
Preliminary experimental outcomes of induced hypercapnia in treatment of obstinate singultus
Introduction
Our team discovered that subjecting the body to acute hypercapnia creates the physiological conditions necessary to stop singultus, or hiccups (1,2). The partial pressure of CO2 in arterial blood must reach no less than 50mmHg and the CO2 pressure gradient between arterial and venous blood must disappear almost completely to be effective (1,2). In order to investigate these conditions precisely, we had a combination gas consisting of 10% CO2 and 90% O2 made for patients to inhale, aiming to create the above conditions instantly and safely; we thought that if patients continued breathing in the gas, their CO2 pressure in blood should constantly increase from normal level to about 70 mmHg within a few minutes. If the gas successfully ceased their hiccups, the precise target to stop them would be revealed. Incidentally, according to our former report, a CO2 pressure gradient between venous-arterial blood should be found until CO2 pressure in arterial blood is below around 50 mmHg, and after that point the pressure gradient should be abolished (1,2). We report the preliminary experimental outcomes of treatment for chronic singultus using induced hypercapnia and discuss the next step forward regarding treatment. We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/jtd-20-1049).
Methods
The study protocol was examined and approved by our institutional review board (Institutional Review Board of St. Mary’s Hospital; No. 16-1010 and No. 19-0606, approved on Oct. 31, 2016 and Jun. 30, 2019, respectively). Clinical trial No. was UMIN000037704 and registered on August 17, 2019. This study was registered as UMIN000037704 on August 17, 2019 and was conducted in accordance with the Helsinki Declaration (as revised in 2013).
Participants
From August 2019 to March 2020, a total of 26 patients with long-term intractable singultus were treated with the combination gas at our institution. All patients agreed to participate in our study to stop singultus using the gas, and written informed consent was obtained from the participants. The group consisted of 21 males and 5 females with a mean age of 70.0±12.8 years (Table 1), and the mean duration of hiccups was 8.0±13.1 years, with a range of 5 days to 66 years. All patients had undergone numerous treatments, both home remedies and standard medications (such as injection of metoclopramide), with no lasting effect. It is worth noting that all patients who requested treatment at our institution during this time were included in the study and are presented in consecutive order in the data tables.
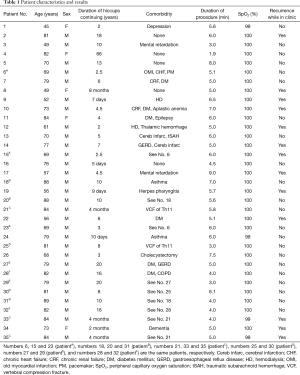
Full table
Materials
The combination gas consisting of 10% CO2 and 90% O2 was ordered through a gas company (Kyushu Air Water) in Kumamoto Prefecture, Japan. A standard oxygen mask was used for delivery of the combination gas to the patient, whose head was completely covered with a 45 L (650×800 mm2) clear plastic bag (Figure 1). An airtight seal was made around the neck using plastic tape in order to prevent the gas from escaping into the atmosphere and reducing the effectiveness of the procedure. To prevent the plastic bag from clinging to the nostrils or mouth, patients wore a baseball cap or a hat with a wide brim.

Procedure
After the oxygen mask, hat, and plastic bag were fully in place, we administered the combination gas to each patient at a rate of 2–6 L/min, paying attention to overpressure inside the bag. Patients were instructed to continue breathing normally inside the bag until they felt their singultus stop. A pulse oximeter was used to continuously monitor the peripheral capillary oxygen saturation (SpO2) and heart rate (HR) of the patients, for their safety.
The duration of the procedure was measured from the beginning to the point at which singultus ceased. If patients agreed, a blood test was performed to measure the partial pressure of CO2 in venous blood at the point at which singultus ceased, and also before the procedure. Incidentally, according to our previous study, we regarded CO2 pressure in arterial blood as almost the same value as that in venous blood when they were over 50 mmHg (2).
Results
A total of 35 cases consisting of 26 consecutive patients with persistent or intractable singultus were treated with the combination gas. The group consisted of 21 males and 5 females, and the mean duration of singultus was 8.0±13.1 years (mean ± SD). We administered the combination gas to each patient. Singultus was successfully stopped in all patients in a mean time of 5.3±1.5 minutes. In 13 of the 35 cases, recurrence occurred while in the clinic, and the same procedures were re-performed; the second treatments were also effective in those cases. In patient No.2 and No.34, however, singultus restarted a few minutes after the procedure again and again. Patient No.2 agreed to 4 subsequent attempts, and patient No.34 did 2 attempts, but none resulted in long-term relief in both patients. Life-threatening complications were not found in any patient.
The blood test was performed in 23 cases (consisting of 20 patients) of the 35 cases; the mean partial pressure of CO2 in the venous blood at the point the singultus stopped was 60.8±6.8 mmHg, whereas that before the procedure was 46.8±6.7 mmHg. The mean HR at the beginning of the procedure was 75.9±13.0 bpm and at the time hiccups stopped was 89.3±14.9 bpm (17.7% increase). Incidentally, all data was collected at the first trial of each case.
Discussion
Singultuses are involuntary movements triggered from afferent signals such as through the glossopharyngeal nerve, vagus nerve, phrenic nerve and sympathetic nerves (T6–T12), and involve rapid inspiration and sudden closing of both the vocal cords and epiglottis (3-6). Since the movements are related to the innervation areas of the phrenic nerves and vagus nerve, it is presumed that the “hiccup epicenter” is located near the nucleus tractus solitarii in the medulla (1-3). Sudden contraction of the diaphragm generates strong negative pressure in the air tract, and air aspirated through the narrow space between the vocal cords as they slam shut creates the high-pitch ‘hic’ noise we know as a hiccup (3,4).
Although the nature of singultus is still a mystery (3,4), it has been believed since ancient times that CO2 retention in the body should lead singultus to stop (7). In fact, many researchers have studied about it using paper-bag rebreathing and CO2 inhalation; CO2 affects the central nervous system (CNS) and ceases singultus, although the precise mechanism has not been completely revealed as of yet (5-8). According to historical evidence, it is thought that CO2 has some potential to cut the circuit of singultus in the CNS (7,8). On this ground, treatment using CO2 would possibly be a radical therapy for singultus (7). Unfortunately, however, methods such as paper-bag rebreathing are still considered to be home remedies, even now (4,6). Probably because of their unstable reproducibility, it may well be difficult for many physicians to take them seriously as a standard therapy (8).
As mentioned in our previous report (1), our team thought that the unstable reproducibility of CO2 retention methods was probably caused by an insufficient level of CO2 in the body, especially in the CNS. According to Petroianu, modest concentration of CO2 in the body can explain the limited success of paper-bag rebreathing therapies for singultus (8). For CO2 concentrations in patients to be a reliable treatment option, PaCO2 should increase, for example from 40 to 50 mmHg, so as to sufficiently decrease the pH in the CNS to suppress excitability of the respiratory center (8). From this point of view, our method increased PaCO2 so steadily from 40 to around 70 mmHg that excitability of the CNS was able to be sufficiently suppressed to cease persistent or intractable singultus in all of our patients. In our previous reports, singultus stopped in hypercapnia when the venous-arterial CO2 gradient was abolished; it occurred when PaCO2 reached no less than 50 mmHg. The present study more precisely revealed that it occurs around 60 mmHg, even though the precise point was different in each patient. In theory, our method can always reach and pass the threshold point, which is between about 50 and 76 mmHg. That is the reason for being able to successfully calm CNS excitability in order to cease singultus.
Although our team has some speculations about possible mechanisms, one of which is activation of fight-or-flight response (9), the actual mechanism of how CO2 retention can terminate singultus effectively using our method is still a difficult question. Further investigation and cooperation with other researchers are necessary to reveal this mystery completely.
Nonetheless, our team found several interesting facts through this experimental treatment. Firstly, our team can provide mental relief for patients because many of them believed that their singultus would never cease by such treatments. Despite the fact that the effect did not always last for a long period, they realized that there is at least one reliable method to instantly stop singultus at their will. In fact, a few patients with intractable singultus returned to the hospital to stop it again from time to time when they were annoyed by the recurrence. We are confident that the certainty and reliability of our treatment can often relieve patients’ psychological burden. Secondly, we have realized that the restarting mechanism is the actual mystery of singultus. We thought that singultus problems would be resolved for good if only we could simply stop the hiccups. Actually, however, hiccups often recurred in patients with chronic singultus, in the same way that arrhythmia sometimes recurs after being successfully terminated using a defibrillator. It is crucial to find the “ignition” that restarts the singultus circuit. Lastly, other researchers can easily conduct conformation experiments, as our results demonstrated that the threshold to stop singultus was around 60 mmHg of PaCO2 as well as PvCO2. To the best of our knowledge, there was no report with even 26 patients with persistent or intractable singultus, and where singultus was successfully stopped in all cases, even only temporarily. We believe that this number demonstrates that our method is highly promising. It is our sincere hope that many researchers will join this field and refine our method and theory.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/jtd-20-1049
Data Sharing Statement: Available at http://dx.doi.org/10.21037/jtd-20-1049
Peer Review File: Available at http://dx.doi.org/10.21037/jtd-20-1049
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jtd-20-1049). TO reports he has a patent null pending. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study protocol was examined and approved by our institutional review board (Institutional Review Board of St. Mary’s Hospital; No. 16-1010 and No. 19-0606, approved on Oct. 31, 2016 and June 30, 2019, respectively). Clinical trial No. was UMIN000037704 and registered on August 17, 2019. This study was registered as UMIN000037704 on August 17, 2019 and was conducted in accordance with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the participants.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Obuchi T, Shimamura S, Miyahara N, et al. CO2 Retention: The key to Stopping Hiccups. Clin Respir J 2018;12:2340-5. [Crossref] [PubMed]
- Obuchi T, Wakahara J, Fujimura N, et al. Medullar impairment resolves hiccups. J Thorac Dis 2018;10:3622-6. [Crossref] [PubMed]
- Chang FY, Lu CL. Hiccup: mystery, nature and treatment. J Neurogastroenterol Motil 2012;18:123-30. [Crossref] [PubMed]
- Kohse EK, Hollmann MW, Bardenheuer HJ, et al. Chronic Hiccups: An Underestimated Problem. Anesth Analg 2017;125:1169-83. [Crossref] [PubMed]
- Oshima T, Sakamoto M, Arita H. Hiccuplike response elicited by mechanical stimulation of dorsal epipharynx of cats. J Appl Physiol 1994;76:1888-95. [Crossref] [PubMed]
- Rouse S, Wodziak M. Intractable Hiccups. Curr Neurol Neurosci Rep 2018;18:51. [Crossref] [PubMed]
- Petroianu GA. Singultus, paper-bag ventilation, and hypercapnia. J Hist Neurosci 2020;29:286-98. [Crossref] [PubMed]
- Petroianu GA. Abolishing the venous-arterial CO2 gradient as treatment for singultus: Commentary on Obuchi et al. (2018). Clin Respir J 2019;13:408-9. [Crossref] [PubMed]
- Petroianu GA. Treatment of hiccup by vagal maneuvers. J Hist Neurosci 2015;24:123-36. [Crossref] [PubMed]


