Single incision thoracoscopic lobectomy through a 2.5 cm skin incision
Introduction
Single incision thoracoscopic surgery (SITS) involves only one intercostal space with minimal skin incision, which means it can be the most minimally invasive surgery up to date. SITS has been mainly used for simple thoracic procedures since the first application by Rocco in 2000 (1). The advancement of surgical techniques and instruments led to the introduction of SITS lobectomy by Gonzalez in 2011 (2). Several clinical series demonstrated that SITS lobectomy had similar efficacy to 3-port video-assisted thoracic surgery (VATS) lobectomy (3,4). However, reports in the literature on SITS lobectomy were almost exclusively devoted to the treatment of lung cancers. Unlikely lung cancer surgery, SITS lobectomy for benign pulmonary disease has advantage for extracting the lobar specimen from a small incision and no need for mediastinal lymph node (LN) dissection.
We report our experience of four patients treated with SITS lobectomy for benign pulmonary disease through a minimal skin incision.
Clinical summary
Case 1
A 50-year-old female patient was planned to undergo SITS left lower lobe (LLL) lobectomy for recurrent pneumonia due to bronchiectasis.
Case 2
A 12-year-old boy admitted to the emergency department with left sided chest pain and was subsequently diagnosed with left spontaneous pneumothorax and underwent closed thoracostomy. The high resolution computed tomography showed congenital lobar emphysema of the left upper lobe (LUL) and the patient was planned to undergo SITS LUL lobectomy due to a persistent air leak.
Case 3
A 52-year-old female patient was diagnosed with a fungus ball in the right upper lobe (RUL) and was under observation for 2 years. She developed recurrent hemoptysis and was planned to undergo SITS RUL lobectomy.
Case 4
A healthy 34-year-old female was detected with a 1.4 cm sized, well-demarcated round mass in the RUL central portion during routine health screening 2 years ago. The size of the thought-to-be benign tumor increased to 1.7 cm during the follow-up and was suspected with low grade malignancy. The patient was planned to undergo SITS RUL lobectomy directly due to the location of mass instead of limited resection (Table 1).
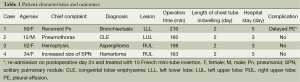
Full table
Surgical technique
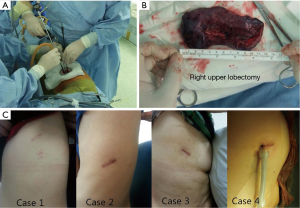
Under general anesthesia, the patients were intubated with double lumen endotracheal tube and placed in the lateral decubitus position. Pre-emptive wound infiltration with 0.5% bupivacaine was used for pain relief. A 2.5 cm single incision was made in the mid axillary line of the 5th intercostal space and the wound protector was set up. A 5.5 mm, 30˚ thoracoscope with a working length of 45 cm (HD5530XL, ConMed Linvatec, Largo, FL, USA) was used. The long and thin shaft of the scope helped to minimize collision of the instruments and allowed the placement of various other instruments in the small port. The flexible single incision laparoscopic surgery (SILS)TM HOOK (Covidien®, Mansfield, MA, USA) was used in patients with pleural adhesion for convenient adhesiolysis. The fissure was separated through a central approach to expose the interlobar pulmonary artery (PA) first, and the branches of the PA were divided from anterior to the posterior direction. The pulmonary vein and the lobar bronchus were divided using the endoscopic stapler. The specimens were placed in the retrieval bag for extraction. For case 1 and 3, the specimens were divided into 4-5 pieces within the bag and retrieved in parts (Figure 1). For case 2 and 4, the specimens were retrieved as a whole without injury (Figure 2). A 24 French chest tube was placed on the posterior part of the wound (Figure 3). There were no conversion cases to multi-port VATS or thoracotomy. The mean operation time was 182±25 minutes. Chest drains were removed on postoperative day (POD) 2 in all patients. Three patients discharged on POD 3. One patient who discharged on POD 5 readmitted for delayed pleural effusion and treated with mini-tube insertion. There were no late complications or symptom relapses during the median follow-up of 13.5 months.


Discussion
SITS has been used by some thoracic surgeons in the past few years and different techniques have been published for application in various thoracic diseases (3,4,7,8). Several reports have shown that SITS causes less incisional pain, less paresthesia and higher satisfaction regarding the wound scar compared to the 3-port VATS (9,10). However, most of these merits were based on wedge resection for pneumothorax patients treated through a 2.5 cm single incision. For SITS lobectomy, there has been no scientific evidence on the benefit of SITS compared to 3-port VATS lobectomy. However, we hypothesized that minimizing the chest wall trauma would be beneficial to patients when inferring from the previous comparative studies between SITS and 3-port VATS. We identified a potential to reduce the wound size to the 2.5 cm using the thin, long, curved or flexible instruments with 5 mm long working length videoscope. This is the minimum size of the incision that allows the placement of the endoscopic stapler, the 5 mm videoscope, and the 5 mm endograsper instrument together under the current technical aspects. Surgical indication for 2.5 cm SITS lobectomy was patients with benign pulmonary disease rather than lung cancer. The benign pulmonary disease does not need LN dissection and the specimen does not need to be removed as a whole. In this study, one patient had a lung mass of 1.7 cm which could potentially be cancerous, but we conducted 2.5 cm SITS lobectomy because she was very young and such malignancy was likely to be of low grade.
There was one case of bleeding during the division of the branch of the PA. The bleeding was controlled using a gelatin and thrombin based matrix (Floseal®; Baxter Inc, Deerfield, IL, USA) without additional incision.
It took more operation time compared to conventional VATS lobectomy (mean: 182±25 minutes; range: 160-210 minutes). However, this is a case report for only four patients. We believe that with the accumulation of cases, this may be able to overcome. From the other point of view, among of them, three patients (case 1, 2, and 3) had fusion fissure or hilar inflammation due to underlying disease characteristics (see Figures 1 and 2). Despite of these fusion fissures, chest drains were removed on POD 2 in all patients. This was possible because of the slow and careful dissection of the fissure and meticulous air leak control in the stage of air leak test. Actually, the process that was most time-consuming during 2.5 cm SITS lobectomy was adjusting the angle of stapling. The development of a thinner stapler with maximum angulation of 90° will significantly reduce the operation time.
In order to apply a 2.5 cm SITS lobectomy for lung cancer, the size of the tumor should be less than 2 cm. In addition, the flexible energy device and the curved vessel retractor for tissue dissection will be helpful for complete LN dissection. There should be further study on the new and safe extraction method without tumor cell spillage for cases where specimen is difficult to extract as a whole.
Conclusions
A 2.5 cm SITS lobectomy can be mainly applied to benign lung disease where there is no need for LN dissection and no concerns for tumor cell spillage. The development of long and thin curved instruments, flexible instruments, and thin endoscopic staplers with better flexibility will allow reduction in the size of the wound and operation time.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Rocco G, Martin-Ucar A, Passera E. Uniportal VATS wedge pulmonary resections. Ann Thorac Surg 2004;77:726-8. [PubMed]
- Gonzalez D, Paradela M, Garcia J, et al. Single-port video-assisted thoracoscopic lobectomy. Interact Cardiovasc Thorac Surg 2011;12:514-5. [PubMed]
- Gonzalez-Rivas D, Paradela M, Fernandez R, et al. Uniportal video-assisted thoracoscopic lobectomy: two years of experience. Ann Thorac Surg 2013;95:426-32. [PubMed]
- Wang BY, Tu CC, Liu CY, et al. Single-incision thoracoscopic lobectomy and segmentectomy with radical lymph node dissection. Ann Thorac Surg 2013;96:977-82. [PubMed]
- Yang HC, Noh D. Single port left lower lobectomy for bronchiectasis (case 1: specimen was divided into 4-5 pieces within the bag). Asvide 2015;2:043. Available online: http://www.asvide.com/articles/499
- Yang HC, Noh D. Single port left upper lobectomy for congenital lobar emphysema (case 2: specimen was extracted as a whole without injury). Asvide 2015;2:044. Available online: http://www.asvide.com/articles/500
- Chen CH, Lee SY, Chang H, et al. Technical aspects of single-port thoracoscopic surgery for lobectomy. J Cardiothorac Surg 2012;7:50. [PubMed]
- Song IH, Yum S, Choi W, et al. Clinical application of single incision thoracoscopic surgery: early experience of 264 cases. J Cardiothorac Surg 2014;9:44. [PubMed]
- Jutley RS, Khalil MW, Rocco G. Uniportal vs standard three-port VATS technique for spontaneous pneumothorax: comparison of post-operative pain and residual paraesthesia. Eur J Cardiothorac Surg 2005;28:43-6. [PubMed]
- Yang HC, Cho S, Jheon S. Single-incision thoracoscopic surgery for primary spontaneous pneumothorax using the SILS port compared with conventional three-port surgery. Surg Endosc 2013;27:139-45. [PubMed]


