
Staged repair of chronic type A aortic dissection with small true lumen at the descending aorta
Introduction
Chronic type A aortic dissection is a common disease owing to the following circumstances: (I) aortic dissection after previous cardiovascular surgery, (II) dilatation of the aorta distal to the aortic graft after successful surgical treatment of acute type A dissection using only ascending aortic replacement, and (III) delayed diagnosis and surgical treatment in patients with acute type A dissection (1-3). However, it is a life-threatening event associated with formidable mortality. The surgical treatment of chronic type A dissection is yet challenging, especially for patients with small true lumen at the descending aorta due to compression of the fibrotic and rigid chronic dissection intimal membrane. Although several surgical procedures have been developed (3-5), the patients of chronic type A dissection with small true lumen at the descending aorta require further innovative surgical techniques.
Total arch replacement (TAR) combined with stented elephant trunk (SET) implantation for type A dissection was found to be an optimal approach in surgical treatment (6). However, the advantage of this operation is impaired by the size limitation of the SET within the treatment for patients with small true lumen at the descending aorta. In this study, we reviewed our experience of the two-stage procedure for the repair of chronic type A dissection with small true lumen at the descending aorta. We present the following article in accordance with the STROBE guideline checklist (available at http://dx.doi.org/10.21037/jtd-20-1048).
Methods
Patient data
A total of seven patients (including 6 males), aged 40.4±11.5 (range, 21–53) years, with chronic type A dissection with small true lumen at the descending aorta underwent the two-stage procedure between February 2016 and December 2019. Five patients who initially presented progressive dyspnea were referred to Changhai Hospital, and the other 2 suffered mild chest pain. Marfan syndrome occurred in 5/7 (71.4%) patients. Aortic root aneurysm with severe aortic valve insufficiency was found in three cases. Preoperative computed tomographic angiography (CTA) was performed to carefully assess the diameter of the descending aorta, tear site, and visceral arteries. The major tear site was located at the ascending aorta in three patients, at the transverse arch in three patients, and at the proximal descending thoracic aorta in two patients. All the patients had multiple tears at the distal descending aorta. Interestingly, CTA of 5/7 patients showed that visceral arteries stem from both false lumen and true lumen (Table 1).
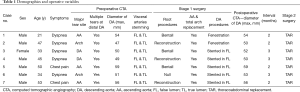
Full table
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by the Ethics Committee of Changhai Hospital affiliated to Second Military Medical University (Number: CHCS012016). All patients enrolled completed the informed consent form.
Technique
According to preoperative CTA and intraoperative exploration, the true lumen of the descending aorta was extremely small, and a suitable SET could not be implanted (Figure 1A). Thus, we adopted a two-stage procedure. The first stage of ascending aorta and TAR using a tetrafurcate graft was performed in all patients via a median sternotomy under cardiopulmonary bypass (CPB) with selective cerebral perfusion (SCP). The cannulation of the right axillary artery was carried out routinely for CPB and SCP. Furthermore, CPB and cooling were started after the cannulation of the right axillary artery and the right atrium. Aortic root procedures were performed (if necessary) after cross-clamping the ascending aorta and cardioplegia. A circulatory arrest was established when the nasopharyngeal temperature reached 27 °C, the ascending aorta and aortic arch were opened, and the tear site was resected whenever possible. The proximal descending aorta was transected circumferentially distal to the origin of the left subclavian artery or distal to the intimal tear in the proximal descending aorta. Because the true lumen of the descending thoracic aorta was extremely small, no suitable SET could be implanted. Therefore, open fenestration of the proximal descending chronic dissection flap was performed during the intraoperative view of the selective antegrade brain perfusion in two cases. In addition, the length of the septum excised was typically about 3–4 cm. After fenestration, a Dacron graft (about 2–3 cm length and the size same as tetrafurcate graft) was inserted into the true lumen at the descending thoracic aorta. In the remaining five cases, a 10-cm-long stent graft was inserted into the false lumen of the descending thoracic aorta (Figure 1B). Then, the anastomosis between the tetrafurcate graft and the descending aorta was effectuated by the open aortic technique.
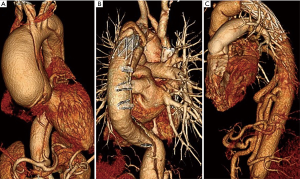
All patients have received the second stage operation, which was like standard descending thoracic or thoracic abdominal replacement after 2–3 months of the first-stage procedure. The left heart bypass was performed from the pulmonary vein to the common femoral artery. With a clamp at the proximal descending thoracic aorta, the distal of the SET or Dacron graft inserted in the descending thoracic aorta during the first stage was grasped. A new graft was sutured to the elephant trunk or the Dacron graft (Figure 1C).
Results
All patients of chronic type A dissection with a small true lumen of the descending aorta underwent TAR in the first stage using a tetrafurcate graft. The concomitant procedures included Bentall in three cases and aortic root reconstruction in three cases.
All patients underwent first- and second-stage procedures. No mortality was detected among the seven patients. One patient who had a transient neurological deficit after the first stage recovered completely before hospital discharge. In two patients, the diameter of the descending aorta was enlarged postoperatively after the first-stage procedure. The interval between the two procedures was 2–3 months. Subsequently, no adverse events, such as stroke, paraparesis, visceral malperfusion, and lower extremity malfunction were observed.
Discussion
Although several surgical procedures have been developed for chronic type A dissection (3-5), the optimal technique for the treatment of chronic type A dissection with small true lumen at the descending aorta is not yet established.
The primary objective of the surgical treatment of type A dissection is to save the life of the patient. The adaptable and efficient method is to apply a conservative procedure of replacement of ascending aorta or combined with hemiarch replacement. A high incidence of dilatation of either distal aorta or residual dissection is observed in addition to a high prevalence of reoperation (7). In order to avoid readmitting sternotomy and facilitate the performance of reintervention after proximal aortic surgery, TAR with an elephant trunk was recommended for staged aortic replacement in patients with chronic type A dissection (8). Strikingly, placing the conventional elephant trunk in the small true lumen in patients with chronic type A dissection is difficult because the true lumen is compressed by the false lumen. Consequently, complications, including kinking and obstruction of the graft, embolization, and paraplegia, have been observed (8). Therefore, the SET procedure initiated by Sun et al. obtained an encouraging outcome (6). In comparison to the conventional elephant trunk technique, the SET (which is in a bound, compressed state) could be easily applied to the true lumen of the distal aorta under direct vision. Also, compared to the procedure described by Kouchoukos et al. (4) that an “arch-first” procedure and bilateral anterior thoracotomy incision to treat chronic type A dissection, the SET procedure effectively avoided scathe forgoing of the internal thoracic arteries and significantly reduced the prevalence of pulmonary complications. However, the limitation of the SET procedure is that it does not exist in the formatted size for the patient who has chronic type A dissection with a small true lumen at the descending aorta. A potential risk of kinking and obstruction of the graft might induce visceral malperfusion and lower extremity malfunction, which cannot be neglected when an oversize SET is implanted into a very small true lumen. Furthermore, the SET is not optimal when the diameter of the descending aorta is >50 mm (3).
In our group of patients of chronic type A dissection with small true lumen at the descending aorta, preoperative CTA showed that the diameter of descending aorta was >50 cm (mean 5.2 cm) in 5/7 cases. During intraoperative exploration, we found that the true lumen of the descending aorta was extremely small, and no suitable SET could be implanted. To address this issue, we adopted a two-stage procedure. Two patients with visceral arteries stemming from the true lumen underwent open fenestration of the proximal descending chronic dissection flap procedure. Subsequently, a Dacron graft (about 2–3 cm length and the size same as a tetrafurcate graft) was inserted into the true lumen of the descending thoracic aorta. The advantage of the fenestration procedure is that it facilitates perfusion of both channels, and the hemodynamics is similar to that of preoperation. No injury to the spinal cord and organ malperfusion were detected. Since a Dacron graft was reserved in the true lumen of the descending aorta in the first-stage, several options are available in the two-stage procedure, such as standard descending thoracic or thoracic, abdominal replacement, or endovascular placement of a stent-graft for certain groups of patients and high-risk patients. Five patients whose CTA showed that visceral arteries stemming from both false lumen and true lumen and multiple tears at the distal descending aorta, received a 10-cm-long stent-graft implantation into the false lumen at the descending thoracic aorta directly. In this group, no injury to the spinal cord and organ malperfusion were observed. The true lumen existed in the downstream aorta distal to the end of the surgical stent. Both lumens (true and false) were perfused. Sun et al. (9) used SET implantation to treat type A dissection, and found some cases wherein the distal end of the stent-graft entered the false lumen unplanned. Because of the extremely tortuous morphology of the false lumen, the intimal layer might be torn during implantation of the SET. However, no organ malperfusion was found. Therefore, in the event of multiple tears at the distal descending aorta, directly implanting the stent-graft into the false lumen may be safe. Furthermore, applying the SET into the enlarged false lumen of the distal aorta under direct vision is easy. Additionally, the stented graft was 10-cm long and posed a technical challenge in the two-stage procedure. The potential risk of this procedure is rapid aneurysmal dilatation or rupture of the residual descending aorta. Although deaths caused by rupture of the remaining aortic aneurysm in the interval between the two-stage procedures have been reported (10), chronic descending aortic dissection may have a lower incidence of rupture than true aneurysm. In centers utilizing this procedure, the interval between the two procedures was 4.9±7.5 months (11). Therefore, the interval between the two procedures is determined by the condition of the patients’ recovery and illustration of postoperative CTA after the first stage procedure. If the CTA shows that the diameter of the descending aorta is >5.5 cm and the patient has a good recovery, the second stage procedure should be performed promptly.
Taken together, the two-staged procedure for the repair of chronic type A dissection with small true lumen at the descending aorta is adaptable, as it has a low prevalence of morbidity and complication in our study group.
Acknowledgments
Funding: The study was funded by the National Natural Science Foundation of China (Grant No. 81870344).
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/jtd-20-1048
Data Sharing Statement: Available at http://dx.doi.org/10.21037/jtd-20-1048
Peer Review File: Available at http://dx.doi.org/10.21037/jtd-20-1048
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jtd-20-1048). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by the Ethics Committee of Changhai Hospital affiliated to Second Military Medical University (Number: CHCS012016). All patients enrolled completed the informed consent form.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Hirose H, Svensson LG, Lytle BW, et al. Aortic dissection after previous cardiovascular surgery. Ann Thorac Surg 2004;78:2099-105. [Crossref] [PubMed]
- Heinemann M, Laas J, Karck M, et al. Thoracic aortic aneurysms after acute type A aortic dissection: necessity for follow-up. Ann Thorac Surg 1990;49:580-4. [Crossref] [PubMed]
- Sun LZ, Qi RD, Chang Q, et al. Is total arch replacement combined with stented elephant trunk implantation justified for patients with chronic Stanford type A aortic dissection? J Thorac Cardiovasc Surg 2009;138:892-6. [Crossref] [PubMed]
- Kouchoukos NT, Masetti P, Rokkas CK, et al. Single-stage reoperative repair of chronic type A aortic dissection by means of the arch-first technique. J Thorac Cardiovasc Surg. 2001;122:578-82. [Crossref] [PubMed]
- Hu XP, Chang Q, Zhu JM, et al. One-stage total or subtotal aortic replacement. Ann Thorac Surg 2006;82:542-6. [Crossref] [PubMed]
- Sun L, Qi R, Zhu J, et al. Total arch replacement combined with stented elephant trunk implantation: a new "standard" therapy for type a dissection involving repair of the aortic arch? Circulation 2011;123:971-8. [Crossref] [PubMed]
- Girdauskas E, Kuntze T, Borger MA, et al. Distal aortic reinterventions after root surgery in Marfan patients. Ann Thorac Surg 2008;86:1815-9. [Crossref] [PubMed]
- Crawford ES, Coselli JS, Svensson LG, et al. Diffuse aneurysmal disease (chronic aortic dissection, Marfan, and mega aorta syndromes) and multiple aneurysm. Treatment by subtotal and total aortic replacement emphasizing the elephant trunk operation. Ann Surg 1990;211:521-37. [Crossref] [PubMed]
- Sun L, Li M, Zhu J, et al. Surgery for patients with Marfan syndrome with type A dissection involving the aortic arch using total arch replacement combined with stented elephant trunk implantation: the acute versus the chronic. J Thorac Cardiovasc Surg 2011;142:e85-91. [Crossref] [PubMed]
- Safi HJ, Miller CC 3rd, Estrera AL, et al. Staged repair of extensive aortic aneurysms: morbidity and mortality in the elephant trunk technique. Circulation 2001;104:2938-42. [Crossref] [PubMed]
- LeMaire SA, Carter SA, Coselli JS. The elephant trunk technique for staged repair of complex aneurysms of the entire thoracic aorta. Ann Thorac Surg 2006;81:1561-9; discussion 1569. [Crossref] [PubMed]


