Screening for pectus excavatum among primary students and establishment of a pectus excavatum screening program in Dongguan, China
Introduction
Pectus excavatum (PEx) is the most common congenital deformity of the anterior wall of the chest, in which the third to the seventh ribs cave in towards the inner side of the rib-cartilage conjunction or towards the spine. This produces a funnel appearance of the chest (1). Bauhinus first described PEx in the 16th century, and another documented description of an appearance of the thorax could be found in 1860 by Woillez. In 1863, von Luschka (2) reported about a 6-cm deep depression in the thorax wall of a 24-year-old man. In 1870, Eggel (3) published the first comprehensive case report of a patient with a funnel-formed thorax depression calling it a ‘miraculum naturae’. Meyer performed the first operation of PEx in 1911 with the removal of the rib cartilage. In 1998, a non-invasive way to correct PEx without the need for extensive costal cartilage resection or sternal osteotomy was proposed by Nuss; since then, the Nuss procedure has been widely applied because it is minimally invasive and can achieve a natural post operative appearance. It has become a preferred procedure for repairing PEx in developed countries (4).
The incidence of PEx ranges between 1 and 8 per 1,000 persons (2), in particular among children younger than 12 years. Interestingly, males are more often affected, with a gender distribution between 2:1 and 9:1 (3,5). PEx is mainly believed to be caused by congenital factors, showing autosomal dominant inheritance. The prevalence rate of PEx is 2.5‰ among individuals with a family history but is only 1‰ among those without any family history of PEx. The symptoms of PEx patients become progressively worse with age; they often exist at birth, and will be identified by parents months or years later (6). The common symptoms and hazards of PEx are often multi-faceted: (I) physical impacts: in patients with mild PEx, the caved-in posterior edge of the sternum does not compress the heart, and thus the heart and lung functions will not be seriously affected. In patients with severer PEx, however, the caved-in chest wall decreases the volume of the pleural cavity and suppresses the expansion of the lung. In particular, the lung expansion is restricted during the inhaling and the respiratory resistance is increased (7), resulting in the recurrent upper respiratory tract infections. The shrunken pleural cavity restricts the cardiac activities, leading to the decrease in cardiac output (8). The patients may suffer from palpitation, shortness of breath, difficulty breathing, and other symptoms during physical activities; (II) psychological impacts: PEx patients tend to experience mental disorders such as sense of inferiority, sense of shame, social disorder, autism, and depression, which may be further exacerbated with age and thus seriously affect the patients' physical and mental health (9).
Surgical correction of the the depressed sternum remains the main treatment for PEx, and the common procedures include Ravitch procedure and Nuss procedure (4,10,11). These procedures are mainly applied in patients with moderate or severe PEx, and the operation must be completed before puberty (12,13).
Although the Nuss procedure has been applied in clinical settings for decades, many PEx patients have not been identified or treated. The deformity of PEx progressive worsens along with the growth/development and its adverse impacts on the physical and mental statues of the children become increasingly obvious. Too often the treatment during the puberty has already missed the best chance and can not achieve the expected efficacy, resulting in life-long regrets. However, studies on PEx have been focused on its radiological diagnosis and surgical interventions and, to our knowledge, no study have reported the screening for PEx. Therefore, it is necessary to establish a sophisticated screening program to identify the prevalence of PEx among middle and primary school students, so as to facilitate the early diagnosis and follow-up of PEx patients. Also, it is important to train a group of qualified medical staff in school infirmaries so that they are able to detect the suspected cases and help the patients to receive Nuss procedure in time.
In our current study, by carrying our well-organized screening, we tried to learn the status of PEx among pupils in Dongguan, Guangdong Province, particularly the prevalence of PEx and its epidemiological distribution; meanwhile, by providing training for medical staff in the school infirmaries, we tried to establish a highly efficient PEx screening program and network in Dongguan and help the patients to receive the minimally invasive Nuss procedure in time. This project will remarkably improve the diagnosis and management of PEx among pupils in Dongguan primary schools and then fosters a considerate environment for the growth of this population.
Patients and methods
It was planned to carry out PEx screening among 479,402 primary school students who were already in school in 2012 or newly enrolled in 2013 from 422 primary schools in 31 towns in Dongguan, Guangdong Province. The name, gender, age, date of birth, school, class, and telephone number as well as the date of recording and the name of recorder were recorded. Meanwhile, we also carried out three 2-day workshops for 410 medical staff from these primary schools, so as to establish a screening network that enables the early diagnosis and follow-up of the PEx children and the reporting of the results to the Dongguan Health Bureau. Thus, a PEx screening network and early diagnosis program were established.
Statistical analysis
Statistical analyses were performed with commercially available software (SPSS 16.0 for Windows, SPSS, Inc., Chicago, IL, USA). Pearson chi-square test and independent t-test were used to compare categorical and numerical data, respectively. The level of statistical significance was set as P<0.05.
Results
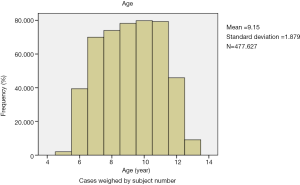
Valid screening results were obtained from 477,627 pupils (99.62%) from 406 primary schools in 31 towns. Some students did not participate in this survey due to illness/private affair leave, suspension of schooling, and/or refusal by the school to participate. These students aged 4-15 years (mean: 8.78 years), among whom there were 244,545 males (N1; mean age: 8.22 years) and 233,082 females (N2; mean age: 8.89 years) (Figure 1).
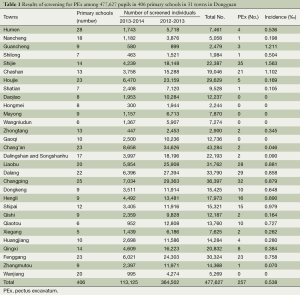
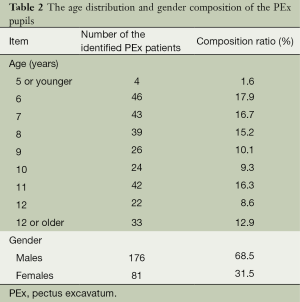
Totally 257 PEx patients were identified, yielding a prevalence of 0.583%, among whom there were 176 males (N3; mean age: 8.79 years) and 81 females (N4; mean age: 8.77 years) (Tables 1,2).
Full table
Full table
The PEx patients as the PEx group (males: 176; females: 81) and the healthy children as the control group (males: 244,369; females: 233,001), chi square test with gender as the dependent variable showed that the incidence of PEx was significantly different between male and female students (χ2=30.739, P<0.001).
Meanwhile, with an attempt to establish PEx screening network, we also carried out three 2-day workshops for 410 medical staff from the 406 primary schools in 31 towns in Dongguan. The training contents included the history and clinical presentations of PEx and the recent advances in the management of this disease. All the 410 trainees successfully passed the examinations, which included a written test and a practical test (the medical staff were asked to diagnose the newly enrolled students in 2013, and the results were reviewed by thoracic surgeons).
Discussion
PEx is the most common chest wall deformity, accounting for more than 90% of all chest wall deformities. It is featured by the funnel-shaped depression of the anterior chest wall (centered on xiphoid) caused when the lower portion of the sternum and its corresponding costal cartilages are abnormally pushed inward. Previously, the most authoritative reports on PEx were authored by Nuss and Kelly and published in the Journal of Pediatric Surgery in 1998 and 2005, respectively (2,4). In the first article, Nuss et al. calculated the incidence of PEx during the period 1987-1996 based on the thoracic malformation patients who had undergone surgeries during this period. In the second article, Kelly et al. collected the autopsy data of the dead newborns in the past 112 years (from 1889 to 2001), and calculated the incidence of PEx based on the samples with chest wall deformities.
In our current study, we investigated the incidence of PEx among 477,627 pupils from 406 primary schools in 31 towns in Dongguan. It was the first prevalence survey targeting a specific age group in a specific area; compared with the previous retrospective studies, our current study included all the PEx cases among pupils in Dongguan and provided these patients with early treatment; meanwhile, our study accurately described the regional and age distributions of the PEx cases.
A total of 257 PEx patients were identified in our current study, yielding a prevalence rate of 0.583%. The Shijie Town had the highest incidence (35/22,387, I=1.563‰), while no PEx case was found in six towns (Daojiao, Hongmei, Machong, Wangniudun, Gaobu, and Wansongshan). The prevalence rate of PEx in our study was lower than those reported in literature, which ranged 1-4‰ (1-4).
Such a low prevalence rate may be explained by the following reasons: (I) study design: as a cross-sectional study, our study was targeted at all the pupils in Dongguan city. According to the previous literature, due to the features of bone development, young PEx patients have softer bones and longer costal cartilages, and the optimal ages for the surgical treatment of PEx are 3-12 years, particularly at 6-8 years (14). For adolescents and adults whose bones have gradually became fully developed, surgical treatment such as the Nuss procedure can be associated with poor outcomes such as increased post-operative complications due to the increased use of steel bars and incisions and poor effectiveness. It has been reported that complications such as pneumothorax and pleural effusion were found in up to 60% of patients after the Nuss procedure if the surgery was performed in adolescents and adults older than 18 years (15-20). Therefore, from the perspective of surgical feasibility, we did not include PEx patients who were older than 15 years into this study; (II) sample collection: due to the economic conditions and family reasons, some children living in rural areas in Dongguan are not enrolled in primary schools. These PEx children were also enrolled in our current study; (III) regional differences: many studies in China and abroad have found that the incidences of chest wall deformities (including PEx) have regional differences (21,22). Meanwhile, the incidence of PEx has shown certain correlation with the neonatal nutritional diseases such as rickets. Some authors even argued that PEx was a key sign of the congenital infantile rickets (23). As a relatively developed coastal city in China, Dongguan has established sophisticated systems for perioperative care for newborns, children care, and children nutrition; thus, the incidences of chest deformities have dramatically dropped.
In our current study, the PEx patients aged 4-15 years (mean: 8.782 years); among them there were 176 males (mean age: 8.79 years) and 81 females (mean age: 8.77 years). The age group with the largest patient number was 6-7 years (totally 46 persons). The age of PEx patients were not normally distributed. This may be because PEx is a progressive disease that is related to aging. It often exists at birth but is found by the patient’s parents months or years later as the disease progresses (24). The caved-in sternum has already became quite obvious at presentation, which has already long after its occurrence. Therefore, the identification age of PEx patients can not represent the onset age. Furthermore, since the parents themselves could not clearly deduce or describe the exact onset age of PEx, we could not track back the onset time of the PEx. Determination of the bone alkaline phosphatase (BALP) activity in pregnant women and neonates has shown that the increased BALP activity was significantly correlated with the occurrence of chicken breast or PEx in newborns (25).
Of the 257 PEx patients, there were 176 males (68.5%) and 81 females (31.5%), with a male/female ratio of 2.172:1. Among the non-PEx patients, there were 244,369 males (51.2%) and 233,001 females (48.8%). The PEx patients were assigned as the PEx group, and the non-PEx patients as the control group. Chi square test with the gender as the dependent variable showed that the incidence of PEx was significantly different between males and females (χ2=30.739, P=0.00). Such a gender difference was consistent with the findings of previous retrospective studies, which showed the male/female ratios ranged 2:1-9:1 (3).
No foreign or domestic study has well investigated such a difference. Our current cross-sectional study also could not convincingly explain the why the incidence of PEx was higher in males than in females. The specific etiology of PEx remains unclear. In 2012, Wurtza et al. proposed that PEx is mainly due to congenital factors, showing autosomal dominant inheritance. The prevalence rate of PEx is 2.5‰ among individuals with a family history but is only 1‰ among those without any family history of PEx. In a typical PEx patient, the costal cartilage abnormally grows or elongates at birth or during puberty, along with forward or backward displacement and deformation (26). A Chinese study also compared the incidence of PEx between patients with a family history and those without a family history and found that 10-20% of the pediatric patients had a definite family history (5). However, Wurtza et al. also did not make a reasonable explanation for why the incidence of PEx was higher in males than in females from the perspective of genetics. In our opinion, this may be because the gene sequencing technique was not sophisticated enough at that time. Today we are already in an era of “Big Data”. The human genome atlas has already successfully drawn, and the specific gene loci can be drawn by accurate gene sequencing techniques. Our cross-sectional study provided a solid information network for future genetic studies on PEx. Meanwhile, with an attempt to establish PEx screening network, we also carried out three 2-day workshops for 410 medical staff from the 406 primary schools in 31 towns in Dongguan. By doing so, we successfully formed a screening network and trained a medical team for the early diagnosis and monitoring of PEx, which provided the technical and personal supports for the early diagnosis and treatment of PEx in Dongguan.
This PEx screening network can provide physical examination for the newly enrolled pupils in Dongguan and thus facilitate the early diagnosis and early treatment of students with obvious PEx symptoms. Surgical correction of the depressed sternum remains the main treatment for PEx, and the common procedures include Ravitch procedure and Nuss procedure (4,10,11). These procedures are mainly applied in patients with moderate or severe PEx, and the operation must be completed before puberty (12,13). Thus, the early screening of PEx is closely associated with the possibility of a curative surgery. The PEx screening network established in our study can maximize the surgery success rate and thus provide an information assurance for the early eradication of PEx symptoms.
Second, this network can effectively follow up the already identified PEx patients and carry out focused monitoring of the potential PEx among their children, which enables the early prevention of PEx among the kids and the further genetic studies on the etiology of PEx.
Third, by comparing the genetic information of the PEx patients identified through the screening and the normal subjects, we may further identify the genetic sequences that govern the pathogenesis of PEx and thus cure PEx using genetic techniques such as gene knockout.
Our current study had some limitations: (I) limited by the developmental features of PEx, our current study did not include all the PEx patients in Dongguan—children who were not enrolled in primary schools and adolescent or adult PEx patients were missed from our analysis, thus, we were not able to carry out a descriptive statistics on the prevalence and incidence of PEx in Dongguan; (II) due to the limitations in the research advances both in China and abroad, our study neither described the etiology of PEx nor explored its risk factors; (III) restricted by the examination conditions, we were not able to carry out on-site measurement of the HI index for the PEx patients. Instead, we only recorded the severity of PEx when the patients were sent to hospitals for a surgery. Thus, our data on the disease severity may not be available for some cases.
Our subsequent studies may include: (I) we will describe items including the surgery duration, hospitalization time, correction effectiveness, incidences of post-operative complications, and surgery costs, with an attempt to establish the Nuss procedure-centered guidelines on the management of PEx, which may help to include the Nuss procedure in the health insurance system in China and thus benefit more PEx patients; (II) we will carry out long-term follow-up studies on the screened PEx patients, so as to further identify the genetic features of PEx and analyze the genetic data that may explain its etiology.
In our current study, we investigated the incidence of PEx among 477,627 pupils from 406 primary schools in 31 towns in Dongguan. A total of 257 PEx patients were identified in our current study, yielding a prevalence rate of 0.583% among the pupils in Dongguan. Of the 257 PEx patients, there were 176 males (68.5%) and 81 females (31.5%), with a male/female ratio of 2.172:1. The age distribution and regional distribution of these PEx cases were irregular. Meanwhile, with an attempt to establish PEx screening network, we also carried out three workshops for 410 medical staff. By doing so, we successfully formed a screening network and trained a medical team for the early diagnosis and monitoring of PEx, which provided the technical and personal supports for the early diagnosis and treatment of PEx in Dongguan.
Acknowledgements
Funding: This study was supported by the Dongguan Health Bureau 2012 (Grant Number: 2012105102029).
Disclosure: The authors declare no conflict of interest.
References
- Hu YZ. Congenital chest wall deformities. Journal of Clinical Pediatric Surgery 2009;8:60-3.
- Von Luschka H. Die Anatomie des Menschen in Rücksicht auf die Bedürfnisse der praktischen Heilkunde. Die Anatomie der Brust des Menschen. Tübingen: Laupp, 1863:23.
- Eggel. Eine seltene Mißbildung des Thorax. Virchows Arch Path Anat 1870;49:230.
- Nuss D, Kelly RE Jr, Croitoru DP, et al. A 10-year review of a minimally invasive technique for the correction of pectus excavatum. J Pediatr Surg 1998;33:545-52. [PubMed]
- Li J. History and clinical impacts of pectus excavatum. Clinical Medical & Engineering 2013;20:507-8.
- Jiang XP, Hu ZT, Liu WY, et al. Long-term follow-up of lung functions after the correction of pectus excavatum. Chinese Journal of Pediatric Surgery 1999;20:222-4.
- Hu YZ, Wei FK, Luo QC, et al. Sternal elevation operation on pectus excavatum: report of 6 cases. Chinese Journal of Pediatric Surgery 1987;8:341.
- Wang QH, Yang YJ, Wei KL, et al. Epidemiological survey on newborns born at the obstetric departments in hospitals in mid-southern region of China in 2005. Transl Pediatr 2013;2:21-26.
- Liu WY, Yuan YR, Hu YZ, et al. Pulmonary Function in Children with Pectus Excavatum. Chinese Journal of Pediatric Surgery 1992;13:86-8.
- Jaroszewski D, Notrica D, McMahon L, et al. Current management of pectus excavatum: a review and update of therapy and treatment recommendations. J Am Board Fam Med 2010;23:230-9. [PubMed]
- Laituri CA, Garey CL, St Peter SD. Review of the technical variants in the repair of pectus excavatum. Eur J Pediatr Surg 2010;20:217-21. [PubMed]
- Hu ZT. Surgical treatment of pectus excavatum: 30-years experience in 406 patients. Chinese Journal of Pediatric Surgery 2005;26:393-5.
- Snel BJ, Spronk CA, Werker PM, et al. Pectus excavatum reconstruction with silicone implants: long-term results and a review of the english-language literature. Ann Plast Surg 2009;62:205-9. [PubMed]
- Yu S, Hu YG, Fang Y, et al. Selection of surgical procedures for pectus excavatum. Chinese Journal of Pediatric Surgery 2005;26:404.
- Guo SY, Cui CY. Surgical ages for pectus excavatum and the outcomes. Central Plain’s Medical Journal 2002;29:19-20.
- Nuss D, Croitoru DP, Kelly RE Jr, et al. Review and discussion of the complications of minimally invasive pectus excavatum repair. Eur J Pediatr Surg 2002;12:230-4. [PubMed]
- Leonhardt J, Kübler JF, Feiter J, et al. Complications of the minimally invasive repair of pectus excavatum. J Pediatr Surg 2005;40:e7-9. [PubMed]
- Park HJ, Lee SY, Lee CS. Complications associated with the Nuss procedure: analysis of risk factors and suggested measures for prevention of complications. J Pediatr Surg 2004;39:391-5; discussion 391-5. [PubMed]
- Croitoru DP, Kelly RE Jr, Goretsky MJ, et al. Experience and modification update for the minimally invasive Nuss technique for pectus excavatum repair in 303 patients. J Pediatr Surg 2002;37:437-45. [PubMed]
- Park HJ, Lee SY, Lee CS, et al. The Nuss procedure for pectus excavatum: evolution of techniques and early results on 322 patients. Ann Thorac Surg 2004;77:289-95. [PubMed]
- Goretsky MJ, Kelly RE Jr, Croitoru D, et al. Chest wall anomalies: pectus excavatum and pectus carinatum. Adolesc Med Clin 2004;15:455-71. [PubMed]
- Liu WY. Diagnosis and surgical correction of pectus excavatum and pectus carinatum. Journal of Applied Clinical Pediatrics 2012;27:889-92.
- Qiao J, Feng HL. Assisted reproductive technology in China: compliance and non-compliance. Transl Pediatr 2014;3:91-7.
- Sang S, Wu MJ, Lu FQ. Advances in the diagnosis and treatment of congenital pectus excavatum. Journal of Taishan Medical College 2013;34:557-60.
- Xin HY. Role of bone alkaline phosphatase determination in the early diagnosis of infantile rickets. Chinese Medical Digest(Pediatrics) 2013;(4):2-3.
- Wurtz A, Rousse N, Benhamed L, et al. Simplified open repair for anterior chest wall deformities. Analysis of results in 205 patients. Orthop Traumatol Surg Res 2012;98:319-26. [PubMed]


