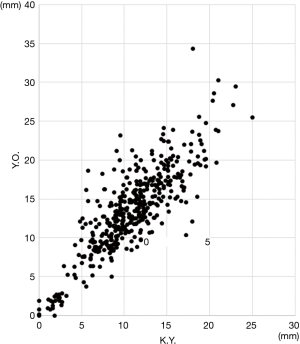
Regarding the objective criteria, the average distance between the mediastinal side of the left lower bronchus and the middle point of the confluences where each left PV joins with the left atrium was significantly shorter in the patients with a common trunk than in those without a common trunk in each evaluator (P<0.01) (Figure 4). The cut-off value of the distance measured by each evaluator was 4.3 cm (Y.O.) and 3.3 cm (K.Y.) respectively. The measured values showed an extremely strong correlation between the two evaluators, with a correlation coefficient of 0.84 (Figure 5).
Regarding the subjective criteria, as shown in Table 1, 26 patients (6.3%) were diagnosed with a common trunk of the left PV by both evaluators, although K.Y. and Y.O. diagnosed 28 and 27 patients as having a common trunk, respectively. Among the 416 patients, a diagnosis of a common trunk was coincident with in 413. The K statistic of the subjective criteria between the 2 evaluators was 0.94, which represented almost perfect agreement. The frequency of a common trunk diagnosed by both evaluators at each institution was as follows: 4.6% (5/109 patients) at Nagoya City University Hospital, 7.1% (9/126 patients) at Suzuka Chuo General Hospital, 7% (7/100 patients) at Toyota Memorial Hospital, and 6.2% (5/81 patients) at Nagoya City West Medical Center. Of the 26 patients diagnosed with a common trunk by both evaluators, 16 had surgical videos that were evaluable. Among those 16, a common trunk was confirmed in 15 (94%).

Full table
Discussion
Pulmonary vascular variation may cause surgical morbidity during anatomical pulmonary resection. Among the variations in the PVs, partial anomalous pulmonary venous connection (PAPVC) (11,12), upper venous drainage posterior to the bronchus intermedius (UVPBI) (13), and a common trunk of the left PV are important clinically because they may cause lethal complications during and after pulmonary resection due to a misunderstanding of the anatomy (6-9). However, in contrast to PAPVC and UVPBI, which can be clearly detected by CT, visualization of a common trunk using CT is considered difficult, especially in the axial view. Posterior colonal-oblique shaded-surface CT is needed in order to visualize the left common PV, as Marom et al. reported (10), and such imaging examinations are difficult to perform for all patients prior to planned lung cancer surgery.
Marom et al. (10) reported that the incidence of a common trunk is 3.5%. The frequency of a common trunk in lung cancer surgery was about 6% in the present study, which is relatively high. As skin incisions and exposure of the anatomical structure continue to decrease in both size and extent due to less-invasive surgery, intraoperative injury may occur when an anatomical anomaly is not identified preoperatively (6). With the increased frequency of robotic- or video-assisted thoracoscopic surgery in recent years (14-18), the preoperative diagnosis of the pulmonary vascular variation is becoming essential.
To avoid the risk of common trunk injury, we tried to identify characteristic findings indicating the presence of a common trunk in the axial view that can be obtained in all patients scheduled to undergo lung cancer surgery. Our results showed that when a common trunk existed, the distance between the mediastinal side of the left lower bronchus and the junction of each left PV was extremely short, and the axial section image of the left lower bronchus showed it to be close to the junction of each left PV. We considered that this finding was suitable for the diagnostic method of the common trunk.
Regarding the evaluation, the CT findings of 416 patients were reviewed independently by 2 evaluators who had different specializations. The objective criteria showed an extremely strong correlation, and the subjective criteria showed almost perfect agreement. These results suggest that this diagnostic method has high reproducibility. The present study included patients from four institutions, and the results for each institution were similar. Furthermore, this diagnostic method requires only an axial view. These findings suggest that this evaluation method can be applied for all patients scheduled to undergo lung cancer surgery. The surgical videos of the patients whom both evaluators diagnosed with a common trunk were checked to confirm the presence of a common trunk. Consequently, these surgical videos also suggested the high reliability of this diagnostic method.
In three patients, there was a discrepancy between two evaluators regarding diagnosis of a common trunk of the left PV in the subjective criteria. On the other hand, as there was a big difference of the distance between the two groups in the objective criteria, we consider that the presence of a left common PV could be determined relatively easily in most patients. However, there is a small number of patients whose measured value is on the borderline, as in the above three patients, which results in a discrepancy concerning the diagnosis according to the subjective criteria. We believe that these patients merit careful consideration of the anatomy of the left PV during surgery.
The present study has several limitations. First, the present study included only patients whose CT images had been obtained with 1-mm collimation and a 1-mm interval. Such an evaluation may be difficult in patients without thin-section CT findings, especially according to the objective criteria, because the images of the junction of each left PV becomes indistinct. In our analysis of a relatively small number of patients, the CT images of 2-mm collimation were evaluable, but those of 5-mm collimation were difficult to evaluate because of the indistinct images. Second, most of the patients (414 of 416 patients) were evaluated with the lung window settings with contrast-enhanced scanning. The left PV and left atrium were described more clearly under these conditions than would be obtained with plain CT images. In patients who undergo non-contrast-enhanced CT, the evaluation may become more difficult due to the indistinctness of the images. In the present study, for example, two patients did not undergo contrast-enhanced scanning, both of which were coincident in the evaluation. Even plain CT images may be evaluable. Finally, the diagnostic method of the present study may require some degree of experience in general thoracic surgery or radiology. In most CT studies, as the confluence of each left PV is not seen in the same image, it is necessary to search the middle point by moving the images. In the present study, two evaluators with ample experience in each of these fields conducted an independent review and obtained results that showed an extremely strong correlation with the objective criteria and almost perfect agreement with the subjective criteria. This diagnostic method is not difficult but requires an understanding of the basic regional anatomy of the chest, such as the running of the PVs or bronchi.
In conclusion, we established a method for the preoperative diagnosis of a common trunk of the left PV in the axial view on chest CT. When a common trunk exists, the distance between the mediastinal side of the left lower bronchus and the junction of each left PV is extremely short in the axial view, and the axial section of the left lower bronchus appears close to the junction of each left PV. The preoperative identification of a common trunk in the axial view can therefore be performed for all patients scheduled to undergo lung cancer surgery and is expected to be useful for ensuring safe surgical procedures.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/jtd-20-1466
Data Sharing Statement: Available at http://dx.doi.org/10.21037/jtd-20-1466
Peer Review File: Available at http://dx.doi.org/10.21037/jtd-20-1466
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jtd-20-1466). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Institutional Review Board of Nagoya City University Graduate School of Medical Sciences (approval number: 60-18-0900). Because of the retrospective nature of the study, patient informed consent or ethical statement was not required.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Endo S, Tsubochi H, Nakano T, et al. A dangerous venous variation in thoracoscopic right lower lobectomy. Ann Thorac Surg 2009;87:e9-10. [Crossref] [PubMed]
- Akiba T, Marushima H, Kamiya N, et al. Thoracoscopic Lobectomy for Treating Cancer in a Patient with an Unusual Vein Anomaly. Ann Thorac Cardiovasc Surg 2011;17:501-3. [Crossref] [PubMed]
- Shibano T, Endo S, Tetsuka K, et al. Dangerous mediastinal basal pulmonary artery during left upper lobectomy. Interact Cardiovasc Thorac Surg 2011;13:358-60. [Crossref] [PubMed]
- Shimizu K, Nagashima T, Ohtaki Y, et al. Analysis of the variation pattern in right upper pulmonary veins and establishment of simplified vein models for anatomical segmentectomy. Gen Thorac Cardiovasc Surg 2016;64:604-11. [Crossref] [PubMed]
- Fourdrain A, De Dominicis F, Bensussan M, et al. Three-dimensional computed tomography angiography of the pulmonary veins and their anatomical variations: involvement in video-assisted thoracoscopic surgery-lobectomy for lung cancer. Folia Morphol (Warsz) 2017;76:388-93. [Crossref] [PubMed]
- Nakamura T, Koide M, Nakamura H, et al. The common trunk of the left pulmonary vein injured incidentally during lung cancer surgery. Ann Thorac Surg 2009;87:954-5. [Crossref] [PubMed]
- Endo T, Tetsuka K, Yamamoto S, et al. Transection of left common pulmonary vein during left upper lobectomy: how should it be reconstructed? J Surg Case Rep 2012;2012:rjs030.
- Seok Y, Lee E. Inadvertently transected left superior pulmonary vein during thoracoscopic left lower lobectomy. J Cardiothorac Surg 2016;11:84. [Crossref] [PubMed]
- Asouhidou I, Karaiskos T, Natsis K. Pulmonary vein anatomical variation during videothoracoscopy-assisted surgical lobectomy. Surg Radiol Anat 2017;39:229-31. [Crossref] [PubMed]
- Marom EM, Herndon JE, Kim YH, et al. Variations in pulmonary venous drainage to the left atrium: implications for radiofrequency ablation. Radiology 2004;230:824-9. [Crossref] [PubMed]
- Black MD, Shamji FM, Goldstein W, et al. Pulmonary resection and contralateral anomalous venous drainage: a lethal combination. Ann Thorac Surg 1992;53:689-91. [Crossref] [PubMed]
- Sakurai H, Kondo H, Sekiguchi A, et al. Left pneumonectomy for lung cancer after correction of contralateral partial anomalous pulmonary venous return. Ann Thorac Surg 2005;79:1778-80. [Crossref] [PubMed]
- Asai K, Urabe N, Yajima K, et al. Right upper lobe venous drainage posterior to the bronchus intermedius: preoperative identification by computed tomography. Ann Thorac Surg 2005;79:1866-71. [Crossref] [PubMed]
- Upham TC, Onaitis MW. Video-assisted thoracoscopic surgery versus robot-assisted thoracoscopic surgery versus thoracotomy for early-stage lung cancer. J Thorac Cardiovasc Surg 2018;156:365-8. [Crossref] [PubMed]
- Louie BE, Wilson JL, Kim S, et al. Comparison of video-assisted thoracoscopic surgery and robotic approaches for clinical stage I and stage II non-small cell lung cancer using the Society of Thoracic Surgeons Database. Ann Thorac Surg 2016;102:917-24. [Crossref] [PubMed]
- Whitson BA, Groth SS, Duval SJ, et al. Surgery for early-stage non-small cell lung cancer: a systemic review of the video-assisted thoracoscopic surgery versus thoracotomy approaches to lobectomy. Ann Thorac Surg 2008;86:2008-16; discussion 2016-8.
- Yan TD, Black D, Bannon PG, et al. Systematic review and meta-analysis of randomized and non randomized trials on safety and efficacy of video-assisted thoracic surgery lobectomy for early-state non-small cell lung cancer. J Clin Oncol 2009;27:2553-62. [Crossref] [PubMed]
- Swanson SJ, Meyers BF, Gunnarsson CL, et al. Video-assisted thoracoscopic lobectomy is less costly and morbid than open lobectomy: a retrospective multi institutional database analysis. Ann Thorac Surg 2012;93:1027-32. [Crossref] [PubMed]


